User login
It’s not an assembly line
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A lot of businesses benefit from being in private equity funds.
Health care isn’t one of them, and a recent report found that
This really shouldn’t surprise anyone. Such funds may offer glittering phrases like “improved technology” and “greater efficiency” but the bottom line is that they’re run by – and for – the shareholders. The majority of them aren’t going to be medical people or realize that you can’t run a medical practice like it’s a clothing retailer or electronic car manufacturer.
I’m not saying medicine isn’t a business – it is. I depend on my little practice to support three families, so keeping it in the black is important. But it also needs to run well to do that. Measures to increase revenue, like cutting my staff down (there are only two of them) or overbooking patients would seriously impact me effectively doing my part, which is playing doctor.
You can predict pretty accurately how long it will take to put a motor and bumper assembly on a specific model of car, but you can’t do that in medicine because people aren’t standardized. Even if you control variables such as same sex, age, and diagnosis, personalities vary widely, as do treatment decisions, questions they’ll have, and the “oh, another thing” factor.
That doesn’t happen at a bottling plant.
In the business model of health care, you’re hoping revenue will pay overhead and a reasonable salary for everyone. But when you add a private equity firm in, the shareholders also expect to be paid. Which means either revenue has to go up significantly, or costs have to be cut (layoffs, short staffing, reduced benefits, etc.), or a combination of both.
Regardless of which option is chosen, it isn’t good for the medical staff or the patients. Increasing the number of people seen in a given amount of time per doctor may be good for the shareholders, but it’s not good for the doctor or the person being cared for. Think of Lucy and Ethyl at the chocolate factory.
Even in an auto factory, if you speed up the rate of cars going through the assembly line, sooner or later mistakes will be made. Humans can’t keep up, and even robots will make errors if things aren’t aligned correctly, or are a few seconds ahead or behind the program. This is why they (hopefully) have quality control, to try and catch those things before they’re on the road.
Of course, cars are more easily fixable. When the mistake is found you repair or replace the part. You can’t do that as easily in people, and when serious mistakes happen it’s the doctor who’s held at fault – not the shareholders who pressured him or her to see patients faster and with less support.
Unfortunately, this is the way the current trend is going. The more people who are involved in the practice of medicine, in person or behind the scenes, the smaller each slice of the pie gets.
That’s not good for the patient, who’s the person at the center of it all and the reason why we’re here.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Buyer beware
The invitation came to my house, addressed to “residential customer.” It was for my wife and me to attend a free dinner at a swanky local restaurant to learn about “revolutionary” treatments for memory loss. It was presented by a “wellness expert.”
Of course, I just had to check out the website.
The dinner was hosted by an internist pushing an unproven (except for the usual small noncontrolled studies) treatment. Although not stated, I’m sure when you call you’ll find out this is not covered by insurance; not Food and Drug Administration approved to treat, cure, diagnose, prevent any disease; your mileage may vary, etc.
The website was full of testimonials as to how well the treatments worked, primarily from people in their 20s-40s who are, realistically, unlikely to have a pathologically serious cause for memory problems. The site also mentions that you can use it to treat traumatic brain injury, ADHD, learning disorders, obsessive-compulsive disorder, PTSD, Parkinson’s disease, autism, dementia, and stroke, though it does clearly state that such use is not FDA approved.
Prices (I assume all cash pay) for the treatment weren’t listed. I guess you have to come to the “free” dinner for those, or submit an online form to the office.
I’m not going to say the advertised treatment doesn’t work. It might, for at least some of those things. A PubMed search tells me it’s under investigation for several of them.
But that doesn’t mean it works. It might, but a lot of things that look promising in early trials end up failing in the long run. So, at least to me, this is no different than people selling various over-the-counter supplements online with all kinds of extravagant claims and testimonials.
I also have to question a treatment targeting young people for memory loss. In neurology we see a lot of that, and know that true pathology is rare. Most of these patients have root issues with depression, or anxiety, or stress that are affecting their memory. That doesn’t make their memory issues any less real, but they shouldn’t be lumped in with neurodegenerative diseases. They need to be correctly diagnosed and treated for what they are.
Maybe it’s just me, but I often see this sort of thing as kind of sketchy – generating business for unproven treatments by selling fear – you need to do something NOW to keep from getting worse. And, of course there’s always the mysterious “they.” The treatments “they” offer don’t work. Why aren’t “they” telling you what really does?
Looking at the restaurant’s online menu, dinners are around $75 per person and the invitation says “seats are limited.” Doing some mental math gives you an idea how many diners need to come, what percentage of them need to sign up for the treatment, and how much it costs to recoup the investment.
Let the buyer beware.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The invitation came to my house, addressed to “residential customer.” It was for my wife and me to attend a free dinner at a swanky local restaurant to learn about “revolutionary” treatments for memory loss. It was presented by a “wellness expert.”
Of course, I just had to check out the website.
The dinner was hosted by an internist pushing an unproven (except for the usual small noncontrolled studies) treatment. Although not stated, I’m sure when you call you’ll find out this is not covered by insurance; not Food and Drug Administration approved to treat, cure, diagnose, prevent any disease; your mileage may vary, etc.
The website was full of testimonials as to how well the treatments worked, primarily from people in their 20s-40s who are, realistically, unlikely to have a pathologically serious cause for memory problems. The site also mentions that you can use it to treat traumatic brain injury, ADHD, learning disorders, obsessive-compulsive disorder, PTSD, Parkinson’s disease, autism, dementia, and stroke, though it does clearly state that such use is not FDA approved.
Prices (I assume all cash pay) for the treatment weren’t listed. I guess you have to come to the “free” dinner for those, or submit an online form to the office.
I’m not going to say the advertised treatment doesn’t work. It might, for at least some of those things. A PubMed search tells me it’s under investigation for several of them.
But that doesn’t mean it works. It might, but a lot of things that look promising in early trials end up failing in the long run. So, at least to me, this is no different than people selling various over-the-counter supplements online with all kinds of extravagant claims and testimonials.
I also have to question a treatment targeting young people for memory loss. In neurology we see a lot of that, and know that true pathology is rare. Most of these patients have root issues with depression, or anxiety, or stress that are affecting their memory. That doesn’t make their memory issues any less real, but they shouldn’t be lumped in with neurodegenerative diseases. They need to be correctly diagnosed and treated for what they are.
Maybe it’s just me, but I often see this sort of thing as kind of sketchy – generating business for unproven treatments by selling fear – you need to do something NOW to keep from getting worse. And, of course there’s always the mysterious “they.” The treatments “they” offer don’t work. Why aren’t “they” telling you what really does?
Looking at the restaurant’s online menu, dinners are around $75 per person and the invitation says “seats are limited.” Doing some mental math gives you an idea how many diners need to come, what percentage of them need to sign up for the treatment, and how much it costs to recoup the investment.
Let the buyer beware.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The invitation came to my house, addressed to “residential customer.” It was for my wife and me to attend a free dinner at a swanky local restaurant to learn about “revolutionary” treatments for memory loss. It was presented by a “wellness expert.”
Of course, I just had to check out the website.
The dinner was hosted by an internist pushing an unproven (except for the usual small noncontrolled studies) treatment. Although not stated, I’m sure when you call you’ll find out this is not covered by insurance; not Food and Drug Administration approved to treat, cure, diagnose, prevent any disease; your mileage may vary, etc.
The website was full of testimonials as to how well the treatments worked, primarily from people in their 20s-40s who are, realistically, unlikely to have a pathologically serious cause for memory problems. The site also mentions that you can use it to treat traumatic brain injury, ADHD, learning disorders, obsessive-compulsive disorder, PTSD, Parkinson’s disease, autism, dementia, and stroke, though it does clearly state that such use is not FDA approved.
Prices (I assume all cash pay) for the treatment weren’t listed. I guess you have to come to the “free” dinner for those, or submit an online form to the office.
I’m not going to say the advertised treatment doesn’t work. It might, for at least some of those things. A PubMed search tells me it’s under investigation for several of them.
But that doesn’t mean it works. It might, but a lot of things that look promising in early trials end up failing in the long run. So, at least to me, this is no different than people selling various over-the-counter supplements online with all kinds of extravagant claims and testimonials.
I also have to question a treatment targeting young people for memory loss. In neurology we see a lot of that, and know that true pathology is rare. Most of these patients have root issues with depression, or anxiety, or stress that are affecting their memory. That doesn’t make their memory issues any less real, but they shouldn’t be lumped in with neurodegenerative diseases. They need to be correctly diagnosed and treated for what they are.
Maybe it’s just me, but I often see this sort of thing as kind of sketchy – generating business for unproven treatments by selling fear – you need to do something NOW to keep from getting worse. And, of course there’s always the mysterious “they.” The treatments “they” offer don’t work. Why aren’t “they” telling you what really does?
Looking at the restaurant’s online menu, dinners are around $75 per person and the invitation says “seats are limited.” Doing some mental math gives you an idea how many diners need to come, what percentage of them need to sign up for the treatment, and how much it costs to recoup the investment.
Let the buyer beware.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
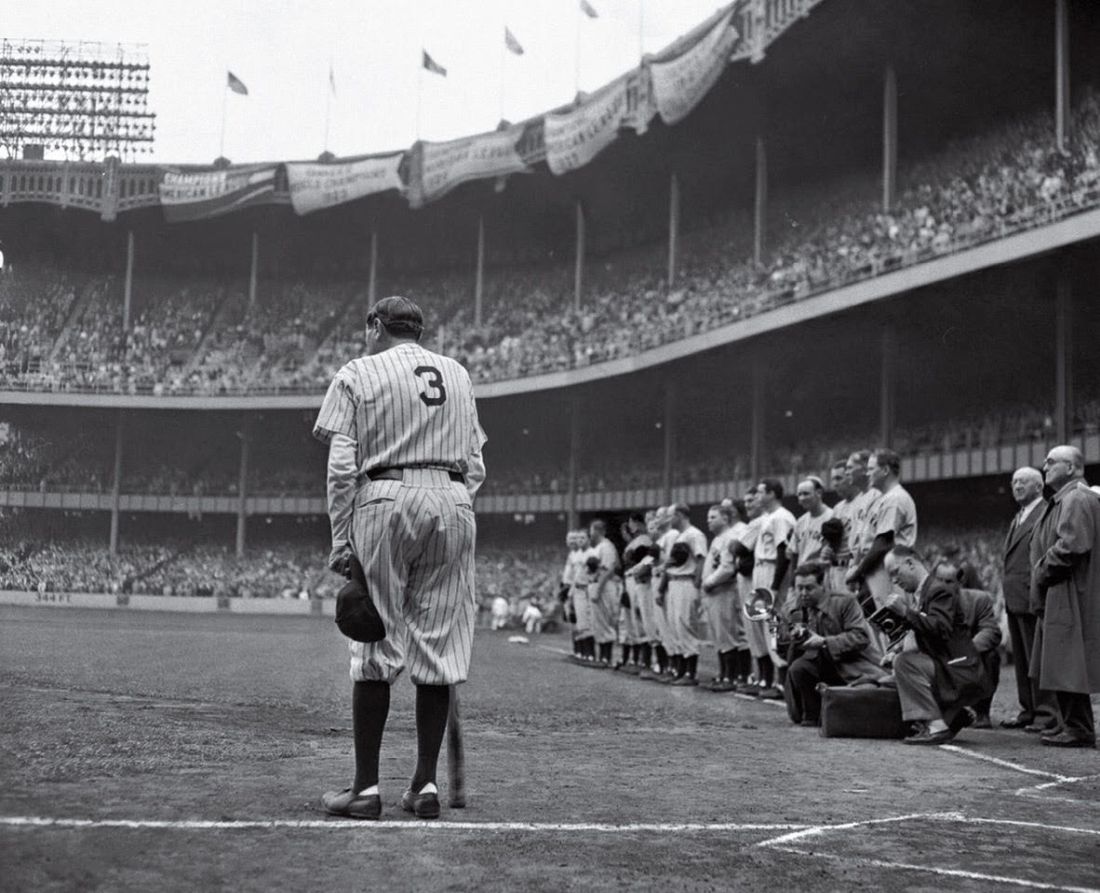
Babe Ruth’s unique cane, and why he used it
Babe Ruth was arguably the greatest athlete in American history.
Certainly, there have been, and always will be, many great figures in all sports. But none of them – Michael Jordan or LeBron James or Tom Brady – have ever, probably will never, dominate sports AND society in the way Babe Ruth did.
Ruth wasn’t an angel, nor did he claim to be. But he was a center of American life the way no athlete ever was or will be.
He was a remarkably good baseball player. In an era where home runs were rarities, he hit more than the entire rest of Major League Baseball combined. But he wasn’t just a slugger, he was an excellent play maker, fielder, and pitcher. (He was actually one of the best pitchers of his era, something else mostly forgotten today.)
Ruth retired in 1935. He never entirely left the limelight, with fans showing up even to watch him play golf in celebrity tournaments. In 1939 he spoke on July 4 at Lou Gehrig appreciation day as his former teammate was publicly dying of ALS.
In 1946 Ruth began having trouble swallowing and developed pain over his right eye. He was found to have nasopharyngeal carcinoma spreading down into his skull base and neck.
Even today surgery to remove cancer from that area is tricky. In 1946 it didn’t exist. An experimental treatment of combined radiation and chemotherapy – today standard – was tried, including a new folic acid derivative called teropterin. He improved somewhat – enough that he was an unnamed case study presented at a medical meeting – but had lost 80 pounds. After a brief respite he continued to go downhill. On June 13, 1948, he appeared at Yankee Stadium – the house that Ruth built – for the last time, where he was honored. He had difficulty walking and used a baseball bat as a cane. His pharynx was so damaged his voice could barely be heard. He died 2 months later on Aug. 16, 1948.
This isn’t a sports column, I’m not a sports writer, and this definitely ain’t Sport Illustrated. So why am I writing this?
Because Babe Ruth never knew he had cancer. Was never told he was dying. His family was afraid he’d harm himself if he knew, so his doctors were under strict instructions to keep the bad news from him.
Now, Ruth wasn’t stupid. Wild, unrepentant, hedonistic, and a lot of other things – but not stupid. He certainly must have figured it out with getting radiation, or chemotherapy, or his declining physical status. But none of his doctors or family ever told him he had cancer and was dying (what they did tell him I have no idea).
Let’s look at this as a case history: A 51-year-old male, possessed of all his mental faculties, presents with headaches, dysphonia, and dysphagia. Workup reveals advanced, inoperable, nasopharyngeal cancer. The family is willing to accept treatment, but understands the prognosis is poor. Family members request that, under no circumstances, he be told of the diagnosis or prognosis.
The fact that the patient is probably the biggest celebrity of his era shouldn’t make a difference, but it does.
I’m sure most of us would want to tell the patient. We live in an age of patient autonomy. . But what if the family has concerns that the patient would hurt himself, as Ruth’s family did?
This summer is 75 years since the Babe died. Medicine has changed a lot, but some questions never will.
What would you do?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Babe Ruth was arguably the greatest athlete in American history.
Certainly, there have been, and always will be, many great figures in all sports. But none of them – Michael Jordan or LeBron James or Tom Brady – have ever, probably will never, dominate sports AND society in the way Babe Ruth did.
Ruth wasn’t an angel, nor did he claim to be. But he was a center of American life the way no athlete ever was or will be.
He was a remarkably good baseball player. In an era where home runs were rarities, he hit more than the entire rest of Major League Baseball combined. But he wasn’t just a slugger, he was an excellent play maker, fielder, and pitcher. (He was actually one of the best pitchers of his era, something else mostly forgotten today.)
Ruth retired in 1935. He never entirely left the limelight, with fans showing up even to watch him play golf in celebrity tournaments. In 1939 he spoke on July 4 at Lou Gehrig appreciation day as his former teammate was publicly dying of ALS.
In 1946 Ruth began having trouble swallowing and developed pain over his right eye. He was found to have nasopharyngeal carcinoma spreading down into his skull base and neck.
Even today surgery to remove cancer from that area is tricky. In 1946 it didn’t exist. An experimental treatment of combined radiation and chemotherapy – today standard – was tried, including a new folic acid derivative called teropterin. He improved somewhat – enough that he was an unnamed case study presented at a medical meeting – but had lost 80 pounds. After a brief respite he continued to go downhill. On June 13, 1948, he appeared at Yankee Stadium – the house that Ruth built – for the last time, where he was honored. He had difficulty walking and used a baseball bat as a cane. His pharynx was so damaged his voice could barely be heard. He died 2 months later on Aug. 16, 1948.
This isn’t a sports column, I’m not a sports writer, and this definitely ain’t Sport Illustrated. So why am I writing this?
Because Babe Ruth never knew he had cancer. Was never told he was dying. His family was afraid he’d harm himself if he knew, so his doctors were under strict instructions to keep the bad news from him.
Now, Ruth wasn’t stupid. Wild, unrepentant, hedonistic, and a lot of other things – but not stupid. He certainly must have figured it out with getting radiation, or chemotherapy, or his declining physical status. But none of his doctors or family ever told him he had cancer and was dying (what they did tell him I have no idea).
Let’s look at this as a case history: A 51-year-old male, possessed of all his mental faculties, presents with headaches, dysphonia, and dysphagia. Workup reveals advanced, inoperable, nasopharyngeal cancer. The family is willing to accept treatment, but understands the prognosis is poor. Family members request that, under no circumstances, he be told of the diagnosis or prognosis.
The fact that the patient is probably the biggest celebrity of his era shouldn’t make a difference, but it does.
I’m sure most of us would want to tell the patient. We live in an age of patient autonomy. . But what if the family has concerns that the patient would hurt himself, as Ruth’s family did?
This summer is 75 years since the Babe died. Medicine has changed a lot, but some questions never will.
What would you do?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Babe Ruth was arguably the greatest athlete in American history.
Certainly, there have been, and always will be, many great figures in all sports. But none of them – Michael Jordan or LeBron James or Tom Brady – have ever, probably will never, dominate sports AND society in the way Babe Ruth did.
Ruth wasn’t an angel, nor did he claim to be. But he was a center of American life the way no athlete ever was or will be.
He was a remarkably good baseball player. In an era where home runs were rarities, he hit more than the entire rest of Major League Baseball combined. But he wasn’t just a slugger, he was an excellent play maker, fielder, and pitcher. (He was actually one of the best pitchers of his era, something else mostly forgotten today.)
Ruth retired in 1935. He never entirely left the limelight, with fans showing up even to watch him play golf in celebrity tournaments. In 1939 he spoke on July 4 at Lou Gehrig appreciation day as his former teammate was publicly dying of ALS.
In 1946 Ruth began having trouble swallowing and developed pain over his right eye. He was found to have nasopharyngeal carcinoma spreading down into his skull base and neck.
Even today surgery to remove cancer from that area is tricky. In 1946 it didn’t exist. An experimental treatment of combined radiation and chemotherapy – today standard – was tried, including a new folic acid derivative called teropterin. He improved somewhat – enough that he was an unnamed case study presented at a medical meeting – but had lost 80 pounds. After a brief respite he continued to go downhill. On June 13, 1948, he appeared at Yankee Stadium – the house that Ruth built – for the last time, where he was honored. He had difficulty walking and used a baseball bat as a cane. His pharynx was so damaged his voice could barely be heard. He died 2 months later on Aug. 16, 1948.
This isn’t a sports column, I’m not a sports writer, and this definitely ain’t Sport Illustrated. So why am I writing this?
Because Babe Ruth never knew he had cancer. Was never told he was dying. His family was afraid he’d harm himself if he knew, so his doctors were under strict instructions to keep the bad news from him.
Now, Ruth wasn’t stupid. Wild, unrepentant, hedonistic, and a lot of other things – but not stupid. He certainly must have figured it out with getting radiation, or chemotherapy, or his declining physical status. But none of his doctors or family ever told him he had cancer and was dying (what they did tell him I have no idea).
Let’s look at this as a case history: A 51-year-old male, possessed of all his mental faculties, presents with headaches, dysphonia, and dysphagia. Workup reveals advanced, inoperable, nasopharyngeal cancer. The family is willing to accept treatment, but understands the prognosis is poor. Family members request that, under no circumstances, he be told of the diagnosis or prognosis.
The fact that the patient is probably the biggest celebrity of his era shouldn’t make a difference, but it does.
I’m sure most of us would want to tell the patient. We live in an age of patient autonomy. . But what if the family has concerns that the patient would hurt himself, as Ruth’s family did?
This summer is 75 years since the Babe died. Medicine has changed a lot, but some questions never will.
What would you do?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Sick humor
This past June, during the search for the Titan submersible, and since then, we’ve had a not-entirely-unexpected development: Sick humor.
There was a lot of it. The Subway owner who got reprimanded for putting “Our subs don’t implode” on his sign was minor league compared with other things circulating on the Internet. One example that was sent to me showed the late Stockton Rush, OceanGate’s co-owner, as the new spokesman for Cap’n Crunch.
Of course, this is nothing new. People have made jokes about awful situations since to the dawn of civilization.
Why do we do this?
Humor is a remarkably human trait. There’s evidence other mammals have it, but not to the extent we do. We’ve created a multitude of forms that vary between cultures. But there isn’t a civilization or culture on Earth that doesn’t have humor.
Why we developed it I’ll leave to others, though I assume a key part is that it strengthens bonds between people, helping them stick together in the groups that keep society moving forward.
Sick humor is part of this, though having grown up watching Monty Python and reading National Lampoon magazine I’m certainly guilty of enjoying it. To this day I think “Eating Raoul” is one of the greatest comedies ever.
It’s also pretty common in medicine. I’ve been involved in plenty of hospital situations that were quite unfunny, yet there are always jokes about it flying as we work.
I assume it’s a defense mechanism. Helping us cope with a bad situation as we do our best to deal with it. Using humor to put a block between the obvious realization that someday this could happen to us. To help psychologically shield us from something tragic.
Years ago I was trying to describe the plot of “Eating Raoul” and said “if you read about this sort of crime spree in a newspaper you’d be horrified. But the way it’s handled in the movie it’s hysterical.” Perhaps that’s as close to understanding sick humor as I’ll ever get. It makes the unfunny funny.
Perhaps the better phrase is the more generic “it’s human nature.”
Whether or not it’s funny depends on the person. There were plenty of people horrified by the Subway sign, enough that the owner had to change it. But there were also those who admitted they found it tasteless, but still got a laugh out of it. I’m sure the families of those lost on the Titan were justifiably upset, but the closer you get to a personal tragedy the more serious it is.
There’s a fine line, as National Lampoon put it, between funny and sick. But it’s also part of who we are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This past June, during the search for the Titan submersible, and since then, we’ve had a not-entirely-unexpected development: Sick humor.
There was a lot of it. The Subway owner who got reprimanded for putting “Our subs don’t implode” on his sign was minor league compared with other things circulating on the Internet. One example that was sent to me showed the late Stockton Rush, OceanGate’s co-owner, as the new spokesman for Cap’n Crunch.
Of course, this is nothing new. People have made jokes about awful situations since to the dawn of civilization.
Why do we do this?
Humor is a remarkably human trait. There’s evidence other mammals have it, but not to the extent we do. We’ve created a multitude of forms that vary between cultures. But there isn’t a civilization or culture on Earth that doesn’t have humor.
Why we developed it I’ll leave to others, though I assume a key part is that it strengthens bonds between people, helping them stick together in the groups that keep society moving forward.
Sick humor is part of this, though having grown up watching Monty Python and reading National Lampoon magazine I’m certainly guilty of enjoying it. To this day I think “Eating Raoul” is one of the greatest comedies ever.
It’s also pretty common in medicine. I’ve been involved in plenty of hospital situations that were quite unfunny, yet there are always jokes about it flying as we work.
I assume it’s a defense mechanism. Helping us cope with a bad situation as we do our best to deal with it. Using humor to put a block between the obvious realization that someday this could happen to us. To help psychologically shield us from something tragic.
Years ago I was trying to describe the plot of “Eating Raoul” and said “if you read about this sort of crime spree in a newspaper you’d be horrified. But the way it’s handled in the movie it’s hysterical.” Perhaps that’s as close to understanding sick humor as I’ll ever get. It makes the unfunny funny.
Perhaps the better phrase is the more generic “it’s human nature.”
Whether or not it’s funny depends on the person. There were plenty of people horrified by the Subway sign, enough that the owner had to change it. But there were also those who admitted they found it tasteless, but still got a laugh out of it. I’m sure the families of those lost on the Titan were justifiably upset, but the closer you get to a personal tragedy the more serious it is.
There’s a fine line, as National Lampoon put it, between funny and sick. But it’s also part of who we are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This past June, during the search for the Titan submersible, and since then, we’ve had a not-entirely-unexpected development: Sick humor.
There was a lot of it. The Subway owner who got reprimanded for putting “Our subs don’t implode” on his sign was minor league compared with other things circulating on the Internet. One example that was sent to me showed the late Stockton Rush, OceanGate’s co-owner, as the new spokesman for Cap’n Crunch.
Of course, this is nothing new. People have made jokes about awful situations since to the dawn of civilization.
Why do we do this?
Humor is a remarkably human trait. There’s evidence other mammals have it, but not to the extent we do. We’ve created a multitude of forms that vary between cultures. But there isn’t a civilization or culture on Earth that doesn’t have humor.
Why we developed it I’ll leave to others, though I assume a key part is that it strengthens bonds between people, helping them stick together in the groups that keep society moving forward.
Sick humor is part of this, though having grown up watching Monty Python and reading National Lampoon magazine I’m certainly guilty of enjoying it. To this day I think “Eating Raoul” is one of the greatest comedies ever.
It’s also pretty common in medicine. I’ve been involved in plenty of hospital situations that were quite unfunny, yet there are always jokes about it flying as we work.
I assume it’s a defense mechanism. Helping us cope with a bad situation as we do our best to deal with it. Using humor to put a block between the obvious realization that someday this could happen to us. To help psychologically shield us from something tragic.
Years ago I was trying to describe the plot of “Eating Raoul” and said “if you read about this sort of crime spree in a newspaper you’d be horrified. But the way it’s handled in the movie it’s hysterical.” Perhaps that’s as close to understanding sick humor as I’ll ever get. It makes the unfunny funny.
Perhaps the better phrase is the more generic “it’s human nature.”
Whether or not it’s funny depends on the person. There were plenty of people horrified by the Subway sign, enough that the owner had to change it. But there were also those who admitted they found it tasteless, but still got a laugh out of it. I’m sure the families of those lost on the Titan were justifiably upset, but the closer you get to a personal tragedy the more serious it is.
There’s a fine line, as National Lampoon put it, between funny and sick. But it’s also part of who we are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Looking back and looking ahead
This last week I quietly reached a milestone. I didn’t do anything special about it; it was just another office day.
I passed 25 years since I first began seeing patients as an attending physician. That’s a pretty decent chunk of time.
I was terrified that day. For the first time in my medical career I was working without a net. I even remember the first one, a fellow with back pain. I saw five to six patients that day that I recall, including a work-in from the fellowship I’d completed 2 weeks earlier. I also had my first hospital consult when the oncologist I was subleasing from asked me to have a look at a lady he was admitting for new-onset diplopia.
That’s a good chuck of a career behind me, when you consider the beginnings of it. College, MCATs, waiting by the mailbox (yeah, kids, a mailbox, waiting for a printed letter, delivered by the postman). Moving halfway across the country for 4 years. Somehow, to my own amazement, graduating. Moving back. Internship. Residency. Fellowship.
Then my first day as an attending, now a quarter-century gone. Looking at my charts I’ve seen roughly 18,000 individual patients over time between my office and the hospital.
But that’s another change – after 22 years in the trenches, I stopped doing hospital work over 3 years ago. Inpatient work, at least to me now, seems more like a younger person’s game. In my late 50s, I don’t think I qualify as one anymore.
On day 1, also in the Phoenix summer, I wore a long-sleeved shirt, tie, slacks, and neatly polished shoes. In 2006 I moved to Hawaiian shirts, shorts, and sneakers.
I don’t plan on doing this in another 25 years. I still like it, but by then I will have passed the baton to another generation and will be off on a cruise ship having boat drinks in the afternoon.
But that’s not to say it hasn’t been fun. For all the frustrations, stresses, and aggravations, I have no regrets over the road I’ve taken, and hopefully I will always feel that way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This last week I quietly reached a milestone. I didn’t do anything special about it; it was just another office day.
I passed 25 years since I first began seeing patients as an attending physician. That’s a pretty decent chunk of time.
I was terrified that day. For the first time in my medical career I was working without a net. I even remember the first one, a fellow with back pain. I saw five to six patients that day that I recall, including a work-in from the fellowship I’d completed 2 weeks earlier. I also had my first hospital consult when the oncologist I was subleasing from asked me to have a look at a lady he was admitting for new-onset diplopia.
That’s a good chuck of a career behind me, when you consider the beginnings of it. College, MCATs, waiting by the mailbox (yeah, kids, a mailbox, waiting for a printed letter, delivered by the postman). Moving halfway across the country for 4 years. Somehow, to my own amazement, graduating. Moving back. Internship. Residency. Fellowship.
Then my first day as an attending, now a quarter-century gone. Looking at my charts I’ve seen roughly 18,000 individual patients over time between my office and the hospital.
But that’s another change – after 22 years in the trenches, I stopped doing hospital work over 3 years ago. Inpatient work, at least to me now, seems more like a younger person’s game. In my late 50s, I don’t think I qualify as one anymore.
On day 1, also in the Phoenix summer, I wore a long-sleeved shirt, tie, slacks, and neatly polished shoes. In 2006 I moved to Hawaiian shirts, shorts, and sneakers.
I don’t plan on doing this in another 25 years. I still like it, but by then I will have passed the baton to another generation and will be off on a cruise ship having boat drinks in the afternoon.
But that’s not to say it hasn’t been fun. For all the frustrations, stresses, and aggravations, I have no regrets over the road I’ve taken, and hopefully I will always feel that way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This last week I quietly reached a milestone. I didn’t do anything special about it; it was just another office day.
I passed 25 years since I first began seeing patients as an attending physician. That’s a pretty decent chunk of time.
I was terrified that day. For the first time in my medical career I was working without a net. I even remember the first one, a fellow with back pain. I saw five to six patients that day that I recall, including a work-in from the fellowship I’d completed 2 weeks earlier. I also had my first hospital consult when the oncologist I was subleasing from asked me to have a look at a lady he was admitting for new-onset diplopia.
That’s a good chuck of a career behind me, when you consider the beginnings of it. College, MCATs, waiting by the mailbox (yeah, kids, a mailbox, waiting for a printed letter, delivered by the postman). Moving halfway across the country for 4 years. Somehow, to my own amazement, graduating. Moving back. Internship. Residency. Fellowship.
Then my first day as an attending, now a quarter-century gone. Looking at my charts I’ve seen roughly 18,000 individual patients over time between my office and the hospital.
But that’s another change – after 22 years in the trenches, I stopped doing hospital work over 3 years ago. Inpatient work, at least to me now, seems more like a younger person’s game. In my late 50s, I don’t think I qualify as one anymore.
On day 1, also in the Phoenix summer, I wore a long-sleeved shirt, tie, slacks, and neatly polished shoes. In 2006 I moved to Hawaiian shirts, shorts, and sneakers.
I don’t plan on doing this in another 25 years. I still like it, but by then I will have passed the baton to another generation and will be off on a cruise ship having boat drinks in the afternoon.
But that’s not to say it hasn’t been fun. For all the frustrations, stresses, and aggravations, I have no regrets over the road I’ve taken, and hopefully I will always feel that way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Alzheimer’s disease: To treat or not?
Mr. Jones has Alzheimer’s disease, recently diagnosed.
His wife is a retired hospice nurse, who’s seen plenty of patients and families deal with the illness over the years.
She came in recently, just herself, to go over his treatment options and what can be reasonably expected with them. So we went through the usual suspects, new and old.
I intermittently stopped to ask if she had any questions. At one such break she suddenly said:
“I’d rather he die now than be treated with any of these.”
I tried to address her safety concerns with the different medications, but that wasn’t the issue. Her real, and understandable, point is that none of them are cures. They don’t even stop the disease. Realistically, all we’re doing is slowing things down for maybe a year at most.
Families are different, and no one can really know how they’ll react in this situation until it happens.
Some will want me to do a full-court press, because another year of time is more family gatherings and independence, maybe a grandchild’s birth or wedding, or just being able to keep someone at home longer before starting to look into the cost of memory care.
Others, like Mrs. Jones, don’t see a point. The disease is incurable. Why bother to prolong it when the end is the same? Is it worth adding another year of medications, adult diapers, and the occasional 911 call if they wander off?
That’s a valid view, too. She wasn’t advocating a cause, such as euthanasia, but she did have legitimate concerns.
For all the marketing hype over Leqembi today or Cognex (remember that?) in 1989, the issue is the same. We have new and shinier toys, but still no cures. Whether it’s worth it to prolong life (or suffering) is a glass half-full or half-empty question that only patients and their families can answer.
It ain’t easy.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mr. Jones has Alzheimer’s disease, recently diagnosed.
His wife is a retired hospice nurse, who’s seen plenty of patients and families deal with the illness over the years.
She came in recently, just herself, to go over his treatment options and what can be reasonably expected with them. So we went through the usual suspects, new and old.
I intermittently stopped to ask if she had any questions. At one such break she suddenly said:
“I’d rather he die now than be treated with any of these.”
I tried to address her safety concerns with the different medications, but that wasn’t the issue. Her real, and understandable, point is that none of them are cures. They don’t even stop the disease. Realistically, all we’re doing is slowing things down for maybe a year at most.
Families are different, and no one can really know how they’ll react in this situation until it happens.
Some will want me to do a full-court press, because another year of time is more family gatherings and independence, maybe a grandchild’s birth or wedding, or just being able to keep someone at home longer before starting to look into the cost of memory care.
Others, like Mrs. Jones, don’t see a point. The disease is incurable. Why bother to prolong it when the end is the same? Is it worth adding another year of medications, adult diapers, and the occasional 911 call if they wander off?
That’s a valid view, too. She wasn’t advocating a cause, such as euthanasia, but she did have legitimate concerns.
For all the marketing hype over Leqembi today or Cognex (remember that?) in 1989, the issue is the same. We have new and shinier toys, but still no cures. Whether it’s worth it to prolong life (or suffering) is a glass half-full or half-empty question that only patients and their families can answer.
It ain’t easy.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mr. Jones has Alzheimer’s disease, recently diagnosed.
His wife is a retired hospice nurse, who’s seen plenty of patients and families deal with the illness over the years.
She came in recently, just herself, to go over his treatment options and what can be reasonably expected with them. So we went through the usual suspects, new and old.
I intermittently stopped to ask if she had any questions. At one such break she suddenly said:
“I’d rather he die now than be treated with any of these.”
I tried to address her safety concerns with the different medications, but that wasn’t the issue. Her real, and understandable, point is that none of them are cures. They don’t even stop the disease. Realistically, all we’re doing is slowing things down for maybe a year at most.
Families are different, and no one can really know how they’ll react in this situation until it happens.
Some will want me to do a full-court press, because another year of time is more family gatherings and independence, maybe a grandchild’s birth or wedding, or just being able to keep someone at home longer before starting to look into the cost of memory care.
Others, like Mrs. Jones, don’t see a point. The disease is incurable. Why bother to prolong it when the end is the same? Is it worth adding another year of medications, adult diapers, and the occasional 911 call if they wander off?
That’s a valid view, too. She wasn’t advocating a cause, such as euthanasia, but she did have legitimate concerns.
For all the marketing hype over Leqembi today or Cognex (remember that?) in 1989, the issue is the same. We have new and shinier toys, but still no cures. Whether it’s worth it to prolong life (or suffering) is a glass half-full or half-empty question that only patients and their families can answer.
It ain’t easy.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Flying cars and subdermal labs
A headline recently caught my eye about flying cars close to being a reality. Since this is pretty much the dream of everyone who grew up watching “The Jetsons,” I paused to read it.
Of course, it wasn’t quite what I hoped. Battery-powered short-range helicopter services to fly people to airports – to alleviate traffic congestion – have received Food and Drug Administration approval for testing.
In other words, they are still years away, I’m not going to be at the controls, and I won’t be taking them to my office anytime soon. (Granted, it’s only 5 minutes from my house, but wouldn’t you rather fly?)
Maybe it’s hyperbole, maybe clickbait, maybe just an enthusiastic writer, or a little of each.
On a similar note, a recent article titled, “A tiny patch may someday do your patients’ lab work,” about patches with microneedles to measure interstitial fluid, got my attention.
It certainly sounds promising, and more reasonable than the Theranos scam. This has interesting potential as a way to track lab values without repeated needle sticks.
But “someday” is the key word here. The technology is promising. For some conditions it certainly has the potential to improve patient care without frequent lab trips and blood draws.
But the point is ... it ain’t here yet. At the end of the article it says it may be available for some things within 2 years, with more indications over the next decade.
I’m not knocking the technology. That’s great news. But I’m seeing patients today. If I can’t offer it to them now, it doesn’t matter to me.
Maybe I’m a skeptic, but I’ve seen too many initially promising treatments or tests go nowhere when they move into large-scale trials. A lot of things seem like great ideas that don’t work out.
I think the microneedle patch probably has a future for certain conditions, and when it gets here it will be great for those who need it. But that won’t be tomorrow, or even 2024.
But, as with someday flying to work, I’m not holding my breath for it, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A headline recently caught my eye about flying cars close to being a reality. Since this is pretty much the dream of everyone who grew up watching “The Jetsons,” I paused to read it.
Of course, it wasn’t quite what I hoped. Battery-powered short-range helicopter services to fly people to airports – to alleviate traffic congestion – have received Food and Drug Administration approval for testing.
In other words, they are still years away, I’m not going to be at the controls, and I won’t be taking them to my office anytime soon. (Granted, it’s only 5 minutes from my house, but wouldn’t you rather fly?)
Maybe it’s hyperbole, maybe clickbait, maybe just an enthusiastic writer, or a little of each.
On a similar note, a recent article titled, “A tiny patch may someday do your patients’ lab work,” about patches with microneedles to measure interstitial fluid, got my attention.
It certainly sounds promising, and more reasonable than the Theranos scam. This has interesting potential as a way to track lab values without repeated needle sticks.
But “someday” is the key word here. The technology is promising. For some conditions it certainly has the potential to improve patient care without frequent lab trips and blood draws.
But the point is ... it ain’t here yet. At the end of the article it says it may be available for some things within 2 years, with more indications over the next decade.
I’m not knocking the technology. That’s great news. But I’m seeing patients today. If I can’t offer it to them now, it doesn’t matter to me.
Maybe I’m a skeptic, but I’ve seen too many initially promising treatments or tests go nowhere when they move into large-scale trials. A lot of things seem like great ideas that don’t work out.
I think the microneedle patch probably has a future for certain conditions, and when it gets here it will be great for those who need it. But that won’t be tomorrow, or even 2024.
But, as with someday flying to work, I’m not holding my breath for it, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A headline recently caught my eye about flying cars close to being a reality. Since this is pretty much the dream of everyone who grew up watching “The Jetsons,” I paused to read it.
Of course, it wasn’t quite what I hoped. Battery-powered short-range helicopter services to fly people to airports – to alleviate traffic congestion – have received Food and Drug Administration approval for testing.
In other words, they are still years away, I’m not going to be at the controls, and I won’t be taking them to my office anytime soon. (Granted, it’s only 5 minutes from my house, but wouldn’t you rather fly?)
Maybe it’s hyperbole, maybe clickbait, maybe just an enthusiastic writer, or a little of each.
On a similar note, a recent article titled, “A tiny patch may someday do your patients’ lab work,” about patches with microneedles to measure interstitial fluid, got my attention.
It certainly sounds promising, and more reasonable than the Theranos scam. This has interesting potential as a way to track lab values without repeated needle sticks.
But “someday” is the key word here. The technology is promising. For some conditions it certainly has the potential to improve patient care without frequent lab trips and blood draws.
But the point is ... it ain’t here yet. At the end of the article it says it may be available for some things within 2 years, with more indications over the next decade.
I’m not knocking the technology. That’s great news. But I’m seeing patients today. If I can’t offer it to them now, it doesn’t matter to me.
Maybe I’m a skeptic, but I’ve seen too many initially promising treatments or tests go nowhere when they move into large-scale trials. A lot of things seem like great ideas that don’t work out.
I think the microneedle patch probably has a future for certain conditions, and when it gets here it will be great for those who need it. But that won’t be tomorrow, or even 2024.
But, as with someday flying to work, I’m not holding my breath for it, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Safety first: Regulations
The word “regulations” gets a mixed response.
This is common in all industries, and certainly pharmaceuticals. On any given day there are stories on industry news sites about disputes between companies and regulatory agencies.
I’d agree that some regulation is needed. The history of pharmacy has had both remarkable successes – and failures.
Let’s look at migraines, since that’s in my field. The calcitonin gene-related peptide (CGRP) drugs have been a remarkable breakthrough, certainly the biggest one since the triptans in 1992. There are currently seven on the market for both prevention and abortive use. They’re effective and (to date) pretty safe.
But it wasn’t always that way. Look back just 14 years ago to 2009, when the first promising CGRP agent (MK-3207) had its development halted because of hepatic abnormalities. It’s cousin telcagepant (MK-0974) came to a similar end 2 years later.
Without regulations in place (and the potential for lawsuits) these might have made it to market, bringing migraine relief to some and potentially serious liver damage to others. So Merck made the right decision to axe them. Researchers learned from the experience, went back to the drawing board, and developed the current generation of far-safer drugs.
This came into sharp focus in another industry recently, when the eyes of the world were on the north Atlantic. A small tourist submarine imploded and killed five people. During the inevitable media coverage it came out that the submarine hadn’t been certified for safety by any of the agencies that handle such things, falling into a gray area in international waters where inspections aren’t required.
This isn’t to say it wasn’t safe – it had made several dives before – but obviously not safe enough. While I didn’t know the late Stockton Rush (the owner/designer) it sounds like he viewed regulations as stifling innovation, and in one interview said “at some point, safety is just pure waste.” He ignored warnings from several sides about the submersible’s ability to handle deep ocean pressure and the inevitable wear and tear repeated dives will have on the hull.
I understand there’s a margin of luck, too. Bad things can happen to any of us – or any company. Some things can’t be clearly foreseen. Some drugs don’t start to show problems until they’re on the market and reach a certain number of prescriptions.
But there’s a reason we have regulations. Pretty much every government has, going back to the Roman Empire, covering numerous things. In a perfect world we wouldn’t need them.
But people are far from perfect. And the consequences can be terrible.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The word “regulations” gets a mixed response.
This is common in all industries, and certainly pharmaceuticals. On any given day there are stories on industry news sites about disputes between companies and regulatory agencies.
I’d agree that some regulation is needed. The history of pharmacy has had both remarkable successes – and failures.
Let’s look at migraines, since that’s in my field. The calcitonin gene-related peptide (CGRP) drugs have been a remarkable breakthrough, certainly the biggest one since the triptans in 1992. There are currently seven on the market for both prevention and abortive use. They’re effective and (to date) pretty safe.
But it wasn’t always that way. Look back just 14 years ago to 2009, when the first promising CGRP agent (MK-3207) had its development halted because of hepatic abnormalities. It’s cousin telcagepant (MK-0974) came to a similar end 2 years later.
Without regulations in place (and the potential for lawsuits) these might have made it to market, bringing migraine relief to some and potentially serious liver damage to others. So Merck made the right decision to axe them. Researchers learned from the experience, went back to the drawing board, and developed the current generation of far-safer drugs.
This came into sharp focus in another industry recently, when the eyes of the world were on the north Atlantic. A small tourist submarine imploded and killed five people. During the inevitable media coverage it came out that the submarine hadn’t been certified for safety by any of the agencies that handle such things, falling into a gray area in international waters where inspections aren’t required.
This isn’t to say it wasn’t safe – it had made several dives before – but obviously not safe enough. While I didn’t know the late Stockton Rush (the owner/designer) it sounds like he viewed regulations as stifling innovation, and in one interview said “at some point, safety is just pure waste.” He ignored warnings from several sides about the submersible’s ability to handle deep ocean pressure and the inevitable wear and tear repeated dives will have on the hull.
I understand there’s a margin of luck, too. Bad things can happen to any of us – or any company. Some things can’t be clearly foreseen. Some drugs don’t start to show problems until they’re on the market and reach a certain number of prescriptions.
But there’s a reason we have regulations. Pretty much every government has, going back to the Roman Empire, covering numerous things. In a perfect world we wouldn’t need them.
But people are far from perfect. And the consequences can be terrible.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The word “regulations” gets a mixed response.
This is common in all industries, and certainly pharmaceuticals. On any given day there are stories on industry news sites about disputes between companies and regulatory agencies.
I’d agree that some regulation is needed. The history of pharmacy has had both remarkable successes – and failures.
Let’s look at migraines, since that’s in my field. The calcitonin gene-related peptide (CGRP) drugs have been a remarkable breakthrough, certainly the biggest one since the triptans in 1992. There are currently seven on the market for both prevention and abortive use. They’re effective and (to date) pretty safe.
But it wasn’t always that way. Look back just 14 years ago to 2009, when the first promising CGRP agent (MK-3207) had its development halted because of hepatic abnormalities. It’s cousin telcagepant (MK-0974) came to a similar end 2 years later.
Without regulations in place (and the potential for lawsuits) these might have made it to market, bringing migraine relief to some and potentially serious liver damage to others. So Merck made the right decision to axe them. Researchers learned from the experience, went back to the drawing board, and developed the current generation of far-safer drugs.
This came into sharp focus in another industry recently, when the eyes of the world were on the north Atlantic. A small tourist submarine imploded and killed five people. During the inevitable media coverage it came out that the submarine hadn’t been certified for safety by any of the agencies that handle such things, falling into a gray area in international waters where inspections aren’t required.
This isn’t to say it wasn’t safe – it had made several dives before – but obviously not safe enough. While I didn’t know the late Stockton Rush (the owner/designer) it sounds like he viewed regulations as stifling innovation, and in one interview said “at some point, safety is just pure waste.” He ignored warnings from several sides about the submersible’s ability to handle deep ocean pressure and the inevitable wear and tear repeated dives will have on the hull.
I understand there’s a margin of luck, too. Bad things can happen to any of us – or any company. Some things can’t be clearly foreseen. Some drugs don’t start to show problems until they’re on the market and reach a certain number of prescriptions.
But there’s a reason we have regulations. Pretty much every government has, going back to the Roman Empire, covering numerous things. In a perfect world we wouldn’t need them.
But people are far from perfect. And the consequences can be terrible.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
You’ve been warned
Recently, Canada announced new regulations on tobacco, with warnings printed on individual cigarettes, such as “poison in every puff.” This is on top of the packaging already required to have 75% of its space devoted to similar warnings, often with graphic pictures, of the potential consequences.
Make no mistake, I don’t like cigarettes and try to get smokers to quit.
But I have to wonder how successful this is going to be. I mean, you’d have to have lived under a rock for the last 70 years (or more) to not know that cigarettes (and tobacco in general) aren’t good for you, and can cause stroke, heart disease, and a multitude of cancers.
I suppose you could ban cigarettes, but that only opens up a black market. From 1920 to 1933 the United States set an example for the world with prohibition, showing how such an idea can backfire horribly.
Realistically, there are always going to be people making bad health decisions of one kind or another, including myself. Whether it’s tobacco, alcohol, or a cheeseburger and fries.
Tobacco, of course, has a much worse track record than that of the cheeseburger. We all have to eat, even though some choices are better than others. Tobacco has absolutely no biological necessity, as do food, air, and water.
But it’s remarkably addictive, not to mention profitable. Those factors will always guarantee it a place in society.
At this point,
There’s a legitimate argument to be made in trying to keep people from starting. The teenage years, where we all tend to believe we’re immortal, are when a lot of habits (good and bad) form. If gruesome pictures and repeated warnings cut down on those numbers, then in the long run it’s a very good thing. Given that Canada’s goal is to cut tobacco use from 13% down to less than 5% by 2035, this could happen. Only time will tell how it plays out.
On a side note, here in the United States tobacco use is 19% of the population. This is actually somewhat surprising to me, as a brief, not particularly scientific, review of my charts for the past few weeks found that less than 5% of my patients do it. So either some are lying or (more likely), it’s just the demographics of my practice area.
But at some point it doesn’t matter how many warnings or gory pictures people see, or where they encounter them. Some will keep smoking out of habit. Some because they actually like it. Some to be defiant. Some just because they can. And no amount of warnings is going to change their minds.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, Canada announced new regulations on tobacco, with warnings printed on individual cigarettes, such as “poison in every puff.” This is on top of the packaging already required to have 75% of its space devoted to similar warnings, often with graphic pictures, of the potential consequences.
Make no mistake, I don’t like cigarettes and try to get smokers to quit.
But I have to wonder how successful this is going to be. I mean, you’d have to have lived under a rock for the last 70 years (or more) to not know that cigarettes (and tobacco in general) aren’t good for you, and can cause stroke, heart disease, and a multitude of cancers.
I suppose you could ban cigarettes, but that only opens up a black market. From 1920 to 1933 the United States set an example for the world with prohibition, showing how such an idea can backfire horribly.
Realistically, there are always going to be people making bad health decisions of one kind or another, including myself. Whether it’s tobacco, alcohol, or a cheeseburger and fries.
Tobacco, of course, has a much worse track record than that of the cheeseburger. We all have to eat, even though some choices are better than others. Tobacco has absolutely no biological necessity, as do food, air, and water.
But it’s remarkably addictive, not to mention profitable. Those factors will always guarantee it a place in society.
At this point,
There’s a legitimate argument to be made in trying to keep people from starting. The teenage years, where we all tend to believe we’re immortal, are when a lot of habits (good and bad) form. If gruesome pictures and repeated warnings cut down on those numbers, then in the long run it’s a very good thing. Given that Canada’s goal is to cut tobacco use from 13% down to less than 5% by 2035, this could happen. Only time will tell how it plays out.
On a side note, here in the United States tobacco use is 19% of the population. This is actually somewhat surprising to me, as a brief, not particularly scientific, review of my charts for the past few weeks found that less than 5% of my patients do it. So either some are lying or (more likely), it’s just the demographics of my practice area.
But at some point it doesn’t matter how many warnings or gory pictures people see, or where they encounter them. Some will keep smoking out of habit. Some because they actually like it. Some to be defiant. Some just because they can. And no amount of warnings is going to change their minds.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, Canada announced new regulations on tobacco, with warnings printed on individual cigarettes, such as “poison in every puff.” This is on top of the packaging already required to have 75% of its space devoted to similar warnings, often with graphic pictures, of the potential consequences.
Make no mistake, I don’t like cigarettes and try to get smokers to quit.
But I have to wonder how successful this is going to be. I mean, you’d have to have lived under a rock for the last 70 years (or more) to not know that cigarettes (and tobacco in general) aren’t good for you, and can cause stroke, heart disease, and a multitude of cancers.
I suppose you could ban cigarettes, but that only opens up a black market. From 1920 to 1933 the United States set an example for the world with prohibition, showing how such an idea can backfire horribly.
Realistically, there are always going to be people making bad health decisions of one kind or another, including myself. Whether it’s tobacco, alcohol, or a cheeseburger and fries.
Tobacco, of course, has a much worse track record than that of the cheeseburger. We all have to eat, even though some choices are better than others. Tobacco has absolutely no biological necessity, as do food, air, and water.
But it’s remarkably addictive, not to mention profitable. Those factors will always guarantee it a place in society.
At this point,
There’s a legitimate argument to be made in trying to keep people from starting. The teenage years, where we all tend to believe we’re immortal, are when a lot of habits (good and bad) form. If gruesome pictures and repeated warnings cut down on those numbers, then in the long run it’s a very good thing. Given that Canada’s goal is to cut tobacco use from 13% down to less than 5% by 2035, this could happen. Only time will tell how it plays out.
On a side note, here in the United States tobacco use is 19% of the population. This is actually somewhat surprising to me, as a brief, not particularly scientific, review of my charts for the past few weeks found that less than 5% of my patients do it. So either some are lying or (more likely), it’s just the demographics of my practice area.
But at some point it doesn’t matter how many warnings or gory pictures people see, or where they encounter them. Some will keep smoking out of habit. Some because they actually like it. Some to be defiant. Some just because they can. And no amount of warnings is going to change their minds.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The timekeeper
This little fellow greets you at my office. He’s been there for 25 years.
I don’t know where he came from originally. When I started out he was up front with the physician I subleased from and when he retired he passed him on to me (thanks, Fran!).
From the beginning he’s been the first thing I see when I arrive each morning. Because of my suprachiasmatic nucleus kicking me out of bed between 4 and 5 each morning, I’m always the first one in the office and so I update him. At this point he’s as much a part of my morning ritual as coffee and tea. I juggle the cubes to change the day (12 times a year I change the month) and once this is done I don’t think of him again until the next morning.
When I started setting him each morning I didn’t have kids. Now I have three, all grown. Patients, years, drug reps, and even a pandemic have all been marked by the clicking of his cubes when I change them each morning.
Now two-thirds of the way through my career, he’s taken on a different meaning. He’s counting down the days until I walk away and leave neurology in the hands of another generation. I don’t have a date for doing that, nor a plan to do so anytime soon, but sooner or later I’ll be changing his cubes for the last office day of my life as a neurologist.
What will happen to him then? Seems like a strange question to ask about an inanimate object, but after this much time I’ve gotten attached to the little guy. He’s come to symbolize more than just the date – he’s the passage of time. Maybe he’ll stay on a shelf at home, giving me something to do each morning of my retirement. Maybe one of my kids will want him.
Inevitably, he’ll probably end up at a charity store, awaiting a new owner. When that happens I hope he gives them something to pause, smile, and think about each day, like he did with me, as we travel around the sun together.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This little fellow greets you at my office. He’s been there for 25 years.
I don’t know where he came from originally. When I started out he was up front with the physician I subleased from and when he retired he passed him on to me (thanks, Fran!).
From the beginning he’s been the first thing I see when I arrive each morning. Because of my suprachiasmatic nucleus kicking me out of bed between 4 and 5 each morning, I’m always the first one in the office and so I update him. At this point he’s as much a part of my morning ritual as coffee and tea. I juggle the cubes to change the day (12 times a year I change the month) and once this is done I don’t think of him again until the next morning.
When I started setting him each morning I didn’t have kids. Now I have three, all grown. Patients, years, drug reps, and even a pandemic have all been marked by the clicking of his cubes when I change them each morning.
Now two-thirds of the way through my career, he’s taken on a different meaning. He’s counting down the days until I walk away and leave neurology in the hands of another generation. I don’t have a date for doing that, nor a plan to do so anytime soon, but sooner or later I’ll be changing his cubes for the last office day of my life as a neurologist.
What will happen to him then? Seems like a strange question to ask about an inanimate object, but after this much time I’ve gotten attached to the little guy. He’s come to symbolize more than just the date – he’s the passage of time. Maybe he’ll stay on a shelf at home, giving me something to do each morning of my retirement. Maybe one of my kids will want him.
Inevitably, he’ll probably end up at a charity store, awaiting a new owner. When that happens I hope he gives them something to pause, smile, and think about each day, like he did with me, as we travel around the sun together.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This little fellow greets you at my office. He’s been there for 25 years.
I don’t know where he came from originally. When I started out he was up front with the physician I subleased from and when he retired he passed him on to me (thanks, Fran!).
From the beginning he’s been the first thing I see when I arrive each morning. Because of my suprachiasmatic nucleus kicking me out of bed between 4 and 5 each morning, I’m always the first one in the office and so I update him. At this point he’s as much a part of my morning ritual as coffee and tea. I juggle the cubes to change the day (12 times a year I change the month) and once this is done I don’t think of him again until the next morning.
When I started setting him each morning I didn’t have kids. Now I have three, all grown. Patients, years, drug reps, and even a pandemic have all been marked by the clicking of his cubes when I change them each morning.
Now two-thirds of the way through my career, he’s taken on a different meaning. He’s counting down the days until I walk away and leave neurology in the hands of another generation. I don’t have a date for doing that, nor a plan to do so anytime soon, but sooner or later I’ll be changing his cubes for the last office day of my life as a neurologist.
What will happen to him then? Seems like a strange question to ask about an inanimate object, but after this much time I’ve gotten attached to the little guy. He’s come to symbolize more than just the date – he’s the passage of time. Maybe he’ll stay on a shelf at home, giving me something to do each morning of my retirement. Maybe one of my kids will want him.
Inevitably, he’ll probably end up at a charity store, awaiting a new owner. When that happens I hope he gives them something to pause, smile, and think about each day, like he did with me, as we travel around the sun together.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.