User login
Expanded approval for daratumumab in multiple myeloma
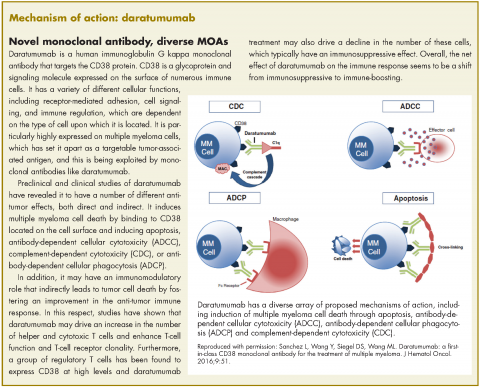
In November 2016, the US Food and Drug Administration expanded the approval of daratumumab for patients with multiple myeloma. The monoclonal antibody, which targets CD38, a protein that is highly expressed on the surface of multiple myeloma cells, was previously granted approval by the agency as a single agent for the treatment of patients who had received at least three previous therapies.
The current approval was for the use of daratumumab in two different combination regimens for the treatment of patients who have received one previous line of treatment. On the basis of improved progression-free survival (PFS), demonstrated in two randomized, open-label, phase 3 trials, daratumumab can now be used in combination with the immunomodulatory agent lenalidomide and dexamethasone, or the proteasome inhibitor bortezomib and dexamethasone, both standard therapies for the treatment of multiple myeloma.
In the POLLUX trial, 569 patients with relapsed/refractory multiple myeloma were randomized 1:1 to receive daratumumab in combination with lenalidomide-dexamethasone or lenalidomide-dexamethasone alone. The CASTOR trial randomized 498 patients with relapsed/refractory multiple myeloma 1:1 to daratumumab in combination with bortezomib-dexamethasone, or bortezomib-dexamethasone alone.
The eligibility and exclusion criteria for both trials were similar; patients had received at least one previous line of therapy, had documented progressive disease according to International Myeloma Working Group criteria, and had measurable disease on the basis of urine and/or serum assessments or serum-free, light-chain assay.
Patients with a neutrophil count of ≤1,000 cells/mm3, hemoglobin level of ≤7.5 g/dL, platelet count of <75,000 cells/mm3, creatinine clearance of ≤20 mL/min per 1.73m2 body surface area (or <30 mL/min in the POLLUX trial), alanine aminotransferase or aspartate aminotransferase level ≥2.5 times the upper limit of normal (ULN) range, bilirubin level of ≥1.5 or more times the ULN range, disease refractory to bortezomib or lenalidomide, and unacceptable side effects from bortezomib or lenalidomide, were ineligible for these studies. In addition, patients with grade 2 or higher peripheral neuropathy or neuropathic pain, were excluded from the CASTOR study.
Randomization was stratified according to International Staging System disease stage at the time of screening (stage I, II or III, with higher stage indicating more severe disease), number of previous lines of therapy (1 vs 2, or 3 vs >3), and previous receipt of lenalidomide or bortezomib.
In the CASTOR trial, patients received up to eight 21-day cycles of bortezomib, administered subcutaneously at a dose of 1.3 mg/m2 on days 1, 4, 8, and 11 of cycles 1-8, and dexamethasone, administered orally or intravenously at a dose of 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12 for a total dose of 160 mg per cycle. Daratumumab was administered at a dose of 16 mg/kg intravenously once weekly on days 1, 8, and 15 during cycles 1 to 3, once every 3 weeks on day 1 of cycles 4-8, and once every 4 weeks thereafter.
In the POLLUX trial, patients were treated in 28-day cycles. Daratumumab was administered at the same dose as in the CASTOR trial, but on days 1, 8, 15 and 22 for 8 weeks during cycles 1 and 2, every 2 weeks on days 1 and 15 for 16 weeks during cycles 3 through 7, and every 4 weeks from then onwards. Lenalidomide was administered at a dose of 25 mg orally on days 1-21 of each cycle, and dexamethasone at a dose of 20 mg before infusion and 20 mg the following day.
The combination of daratumumab with lenalidomide-dexamethasone demonstrated a substantial improvement in PFS, compared with lenalidomide-dexamethasone alone (estimated PFS not yet reached vs 18.4 months, respectively; HR, 0.37; P < .0001), representing a 63% reduction in the risk of disease progression or death. Meanwhile, there was a 61% reduction in the risk of disease progression or death for the combination of daratumumab with bortezomib-dexamethasone in the CASTOR trial (estimated PFS not yet reached vs 7.2 months; HR: 0.39; P < .0001). The PFS benefit was observed across all prespecified subgroups in both studies.
In the CASTOR trial, over a median follow-up of 7.4 months, the overall response rate (ORR) was 82.9% for the combination arm, compared with 63.2% for the bortezomib-dexamethasone arm (P < .001), with a very good partial response (VGPR) or better rate of 59.2% compared with 29.1%, and a complete response (CR) rate of 19.2% compared with 9%. In the POLLUX trial, over a median follow-up of 13.5 months, ORR was 92.9% for the combination arm, compared with 76.4% for lenalidomide-dexamethasone, with a VGPR or better rate of 75.8% versus 44% and a CR rate of 43.1% versus 19.2%.
Overall, the safety profile for both combinations was consistent with what is usually observed with daratumumab monotherapy and lenalidomide-dexamethasone or bortezomib-dexamethasone combinations. The most frequently reported adverse events (AEs) were similar in both studies and included infusion reactions, diarrhea, and upper respiratory tract infection. In the POLLUX trial they also included nausea, fatigue, pyrexia, muscle spasm, cough, and dyspnea, whereas in the CASTOR trial patients also frequently experienced peripheral edema.
The most common grade 3/4 AEs in both trials were neutropenia (51.9% vs 37% in the POLLUX trial and 12.8 vs 4.2% in the CASTOR trial), thrombocytopenia (12.7% vs 13.5% and 45.3% vs 32.9%, respectively), and anemia (12.4% vs 19.6% and 14.4% vs 16%, respectively). The percentage of patients who discontinued treatment due to AEs was similar in both groups across the two studies; in the CASTOR trial discontinuations resulted most commonly from peripheral sensory neuropathy and pneumonia, while in the POLLUX trial, from pneumonia, pulmonary embolism and deterioration in general physical health.
The recommended dose for daratumumab in both combination regimens is 16 mg/kg intravenously, calculated on actual body weight. The dosing schedules begin with weekly administration during weeks 1-8 (when used in combination with lenalidomide-dexamethasone) and weeks 1-9 (for use with the bortezomib-dexamethasone combination), decreasing to every 2 weeks between weeks 9 and 24 or 10 and 24, respectively, and progressing to every 4 weeks from week 25 onward until disease progression and unacceptable toxicity.
Daratumumab is marketed as Darzalex by Janssen Biotech Inc. Neutropenia and thrombocytopenia have been added to the list of warnings and precautions for the prescribing information for these new indications. Complete blood cell count should be monitored periodically during treatment and daratumumab administration delayed to allow recovery of neutrophils or platelets. Supportive care with growth factors or transfusion should be considered in the event of neutropenia or thrombocytopenia, respectively.
1. Darzalex (daratumumab) injection, for intravenous use. Prescribing information. Janssen Biotech Inc. https://www.darzalexhcp.com/shared/product/darzalex/darzalex-prescribing-information.pdf. Released November 2016. Accessed January 8, 2017.
2. Palumbo A, Chanan-Khan A, Weisel K, et al. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:754-766.
3. Dimopoulos MA, Oriol A, Nahi H, et al. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:1319-1331.
In November 2016, the US Food and Drug Administration expanded the approval of daratumumab for patients with multiple myeloma. The monoclonal antibody, which targets CD38, a protein that is highly expressed on the surface of multiple myeloma cells, was previously granted approval by the agency as a single agent for the treatment of patients who had received at least three previous therapies.
The current approval was for the use of daratumumab in two different combination regimens for the treatment of patients who have received one previous line of treatment. On the basis of improved progression-free survival (PFS), demonstrated in two randomized, open-label, phase 3 trials, daratumumab can now be used in combination with the immunomodulatory agent lenalidomide and dexamethasone, or the proteasome inhibitor bortezomib and dexamethasone, both standard therapies for the treatment of multiple myeloma.
In the POLLUX trial, 569 patients with relapsed/refractory multiple myeloma were randomized 1:1 to receive daratumumab in combination with lenalidomide-dexamethasone or lenalidomide-dexamethasone alone. The CASTOR trial randomized 498 patients with relapsed/refractory multiple myeloma 1:1 to daratumumab in combination with bortezomib-dexamethasone, or bortezomib-dexamethasone alone.
The eligibility and exclusion criteria for both trials were similar; patients had received at least one previous line of therapy, had documented progressive disease according to International Myeloma Working Group criteria, and had measurable disease on the basis of urine and/or serum assessments or serum-free, light-chain assay.
Patients with a neutrophil count of ≤1,000 cells/mm3, hemoglobin level of ≤7.5 g/dL, platelet count of <75,000 cells/mm3, creatinine clearance of ≤20 mL/min per 1.73m2 body surface area (or <30 mL/min in the POLLUX trial), alanine aminotransferase or aspartate aminotransferase level ≥2.5 times the upper limit of normal (ULN) range, bilirubin level of ≥1.5 or more times the ULN range, disease refractory to bortezomib or lenalidomide, and unacceptable side effects from bortezomib or lenalidomide, were ineligible for these studies. In addition, patients with grade 2 or higher peripheral neuropathy or neuropathic pain, were excluded from the CASTOR study.
Randomization was stratified according to International Staging System disease stage at the time of screening (stage I, II or III, with higher stage indicating more severe disease), number of previous lines of therapy (1 vs 2, or 3 vs >3), and previous receipt of lenalidomide or bortezomib.
In the CASTOR trial, patients received up to eight 21-day cycles of bortezomib, administered subcutaneously at a dose of 1.3 mg/m2 on days 1, 4, 8, and 11 of cycles 1-8, and dexamethasone, administered orally or intravenously at a dose of 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12 for a total dose of 160 mg per cycle. Daratumumab was administered at a dose of 16 mg/kg intravenously once weekly on days 1, 8, and 15 during cycles 1 to 3, once every 3 weeks on day 1 of cycles 4-8, and once every 4 weeks thereafter.
In the POLLUX trial, patients were treated in 28-day cycles. Daratumumab was administered at the same dose as in the CASTOR trial, but on days 1, 8, 15 and 22 for 8 weeks during cycles 1 and 2, every 2 weeks on days 1 and 15 for 16 weeks during cycles 3 through 7, and every 4 weeks from then onwards. Lenalidomide was administered at a dose of 25 mg orally on days 1-21 of each cycle, and dexamethasone at a dose of 20 mg before infusion and 20 mg the following day.
The combination of daratumumab with lenalidomide-dexamethasone demonstrated a substantial improvement in PFS, compared with lenalidomide-dexamethasone alone (estimated PFS not yet reached vs 18.4 months, respectively; HR, 0.37; P < .0001), representing a 63% reduction in the risk of disease progression or death. Meanwhile, there was a 61% reduction in the risk of disease progression or death for the combination of daratumumab with bortezomib-dexamethasone in the CASTOR trial (estimated PFS not yet reached vs 7.2 months; HR: 0.39; P < .0001). The PFS benefit was observed across all prespecified subgroups in both studies.
In the CASTOR trial, over a median follow-up of 7.4 months, the overall response rate (ORR) was 82.9% for the combination arm, compared with 63.2% for the bortezomib-dexamethasone arm (P < .001), with a very good partial response (VGPR) or better rate of 59.2% compared with 29.1%, and a complete response (CR) rate of 19.2% compared with 9%. In the POLLUX trial, over a median follow-up of 13.5 months, ORR was 92.9% for the combination arm, compared with 76.4% for lenalidomide-dexamethasone, with a VGPR or better rate of 75.8% versus 44% and a CR rate of 43.1% versus 19.2%.
Overall, the safety profile for both combinations was consistent with what is usually observed with daratumumab monotherapy and lenalidomide-dexamethasone or bortezomib-dexamethasone combinations. The most frequently reported adverse events (AEs) were similar in both studies and included infusion reactions, diarrhea, and upper respiratory tract infection. In the POLLUX trial they also included nausea, fatigue, pyrexia, muscle spasm, cough, and dyspnea, whereas in the CASTOR trial patients also frequently experienced peripheral edema.
The most common grade 3/4 AEs in both trials were neutropenia (51.9% vs 37% in the POLLUX trial and 12.8 vs 4.2% in the CASTOR trial), thrombocytopenia (12.7% vs 13.5% and 45.3% vs 32.9%, respectively), and anemia (12.4% vs 19.6% and 14.4% vs 16%, respectively). The percentage of patients who discontinued treatment due to AEs was similar in both groups across the two studies; in the CASTOR trial discontinuations resulted most commonly from peripheral sensory neuropathy and pneumonia, while in the POLLUX trial, from pneumonia, pulmonary embolism and deterioration in general physical health.
The recommended dose for daratumumab in both combination regimens is 16 mg/kg intravenously, calculated on actual body weight. The dosing schedules begin with weekly administration during weeks 1-8 (when used in combination with lenalidomide-dexamethasone) and weeks 1-9 (for use with the bortezomib-dexamethasone combination), decreasing to every 2 weeks between weeks 9 and 24 or 10 and 24, respectively, and progressing to every 4 weeks from week 25 onward until disease progression and unacceptable toxicity.
Daratumumab is marketed as Darzalex by Janssen Biotech Inc. Neutropenia and thrombocytopenia have been added to the list of warnings and precautions for the prescribing information for these new indications. Complete blood cell count should be monitored periodically during treatment and daratumumab administration delayed to allow recovery of neutrophils or platelets. Supportive care with growth factors or transfusion should be considered in the event of neutropenia or thrombocytopenia, respectively.
In November 2016, the US Food and Drug Administration expanded the approval of daratumumab for patients with multiple myeloma. The monoclonal antibody, which targets CD38, a protein that is highly expressed on the surface of multiple myeloma cells, was previously granted approval by the agency as a single agent for the treatment of patients who had received at least three previous therapies.
The current approval was for the use of daratumumab in two different combination regimens for the treatment of patients who have received one previous line of treatment. On the basis of improved progression-free survival (PFS), demonstrated in two randomized, open-label, phase 3 trials, daratumumab can now be used in combination with the immunomodulatory agent lenalidomide and dexamethasone, or the proteasome inhibitor bortezomib and dexamethasone, both standard therapies for the treatment of multiple myeloma.
In the POLLUX trial, 569 patients with relapsed/refractory multiple myeloma were randomized 1:1 to receive daratumumab in combination with lenalidomide-dexamethasone or lenalidomide-dexamethasone alone. The CASTOR trial randomized 498 patients with relapsed/refractory multiple myeloma 1:1 to daratumumab in combination with bortezomib-dexamethasone, or bortezomib-dexamethasone alone.
The eligibility and exclusion criteria for both trials were similar; patients had received at least one previous line of therapy, had documented progressive disease according to International Myeloma Working Group criteria, and had measurable disease on the basis of urine and/or serum assessments or serum-free, light-chain assay.
Patients with a neutrophil count of ≤1,000 cells/mm3, hemoglobin level of ≤7.5 g/dL, platelet count of <75,000 cells/mm3, creatinine clearance of ≤20 mL/min per 1.73m2 body surface area (or <30 mL/min in the POLLUX trial), alanine aminotransferase or aspartate aminotransferase level ≥2.5 times the upper limit of normal (ULN) range, bilirubin level of ≥1.5 or more times the ULN range, disease refractory to bortezomib or lenalidomide, and unacceptable side effects from bortezomib or lenalidomide, were ineligible for these studies. In addition, patients with grade 2 or higher peripheral neuropathy or neuropathic pain, were excluded from the CASTOR study.
Randomization was stratified according to International Staging System disease stage at the time of screening (stage I, II or III, with higher stage indicating more severe disease), number of previous lines of therapy (1 vs 2, or 3 vs >3), and previous receipt of lenalidomide or bortezomib.
In the CASTOR trial, patients received up to eight 21-day cycles of bortezomib, administered subcutaneously at a dose of 1.3 mg/m2 on days 1, 4, 8, and 11 of cycles 1-8, and dexamethasone, administered orally or intravenously at a dose of 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12 for a total dose of 160 mg per cycle. Daratumumab was administered at a dose of 16 mg/kg intravenously once weekly on days 1, 8, and 15 during cycles 1 to 3, once every 3 weeks on day 1 of cycles 4-8, and once every 4 weeks thereafter.
In the POLLUX trial, patients were treated in 28-day cycles. Daratumumab was administered at the same dose as in the CASTOR trial, but on days 1, 8, 15 and 22 for 8 weeks during cycles 1 and 2, every 2 weeks on days 1 and 15 for 16 weeks during cycles 3 through 7, and every 4 weeks from then onwards. Lenalidomide was administered at a dose of 25 mg orally on days 1-21 of each cycle, and dexamethasone at a dose of 20 mg before infusion and 20 mg the following day.
The combination of daratumumab with lenalidomide-dexamethasone demonstrated a substantial improvement in PFS, compared with lenalidomide-dexamethasone alone (estimated PFS not yet reached vs 18.4 months, respectively; HR, 0.37; P < .0001), representing a 63% reduction in the risk of disease progression or death. Meanwhile, there was a 61% reduction in the risk of disease progression or death for the combination of daratumumab with bortezomib-dexamethasone in the CASTOR trial (estimated PFS not yet reached vs 7.2 months; HR: 0.39; P < .0001). The PFS benefit was observed across all prespecified subgroups in both studies.
In the CASTOR trial, over a median follow-up of 7.4 months, the overall response rate (ORR) was 82.9% for the combination arm, compared with 63.2% for the bortezomib-dexamethasone arm (P < .001), with a very good partial response (VGPR) or better rate of 59.2% compared with 29.1%, and a complete response (CR) rate of 19.2% compared with 9%. In the POLLUX trial, over a median follow-up of 13.5 months, ORR was 92.9% for the combination arm, compared with 76.4% for lenalidomide-dexamethasone, with a VGPR or better rate of 75.8% versus 44% and a CR rate of 43.1% versus 19.2%.
Overall, the safety profile for both combinations was consistent with what is usually observed with daratumumab monotherapy and lenalidomide-dexamethasone or bortezomib-dexamethasone combinations. The most frequently reported adverse events (AEs) were similar in both studies and included infusion reactions, diarrhea, and upper respiratory tract infection. In the POLLUX trial they also included nausea, fatigue, pyrexia, muscle spasm, cough, and dyspnea, whereas in the CASTOR trial patients also frequently experienced peripheral edema.
The most common grade 3/4 AEs in both trials were neutropenia (51.9% vs 37% in the POLLUX trial and 12.8 vs 4.2% in the CASTOR trial), thrombocytopenia (12.7% vs 13.5% and 45.3% vs 32.9%, respectively), and anemia (12.4% vs 19.6% and 14.4% vs 16%, respectively). The percentage of patients who discontinued treatment due to AEs was similar in both groups across the two studies; in the CASTOR trial discontinuations resulted most commonly from peripheral sensory neuropathy and pneumonia, while in the POLLUX trial, from pneumonia, pulmonary embolism and deterioration in general physical health.
The recommended dose for daratumumab in both combination regimens is 16 mg/kg intravenously, calculated on actual body weight. The dosing schedules begin with weekly administration during weeks 1-8 (when used in combination with lenalidomide-dexamethasone) and weeks 1-9 (for use with the bortezomib-dexamethasone combination), decreasing to every 2 weeks between weeks 9 and 24 or 10 and 24, respectively, and progressing to every 4 weeks from week 25 onward until disease progression and unacceptable toxicity.
Daratumumab is marketed as Darzalex by Janssen Biotech Inc. Neutropenia and thrombocytopenia have been added to the list of warnings and precautions for the prescribing information for these new indications. Complete blood cell count should be monitored periodically during treatment and daratumumab administration delayed to allow recovery of neutrophils or platelets. Supportive care with growth factors or transfusion should be considered in the event of neutropenia or thrombocytopenia, respectively.
1. Darzalex (daratumumab) injection, for intravenous use. Prescribing information. Janssen Biotech Inc. https://www.darzalexhcp.com/shared/product/darzalex/darzalex-prescribing-information.pdf. Released November 2016. Accessed January 8, 2017.
2. Palumbo A, Chanan-Khan A, Weisel K, et al. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:754-766.
3. Dimopoulos MA, Oriol A, Nahi H, et al. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:1319-1331.
1. Darzalex (daratumumab) injection, for intravenous use. Prescribing information. Janssen Biotech Inc. https://www.darzalexhcp.com/shared/product/darzalex/darzalex-prescribing-information.pdf. Released November 2016. Accessed January 8, 2017.
2. Palumbo A, Chanan-Khan A, Weisel K, et al. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:754-766.
3. Dimopoulos MA, Oriol A, Nahi H, et al. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:1319-1331.
Bevacizumab-awwb becomes first biosimilar approved for cancer treatment
Targeted therapies have revolutionized the treatment of numerous different cancer types and ushered in an era of personalized medicine, yet they can be prohibitively costly. As patent protection expires on many of the first FDA-approved monoclonal antibodies developed for oncologic indications, the doors are opened for other companies to develop their own version of these drugs, known as biosimilars. The price of biosimilars is expected to be considerably lower than the original drugs upon which they are based.
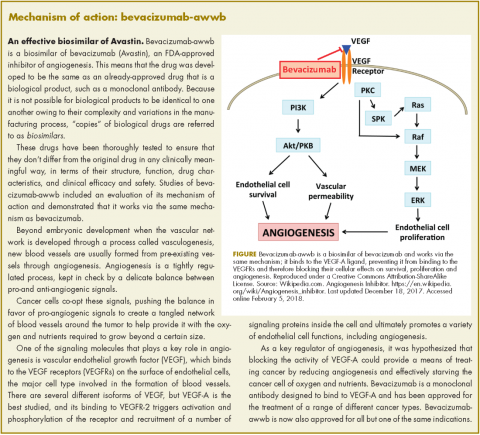
Bevacizumab-awwb, marketed as Mvasi by Amgen and Allergen, became the first such drug to receive approval by the US Food and Drug Administration for the treatment of cancer in fall last year.1 It is a biosimilar of Genentech’s anti-angiogenesis drug, bevacizumab (Avastin), a monoclonal antibody that targets vascular endothelial growth factor-A (VEGF-A).
The approval of biosimilars is based on rigorous demonstration of a high level of similarity between the biosimilar and the already-approved reference drug, in terms of structure, function, pharmacokinetics, pharmacodynamics, and clinical efficacy and safety.
Bevacizumab-awwb was approved for the first- or second-line treatment of metastatic colorectal cancer (mCRC) in combination with 5-fluorouracil-based chemotherapy; the second-line treatment of mCRC in combination with fluoropyrimidine-oxaliplatin chemotherapy in patients who progressed on first-line bevacizumab; the first-line treatment of unresectable, locally advanced, recurrent or metastatic nonsquamous non-small cell lung cancer (NSCLC) in combination with carboplatin and paclitaxel; the second-line treatment of glioblastoma (GBM) as monotherapy; and in patients with persistent, recurrent, or metastatic cervical cancer in combination with paclitaxel and cisplatin or paclitaxel and topotecan. It was not approved for the treatment of ovarian cancer, for which bevacizumab is indicated.
The majority of the data used to support approval came from 2 studies – a 3-arm, single-dose pharmacokinetics study, and a comparative clinical study in patients with advanced/metastatic NSCLC. In the pharmacokinetics study, 202 healthy men received an infusion of 3 mg/kg of bevacizumab-awwb, US-approved bevacizumab, or EU-approved bevacizumab. Bevacizumab-awwb was shown to have pharmacokinetic similarity to both approved forms of bevacizumab, and safety and tolerability were comparable, with none of the participants developing binding or neutralizing antidrug antibodies.2
In the clinical study, 648 patients received an infusion of bevacizumab-awwb or EU-approved bevacizumab at a dose of 15 mg/kg every 3 weeks in combination with 6 AUC carboplatin and 200 mg/m2 paclitaxel for 6 cycles. The overall response rate was 39% for bevacizumab-awwb, compared with 41.7% for EU-bevacizumab, and there were 2 complete responses in each group. The median duration of response for bevacizumab-awwb compared with EU-bevacizumab was 5.8 months versus 5.6 months, respectively, and median progression-free survival was 6.6 months versus 7.9 months.3
In terms of safety, the rates of grade 3/4 adverse events (AEs) were 42.9% in the biosimilar arm, compared with 44.3% for the reference drug. Overall, there were no clinically meaningful differences in AEs, serious AEs, deaths, or treatment discontinuations.
The recommended dose for bevacizumab-awwb in patients with mCRC is a 5 mg/kg intravenous dose administered every 2 weeks with bolus-IFL, a 10 mg/kg IV dose administered every 2 weeks with FOLFOX4, or a 5 mg/kg IV dose administered every 2 weeks or 7.5 mg/kg IV dose administered every 3 weeks with fluoropyrimidine-irinotecan or fluoropyrimidine-oxaliplatin-based chemotherapy.
For patients with NSCLC, bevacizumab-awwb should be administered at a 15 mg/kg IV dose every 3 weeks with the carboplatin–paclitaxel combination; for GBM patients, a 10 mg/kg IV dose should be administered every 3 weeks; and for patients with cervical cancer, an IV dose of 15 mg/kg every 3 weeks in combination with paclitaxel–cisplatin or paclitaxel–topotecan is recommended.
The prescribing information outlines warnings and precautions to advise clinicians administering the new biosimilar of the risks of gastrointestinal (GI) perforations, surgery and wound healing complications, and severe and potentially fatal pulmonary, GI, central nervous system, and vaginal bleeding.4
Treatment should be discontinued if GI perforation occurs. Patients should not take bevacizumab-awwb in the 28 days before elective surgery and after surgery until the wound is healed, and treatment should be discontinued if the surgical wound breaks open. Bevacizumab-awwb should not be administered to patients with severe hemorrhage or those with hemoptysis.
Blood pressure should be monitored every 2-3 weeks during treatment and hypertension treated with antihypertensive therapy. Treatment should be temporarily suspended in patients with severe hypertension that is not controlled with antihypertensive therapy and discontinued in patients who experience hypertensive crisis or hypertensive encephalopathy.
Proteinuria should be monitored by dipstick urine analysis during treatment, and patients with a 2+ or greater reading (concentration, 100 mg/dL) should undergo further assessment with 24-hour urine collection. Treatment should be suspended if proteinuria levels are ≥2 g/24h and can be resumed when they fall below that level, but should be discontinued in patients with nephrotic syndrome. Treatment should also be discontinued in patients who develop posterior reversible encephalopathy syndrome, and patients should be advised of the potential for fetal harm
1. FDA approves first biosimilar for the treatment of cancer. FDA News Release. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm576112.htm. September 14, 2017. Accessed January 31, 2018.
2. Markus R, Chow V, Pan X, and Hanes V. A phase I, randomized, single-dose study evaluating the pharmacokinetic equivalence of biosimilar ABP 215 and bevacizumab in healthy adult men. Cancer Chemother. Pharmacol. 2017;80:755-763.
3. Thatcher N, Thomas M, Ostoros G, et al. Randomized, double-blind, phase 3 study comparing biosimilar candidate ABP-215 with bevacizumab in patients with non-squamous NSCLC. J Thorac Oncol. 2017;12(1):S902-S903.
4. Mvasi (bevacizumab-awwb) solution, for intravenous infusion. Prescribing information. Amgen Inc, https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761028s000lbl.pdf. September 2017. Accessed January 31, 2018.
Targeted therapies have revolutionized the treatment of numerous different cancer types and ushered in an era of personalized medicine, yet they can be prohibitively costly. As patent protection expires on many of the first FDA-approved monoclonal antibodies developed for oncologic indications, the doors are opened for other companies to develop their own version of these drugs, known as biosimilars. The price of biosimilars is expected to be considerably lower than the original drugs upon which they are based.
Bevacizumab-awwb, marketed as Mvasi by Amgen and Allergen, became the first such drug to receive approval by the US Food and Drug Administration for the treatment of cancer in fall last year.1 It is a biosimilar of Genentech’s anti-angiogenesis drug, bevacizumab (Avastin), a monoclonal antibody that targets vascular endothelial growth factor-A (VEGF-A).
The approval of biosimilars is based on rigorous demonstration of a high level of similarity between the biosimilar and the already-approved reference drug, in terms of structure, function, pharmacokinetics, pharmacodynamics, and clinical efficacy and safety.
Bevacizumab-awwb was approved for the first- or second-line treatment of metastatic colorectal cancer (mCRC) in combination with 5-fluorouracil-based chemotherapy; the second-line treatment of mCRC in combination with fluoropyrimidine-oxaliplatin chemotherapy in patients who progressed on first-line bevacizumab; the first-line treatment of unresectable, locally advanced, recurrent or metastatic nonsquamous non-small cell lung cancer (NSCLC) in combination with carboplatin and paclitaxel; the second-line treatment of glioblastoma (GBM) as monotherapy; and in patients with persistent, recurrent, or metastatic cervical cancer in combination with paclitaxel and cisplatin or paclitaxel and topotecan. It was not approved for the treatment of ovarian cancer, for which bevacizumab is indicated.
The majority of the data used to support approval came from 2 studies – a 3-arm, single-dose pharmacokinetics study, and a comparative clinical study in patients with advanced/metastatic NSCLC. In the pharmacokinetics study, 202 healthy men received an infusion of 3 mg/kg of bevacizumab-awwb, US-approved bevacizumab, or EU-approved bevacizumab. Bevacizumab-awwb was shown to have pharmacokinetic similarity to both approved forms of bevacizumab, and safety and tolerability were comparable, with none of the participants developing binding or neutralizing antidrug antibodies.2
In the clinical study, 648 patients received an infusion of bevacizumab-awwb or EU-approved bevacizumab at a dose of 15 mg/kg every 3 weeks in combination with 6 AUC carboplatin and 200 mg/m2 paclitaxel for 6 cycles. The overall response rate was 39% for bevacizumab-awwb, compared with 41.7% for EU-bevacizumab, and there were 2 complete responses in each group. The median duration of response for bevacizumab-awwb compared with EU-bevacizumab was 5.8 months versus 5.6 months, respectively, and median progression-free survival was 6.6 months versus 7.9 months.3
In terms of safety, the rates of grade 3/4 adverse events (AEs) were 42.9% in the biosimilar arm, compared with 44.3% for the reference drug. Overall, there were no clinically meaningful differences in AEs, serious AEs, deaths, or treatment discontinuations.
The recommended dose for bevacizumab-awwb in patients with mCRC is a 5 mg/kg intravenous dose administered every 2 weeks with bolus-IFL, a 10 mg/kg IV dose administered every 2 weeks with FOLFOX4, or a 5 mg/kg IV dose administered every 2 weeks or 7.5 mg/kg IV dose administered every 3 weeks with fluoropyrimidine-irinotecan or fluoropyrimidine-oxaliplatin-based chemotherapy.
For patients with NSCLC, bevacizumab-awwb should be administered at a 15 mg/kg IV dose every 3 weeks with the carboplatin–paclitaxel combination; for GBM patients, a 10 mg/kg IV dose should be administered every 3 weeks; and for patients with cervical cancer, an IV dose of 15 mg/kg every 3 weeks in combination with paclitaxel–cisplatin or paclitaxel–topotecan is recommended.
The prescribing information outlines warnings and precautions to advise clinicians administering the new biosimilar of the risks of gastrointestinal (GI) perforations, surgery and wound healing complications, and severe and potentially fatal pulmonary, GI, central nervous system, and vaginal bleeding.4
Treatment should be discontinued if GI perforation occurs. Patients should not take bevacizumab-awwb in the 28 days before elective surgery and after surgery until the wound is healed, and treatment should be discontinued if the surgical wound breaks open. Bevacizumab-awwb should not be administered to patients with severe hemorrhage or those with hemoptysis.
Blood pressure should be monitored every 2-3 weeks during treatment and hypertension treated with antihypertensive therapy. Treatment should be temporarily suspended in patients with severe hypertension that is not controlled with antihypertensive therapy and discontinued in patients who experience hypertensive crisis or hypertensive encephalopathy.
Proteinuria should be monitored by dipstick urine analysis during treatment, and patients with a 2+ or greater reading (concentration, 100 mg/dL) should undergo further assessment with 24-hour urine collection. Treatment should be suspended if proteinuria levels are ≥2 g/24h and can be resumed when they fall below that level, but should be discontinued in patients with nephrotic syndrome. Treatment should also be discontinued in patients who develop posterior reversible encephalopathy syndrome, and patients should be advised of the potential for fetal harm
Targeted therapies have revolutionized the treatment of numerous different cancer types and ushered in an era of personalized medicine, yet they can be prohibitively costly. As patent protection expires on many of the first FDA-approved monoclonal antibodies developed for oncologic indications, the doors are opened for other companies to develop their own version of these drugs, known as biosimilars. The price of biosimilars is expected to be considerably lower than the original drugs upon which they are based.
Bevacizumab-awwb, marketed as Mvasi by Amgen and Allergen, became the first such drug to receive approval by the US Food and Drug Administration for the treatment of cancer in fall last year.1 It is a biosimilar of Genentech’s anti-angiogenesis drug, bevacizumab (Avastin), a monoclonal antibody that targets vascular endothelial growth factor-A (VEGF-A).
The approval of biosimilars is based on rigorous demonstration of a high level of similarity between the biosimilar and the already-approved reference drug, in terms of structure, function, pharmacokinetics, pharmacodynamics, and clinical efficacy and safety.
Bevacizumab-awwb was approved for the first- or second-line treatment of metastatic colorectal cancer (mCRC) in combination with 5-fluorouracil-based chemotherapy; the second-line treatment of mCRC in combination with fluoropyrimidine-oxaliplatin chemotherapy in patients who progressed on first-line bevacizumab; the first-line treatment of unresectable, locally advanced, recurrent or metastatic nonsquamous non-small cell lung cancer (NSCLC) in combination with carboplatin and paclitaxel; the second-line treatment of glioblastoma (GBM) as monotherapy; and in patients with persistent, recurrent, or metastatic cervical cancer in combination with paclitaxel and cisplatin or paclitaxel and topotecan. It was not approved for the treatment of ovarian cancer, for which bevacizumab is indicated.
The majority of the data used to support approval came from 2 studies – a 3-arm, single-dose pharmacokinetics study, and a comparative clinical study in patients with advanced/metastatic NSCLC. In the pharmacokinetics study, 202 healthy men received an infusion of 3 mg/kg of bevacizumab-awwb, US-approved bevacizumab, or EU-approved bevacizumab. Bevacizumab-awwb was shown to have pharmacokinetic similarity to both approved forms of bevacizumab, and safety and tolerability were comparable, with none of the participants developing binding or neutralizing antidrug antibodies.2
In the clinical study, 648 patients received an infusion of bevacizumab-awwb or EU-approved bevacizumab at a dose of 15 mg/kg every 3 weeks in combination with 6 AUC carboplatin and 200 mg/m2 paclitaxel for 6 cycles. The overall response rate was 39% for bevacizumab-awwb, compared with 41.7% for EU-bevacizumab, and there were 2 complete responses in each group. The median duration of response for bevacizumab-awwb compared with EU-bevacizumab was 5.8 months versus 5.6 months, respectively, and median progression-free survival was 6.6 months versus 7.9 months.3
In terms of safety, the rates of grade 3/4 adverse events (AEs) were 42.9% in the biosimilar arm, compared with 44.3% for the reference drug. Overall, there were no clinically meaningful differences in AEs, serious AEs, deaths, or treatment discontinuations.
The recommended dose for bevacizumab-awwb in patients with mCRC is a 5 mg/kg intravenous dose administered every 2 weeks with bolus-IFL, a 10 mg/kg IV dose administered every 2 weeks with FOLFOX4, or a 5 mg/kg IV dose administered every 2 weeks or 7.5 mg/kg IV dose administered every 3 weeks with fluoropyrimidine-irinotecan or fluoropyrimidine-oxaliplatin-based chemotherapy.
For patients with NSCLC, bevacizumab-awwb should be administered at a 15 mg/kg IV dose every 3 weeks with the carboplatin–paclitaxel combination; for GBM patients, a 10 mg/kg IV dose should be administered every 3 weeks; and for patients with cervical cancer, an IV dose of 15 mg/kg every 3 weeks in combination with paclitaxel–cisplatin or paclitaxel–topotecan is recommended.
The prescribing information outlines warnings and precautions to advise clinicians administering the new biosimilar of the risks of gastrointestinal (GI) perforations, surgery and wound healing complications, and severe and potentially fatal pulmonary, GI, central nervous system, and vaginal bleeding.4
Treatment should be discontinued if GI perforation occurs. Patients should not take bevacizumab-awwb in the 28 days before elective surgery and after surgery until the wound is healed, and treatment should be discontinued if the surgical wound breaks open. Bevacizumab-awwb should not be administered to patients with severe hemorrhage or those with hemoptysis.
Blood pressure should be monitored every 2-3 weeks during treatment and hypertension treated with antihypertensive therapy. Treatment should be temporarily suspended in patients with severe hypertension that is not controlled with antihypertensive therapy and discontinued in patients who experience hypertensive crisis or hypertensive encephalopathy.
Proteinuria should be monitored by dipstick urine analysis during treatment, and patients with a 2+ or greater reading (concentration, 100 mg/dL) should undergo further assessment with 24-hour urine collection. Treatment should be suspended if proteinuria levels are ≥2 g/24h and can be resumed when they fall below that level, but should be discontinued in patients with nephrotic syndrome. Treatment should also be discontinued in patients who develop posterior reversible encephalopathy syndrome, and patients should be advised of the potential for fetal harm
1. FDA approves first biosimilar for the treatment of cancer. FDA News Release. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm576112.htm. September 14, 2017. Accessed January 31, 2018.
2. Markus R, Chow V, Pan X, and Hanes V. A phase I, randomized, single-dose study evaluating the pharmacokinetic equivalence of biosimilar ABP 215 and bevacizumab in healthy adult men. Cancer Chemother. Pharmacol. 2017;80:755-763.
3. Thatcher N, Thomas M, Ostoros G, et al. Randomized, double-blind, phase 3 study comparing biosimilar candidate ABP-215 with bevacizumab in patients with non-squamous NSCLC. J Thorac Oncol. 2017;12(1):S902-S903.
4. Mvasi (bevacizumab-awwb) solution, for intravenous infusion. Prescribing information. Amgen Inc, https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761028s000lbl.pdf. September 2017. Accessed January 31, 2018.
1. FDA approves first biosimilar for the treatment of cancer. FDA News Release. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm576112.htm. September 14, 2017. Accessed January 31, 2018.
2. Markus R, Chow V, Pan X, and Hanes V. A phase I, randomized, single-dose study evaluating the pharmacokinetic equivalence of biosimilar ABP 215 and bevacizumab in healthy adult men. Cancer Chemother. Pharmacol. 2017;80:755-763.
3. Thatcher N, Thomas M, Ostoros G, et al. Randomized, double-blind, phase 3 study comparing biosimilar candidate ABP-215 with bevacizumab in patients with non-squamous NSCLC. J Thorac Oncol. 2017;12(1):S902-S903.
4. Mvasi (bevacizumab-awwb) solution, for intravenous infusion. Prescribing information. Amgen Inc, https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761028s000lbl.pdf. September 2017. Accessed January 31, 2018.
Trastuzumab-dkst approval adds to the biosimilar cancer drug market
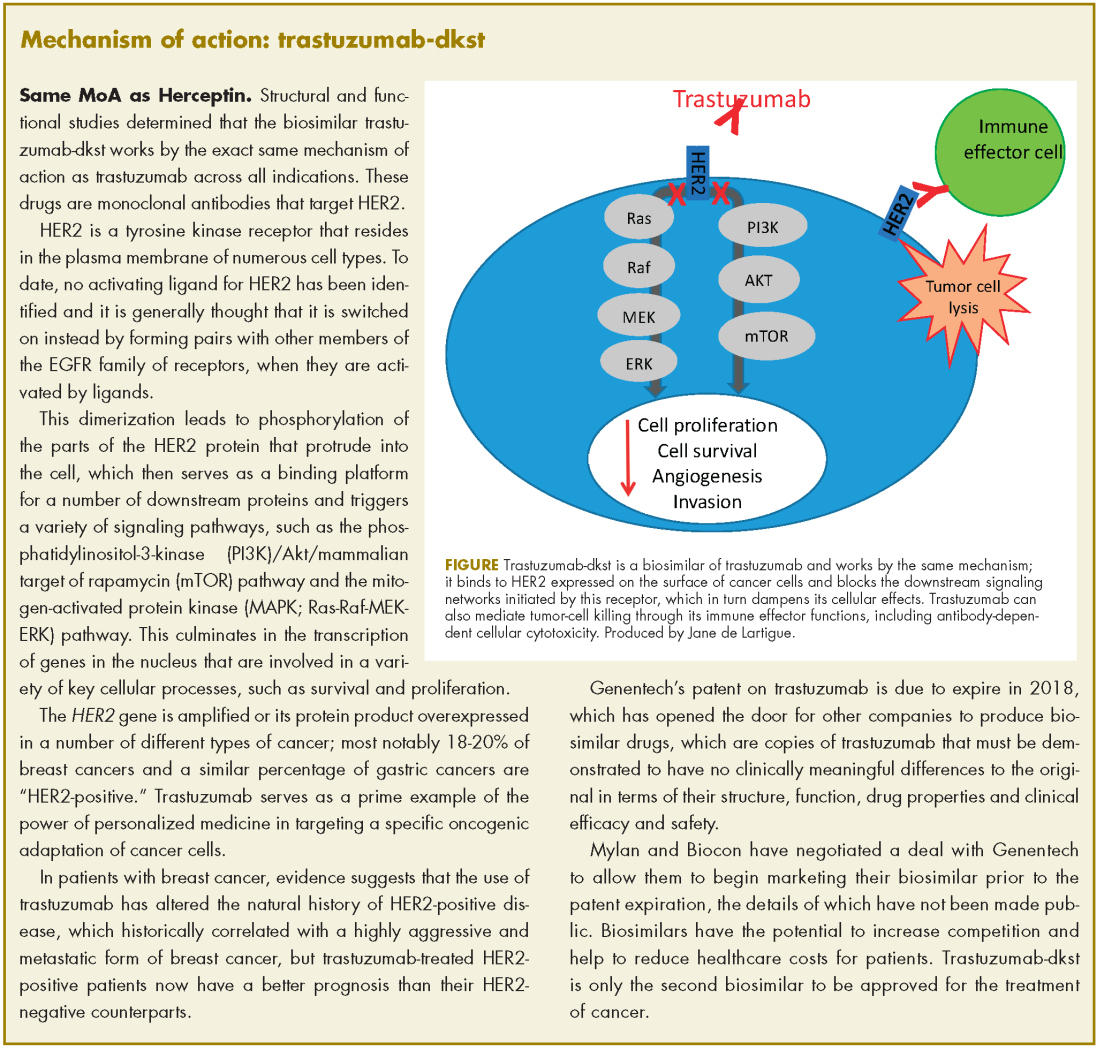
The human epidermal growth factor receptor-2 (HER2)-targeting monoclonal antibody trastuzumab-dkst, was approved by the US Food and Drug Administration in 2017 for the treatment of patients with HER2-positive breast or metastatic gastric or gastroesophageal junction adenocarcinoma.1 Trastuzumab-dkst, marketed as Ogviri by Mylan NV and Biocon Ltd, is a copy, known as a biosimilar, of Genentech’s trastuzumab (Herceptin), which has been approved in the US since 1998. Genentech’s patent on trastuzumab expires in 2018
Approval was based on a comparison of the 2 drugs, which demonstrated that there were no clinically meaningful differences between the biosimilar and the reference product (trastuzumab) in terms of structure and function, pharmacokinetics (PKs), pharmacodynamics, and clinical efficacy and safety.
In structural and functional studies, trastuzumab-dkst was shown to have an identical amino acid sequence and a highly similar 3-dimensional structure, as well as equivalency in an inhibition of proliferation assay, a HER2-binding assay, and an antibody-dependent cellular cytotoxicity assay, compared with trastuzumab.
Two nonclinical animal studies were performed in cynomolgus monkeys; a single-dose comparative PK study and a 4-week, repeat-dose toxicity study. That was further supported by data from a single-dose, randomized, double-blind, comparative 3-way PK study (MYL-HER-1002) in which 120 healthy men were given an 8 mg/kg infusion of trastuzumab-dkst, US-approved trastuzumab, or European Union (EU)-approved trastuzumab.
The key clinical study was the phase 3 HERiTAge trial, a 2-part, multicenter, double-blind, randomized, parallel group trial that was performed in patients with HER2-positive metastatic breast cancer who had not been previously treated with either chemotherapy or trastuzumab in the metastatic setting.2
Eligible patients included males or females with measurably HER2-positive disease (as defined by HER2 overexpression determined by immunohistochemistry performed by a central laboratory), no exposure to chemotherapy or trastuzumab in the metastatic setting, an Eastern Cooperative Oncology Group Performance Status of 0 or 2, left ventricular ejection fraction (LVEF) within institutional range of normal, and who had completed adjuvant trastuzumab therapy at least 1 year before.
Patients with central nervous system metastases had to have stable disease after treatment, and hormonal agents were required to be discontinued before the start of the study. Patients with a history of unstable angina, heart failure, myocardial infarction less than 1 year from randomization, other clinically significant cardiac disease, grade 2 or higher peripheral neuropathy, a history of any other cancer within 4 years before screening, or any significant medical illness that increased treatment risk or impeded evaluation, were excluded from the study.
Patients were randomly assigned 1:1 to receive trastuzumab-dkst or trastuzumab, both in combination with paclitaxel or docetaxel, at a loading dose of 8 mg/kg, followed by a maintenance dose of 6 mg/kg, every 3 weeks for a minimum of 7 cycles in part 1 of the study. Patients who had stable disease or better were enrolled in part 2 and continued treatment until disease progression or unacceptable toxicity.
The primary endpoint was overall response rate (ORR) and, after 24 weeks, the ORR was 69.6% in the trastuzumab-dkst arm, compared with 64% in the trastuzumab arm, with a ratio of ORR of 1.09. Progression-free survival was also nearly identical in the 2 groups and median overall survival had not been reached in either arm.
The safety of the biosimilar and reference product were also highly similar. Serious adverse events occurred in 39.3%, compared with 37% of patients, respectively, with neutropenia the most frequently reported in both arms. Overall, treatment-emergent AEs occurred in 96.8%, compared with 94.7% of patients, respectively, with the majority of events mild or moderate in severity in both groups. This study also confirmed the low immunogenicity of the 2 drug products.
The prescribing information details the recommended doses of trastuzumab-dkst for each approved indication and warnings and precautions for cardiomyopathy, infusion reactions, pulmonary toxicity, exacerbation of chemotherapy-induced neutropenia and embryofetal toxicity.3
Patients should undergo thorough cardiac assessments, including baseline LVEF measurement immediately before starting therapy, every 3 months during therapy, and upon completion of therapy. Patients who complete adjuvant therapy should have cardiac assessments every 6 months for at least 2 years. Treatment should be withheld for ≥16% absolute decrease in LVEF from pre-treatment values or an LVEF value below institutional limits of normal and ≥10% absolute decrease in LVEF from pre-treatment values. When treatment is withheld for significant LVEF cardiac dysfunction, patients should undergo cardiac assessment at 4-week intervals.
To combat infusion reactions, infusion should be interrupted in all patients experiencing dyspnea or clinically significant hypotension and medical therapy administered. Patients should be evaluated and monitored carefully until signs and symptoms resolve and permanent discontinuation considered in patients with severe reactions. Patients should be warned of the potential for fetal harm with trastuzumab-dkst and of the need for effective contraceptive use during and for 6 months after treatment
1. FDA approves first biosimilar for the treatment of certain breast and stomach cancers. FDA News Release. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm587378.htm. December 1, 2017. Accessed January 31, 2018.
2. Rugo HS, Barve A, Waller CF, et al. Effect of a proposed trastuzumab biosimilar compared with trastuzumab on overall response rate in patients with ERBB2 (HER2)-positive metastatic breast cancer: a randomized clinical trial. JAMA. 2017;317(1):37-47.
3. Ogviri (trastuzumab-dkst) injection, for intravenous use. Prescribing information. Mylan, GMBH. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761074s000lbl.pdf. December, 2017. Accessed July 31, 2015.
The human epidermal growth factor receptor-2 (HER2)-targeting monoclonal antibody trastuzumab-dkst, was approved by the US Food and Drug Administration in 2017 for the treatment of patients with HER2-positive breast or metastatic gastric or gastroesophageal junction adenocarcinoma.1 Trastuzumab-dkst, marketed as Ogviri by Mylan NV and Biocon Ltd, is a copy, known as a biosimilar, of Genentech’s trastuzumab (Herceptin), which has been approved in the US since 1998. Genentech’s patent on trastuzumab expires in 2018
Approval was based on a comparison of the 2 drugs, which demonstrated that there were no clinically meaningful differences between the biosimilar and the reference product (trastuzumab) in terms of structure and function, pharmacokinetics (PKs), pharmacodynamics, and clinical efficacy and safety.
In structural and functional studies, trastuzumab-dkst was shown to have an identical amino acid sequence and a highly similar 3-dimensional structure, as well as equivalency in an inhibition of proliferation assay, a HER2-binding assay, and an antibody-dependent cellular cytotoxicity assay, compared with trastuzumab.
Two nonclinical animal studies were performed in cynomolgus monkeys; a single-dose comparative PK study and a 4-week, repeat-dose toxicity study. That was further supported by data from a single-dose, randomized, double-blind, comparative 3-way PK study (MYL-HER-1002) in which 120 healthy men were given an 8 mg/kg infusion of trastuzumab-dkst, US-approved trastuzumab, or European Union (EU)-approved trastuzumab.
The key clinical study was the phase 3 HERiTAge trial, a 2-part, multicenter, double-blind, randomized, parallel group trial that was performed in patients with HER2-positive metastatic breast cancer who had not been previously treated with either chemotherapy or trastuzumab in the metastatic setting.2
Eligible patients included males or females with measurably HER2-positive disease (as defined by HER2 overexpression determined by immunohistochemistry performed by a central laboratory), no exposure to chemotherapy or trastuzumab in the metastatic setting, an Eastern Cooperative Oncology Group Performance Status of 0 or 2, left ventricular ejection fraction (LVEF) within institutional range of normal, and who had completed adjuvant trastuzumab therapy at least 1 year before.
Patients with central nervous system metastases had to have stable disease after treatment, and hormonal agents were required to be discontinued before the start of the study. Patients with a history of unstable angina, heart failure, myocardial infarction less than 1 year from randomization, other clinically significant cardiac disease, grade 2 or higher peripheral neuropathy, a history of any other cancer within 4 years before screening, or any significant medical illness that increased treatment risk or impeded evaluation, were excluded from the study.
Patients were randomly assigned 1:1 to receive trastuzumab-dkst or trastuzumab, both in combination with paclitaxel or docetaxel, at a loading dose of 8 mg/kg, followed by a maintenance dose of 6 mg/kg, every 3 weeks for a minimum of 7 cycles in part 1 of the study. Patients who had stable disease or better were enrolled in part 2 and continued treatment until disease progression or unacceptable toxicity.
The primary endpoint was overall response rate (ORR) and, after 24 weeks, the ORR was 69.6% in the trastuzumab-dkst arm, compared with 64% in the trastuzumab arm, with a ratio of ORR of 1.09. Progression-free survival was also nearly identical in the 2 groups and median overall survival had not been reached in either arm.
The safety of the biosimilar and reference product were also highly similar. Serious adverse events occurred in 39.3%, compared with 37% of patients, respectively, with neutropenia the most frequently reported in both arms. Overall, treatment-emergent AEs occurred in 96.8%, compared with 94.7% of patients, respectively, with the majority of events mild or moderate in severity in both groups. This study also confirmed the low immunogenicity of the 2 drug products.
The prescribing information details the recommended doses of trastuzumab-dkst for each approved indication and warnings and precautions for cardiomyopathy, infusion reactions, pulmonary toxicity, exacerbation of chemotherapy-induced neutropenia and embryofetal toxicity.3
Patients should undergo thorough cardiac assessments, including baseline LVEF measurement immediately before starting therapy, every 3 months during therapy, and upon completion of therapy. Patients who complete adjuvant therapy should have cardiac assessments every 6 months for at least 2 years. Treatment should be withheld for ≥16% absolute decrease in LVEF from pre-treatment values or an LVEF value below institutional limits of normal and ≥10% absolute decrease in LVEF from pre-treatment values. When treatment is withheld for significant LVEF cardiac dysfunction, patients should undergo cardiac assessment at 4-week intervals.
To combat infusion reactions, infusion should be interrupted in all patients experiencing dyspnea or clinically significant hypotension and medical therapy administered. Patients should be evaluated and monitored carefully until signs and symptoms resolve and permanent discontinuation considered in patients with severe reactions. Patients should be warned of the potential for fetal harm with trastuzumab-dkst and of the need for effective contraceptive use during and for 6 months after treatment
The human epidermal growth factor receptor-2 (HER2)-targeting monoclonal antibody trastuzumab-dkst, was approved by the US Food and Drug Administration in 2017 for the treatment of patients with HER2-positive breast or metastatic gastric or gastroesophageal junction adenocarcinoma.1 Trastuzumab-dkst, marketed as Ogviri by Mylan NV and Biocon Ltd, is a copy, known as a biosimilar, of Genentech’s trastuzumab (Herceptin), which has been approved in the US since 1998. Genentech’s patent on trastuzumab expires in 2018
Approval was based on a comparison of the 2 drugs, which demonstrated that there were no clinically meaningful differences between the biosimilar and the reference product (trastuzumab) in terms of structure and function, pharmacokinetics (PKs), pharmacodynamics, and clinical efficacy and safety.
In structural and functional studies, trastuzumab-dkst was shown to have an identical amino acid sequence and a highly similar 3-dimensional structure, as well as equivalency in an inhibition of proliferation assay, a HER2-binding assay, and an antibody-dependent cellular cytotoxicity assay, compared with trastuzumab.
Two nonclinical animal studies were performed in cynomolgus monkeys; a single-dose comparative PK study and a 4-week, repeat-dose toxicity study. That was further supported by data from a single-dose, randomized, double-blind, comparative 3-way PK study (MYL-HER-1002) in which 120 healthy men were given an 8 mg/kg infusion of trastuzumab-dkst, US-approved trastuzumab, or European Union (EU)-approved trastuzumab.
The key clinical study was the phase 3 HERiTAge trial, a 2-part, multicenter, double-blind, randomized, parallel group trial that was performed in patients with HER2-positive metastatic breast cancer who had not been previously treated with either chemotherapy or trastuzumab in the metastatic setting.2
Eligible patients included males or females with measurably HER2-positive disease (as defined by HER2 overexpression determined by immunohistochemistry performed by a central laboratory), no exposure to chemotherapy or trastuzumab in the metastatic setting, an Eastern Cooperative Oncology Group Performance Status of 0 or 2, left ventricular ejection fraction (LVEF) within institutional range of normal, and who had completed adjuvant trastuzumab therapy at least 1 year before.
Patients with central nervous system metastases had to have stable disease after treatment, and hormonal agents were required to be discontinued before the start of the study. Patients with a history of unstable angina, heart failure, myocardial infarction less than 1 year from randomization, other clinically significant cardiac disease, grade 2 or higher peripheral neuropathy, a history of any other cancer within 4 years before screening, or any significant medical illness that increased treatment risk or impeded evaluation, were excluded from the study.
Patients were randomly assigned 1:1 to receive trastuzumab-dkst or trastuzumab, both in combination with paclitaxel or docetaxel, at a loading dose of 8 mg/kg, followed by a maintenance dose of 6 mg/kg, every 3 weeks for a minimum of 7 cycles in part 1 of the study. Patients who had stable disease or better were enrolled in part 2 and continued treatment until disease progression or unacceptable toxicity.
The primary endpoint was overall response rate (ORR) and, after 24 weeks, the ORR was 69.6% in the trastuzumab-dkst arm, compared with 64% in the trastuzumab arm, with a ratio of ORR of 1.09. Progression-free survival was also nearly identical in the 2 groups and median overall survival had not been reached in either arm.
The safety of the biosimilar and reference product were also highly similar. Serious adverse events occurred in 39.3%, compared with 37% of patients, respectively, with neutropenia the most frequently reported in both arms. Overall, treatment-emergent AEs occurred in 96.8%, compared with 94.7% of patients, respectively, with the majority of events mild or moderate in severity in both groups. This study also confirmed the low immunogenicity of the 2 drug products.
The prescribing information details the recommended doses of trastuzumab-dkst for each approved indication and warnings and precautions for cardiomyopathy, infusion reactions, pulmonary toxicity, exacerbation of chemotherapy-induced neutropenia and embryofetal toxicity.3
Patients should undergo thorough cardiac assessments, including baseline LVEF measurement immediately before starting therapy, every 3 months during therapy, and upon completion of therapy. Patients who complete adjuvant therapy should have cardiac assessments every 6 months for at least 2 years. Treatment should be withheld for ≥16% absolute decrease in LVEF from pre-treatment values or an LVEF value below institutional limits of normal and ≥10% absolute decrease in LVEF from pre-treatment values. When treatment is withheld for significant LVEF cardiac dysfunction, patients should undergo cardiac assessment at 4-week intervals.
To combat infusion reactions, infusion should be interrupted in all patients experiencing dyspnea or clinically significant hypotension and medical therapy administered. Patients should be evaluated and monitored carefully until signs and symptoms resolve and permanent discontinuation considered in patients with severe reactions. Patients should be warned of the potential for fetal harm with trastuzumab-dkst and of the need for effective contraceptive use during and for 6 months after treatment
1. FDA approves first biosimilar for the treatment of certain breast and stomach cancers. FDA News Release. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm587378.htm. December 1, 2017. Accessed January 31, 2018.
2. Rugo HS, Barve A, Waller CF, et al. Effect of a proposed trastuzumab biosimilar compared with trastuzumab on overall response rate in patients with ERBB2 (HER2)-positive metastatic breast cancer: a randomized clinical trial. JAMA. 2017;317(1):37-47.
3. Ogviri (trastuzumab-dkst) injection, for intravenous use. Prescribing information. Mylan, GMBH. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761074s000lbl.pdf. December, 2017. Accessed July 31, 2015.
1. FDA approves first biosimilar for the treatment of certain breast and stomach cancers. FDA News Release. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm587378.htm. December 1, 2017. Accessed January 31, 2018.
2. Rugo HS, Barve A, Waller CF, et al. Effect of a proposed trastuzumab biosimilar compared with trastuzumab on overall response rate in patients with ERBB2 (HER2)-positive metastatic breast cancer: a randomized clinical trial. JAMA. 2017;317(1):37-47.
3. Ogviri (trastuzumab-dkst) injection, for intravenous use. Prescribing information. Mylan, GMBH. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761074s000lbl.pdf. December, 2017. Accessed July 31, 2015.
Abemaciclib becomes first CDK inhibitor to clinch single-agent approval for breast cancer
The fall 2017 approval by the US Food and Drug Administration (FDA) of abemaciclib made it the third cyclin-dependent kinase (CDK) inhibitor approved for the treatment of hormone receptor (HR)-positive breast cancer, and the first to receive an approved indication as monotherapy in that setting. Abemaciclib is a small-molecule inhibitor of the CDK4 and CDK6 proteins, which are key gatekeepers of the cell cycle and frequently dysregulated in HR-positive breast cancer. On the basis of the randomized, placebo-controlled, multicenter phase 3 MONARCH-2 trial, it was approved in combination with fulvestrant for the treatment of women with HR-positive, HER2-negative advanced or metastatic breast cancer who had progressed during endocrine therapy.1
A total of 669 women aged 18 years and older, with any menopausal status, an Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 or 1, measurable disease per Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1) or nonmeasurable bone-only disease, were enrolled. Patients had progressed during neoadjuvant or adjuvant endocrine therapy, within 12 months of adjuvant endocrine therapy, or during frontline endocrine treatment for metastatic disease.
Those who had received more than 1 endocrine therapy or any prior chemotherapy for metastatic breast cancer or prior treatment with everolimus or CDK4/6 inhibitors, as well as those with the presence of visceral crisis or evidence or history of central nervous system (CNS) metastases, were excluded from the study.
Patients were randomized 2:1 to receive 150 mg abemaciclib or placebo, both in combination with 500 mg fulvestrant. The initial dose of abemaciclib was 200 mg, but this was amended to 150mg after enrollment of the first 178 patients to alleviate diarrhea-related toxicity concerns. Randomization was stratified according to metastatic site (visceral, bone only, or other) and endocrine therapy resistance (primary or secondary).
Tumors were measured by computed tomography (CT) and magnetic-resonance imaging (MRI) according to RECIST-1.1 within 28 days before random assignment, every 8 weeks for the first year, every 12 weeks thereafter, and then within 2 weeks of clinical progression. Bone scintigraphy was also performed at baseline and then every 6th cycle starting with cycle 7. Hematologic and blood chemistry laboratory tests were performed centrally on days 1 and 15 of the first cycle and day 1 of all remaining cycles.
The primary endpoint was progression-free survival (PFS); median PFS was 16.4 months in the abemaciclib arm, compared with 9.3 months in the placebo arm in the intent-to-treat population (hazard ratio [HR], 0.553;P < .0000001), translating to a 45% reduction in the risk of disease progression or death with the combination. Objective response rate in the 2 groups among patients with measurable disease was 48.1% and 21.3%, respectively, which included a complete response rate of 3.5% in the abemaciclib arm. The median duration of response was not yet reached in the study group, compared with 25.6 months for placebo. Overall survival data were not yet mature.
The agency also approved abemaciclib as monotherapy for women and men with HR-positive, HER2-negative advanced or metastatic breast cancer with disease progression following endocrine therapy and prior chemotherapy in the metastatic setting. That approval was based on data from the single-arm MONARCH-1 trial of 132 patients who received 200 mg abemaciclib twice daily on a continuous schedule.2
Patients had adequate organ function, measurable disease per RECIST-1.1, and an ECOG performance status of 0 or 1. Patients must have progressed on or after previous endocrine therapy and have received prior treatment with at least 2 chemotherapy regimens, at least 1 of them, but no more than 2, having been administered in the metastatic setting. Exclusion criteria included prior receipt of a CDK inhibitor, major surgery within 14 days of the start of the study, and CNS metastases.
Tumor assessments were performed by CT or MRI according to RECIST-1.1 within the 4 weeks prior to the first dose of study drug and then subsequently at every other cycle. Responses were confirmed at least 4 weeks after the initial observation. The overall response rate was 19.7%, made up completely of partial responses. Median duration of response was 8.6 months, median PFS was 6 months and median OS was 17.7 months.
Adverse events
The most common adverse events experienced with the combination of abemaciclib and fulvestrant were neutropenia (23.6%) and diarrhea (13.4%). The rate of grade 4 neutropenia was higher in the combination arm (2.9% vs 0.4%) and there were 3 deaths with the combination that were linked to treatment-related AEs. In the monotherapy trial, abemaciclib treatment most commonly caused diarrhea (90.2%), fatigue (65.2%), nausea (64.4%), decreased appetite (45.5%), and abdominal pain (38.6%). Grade 3 diarrhea and fatigue occurred in 19.7% and 12.9% of patients, respectively. Serious AEs occurred in 24.2% of patients and AEs led to treatment discontinuation in 7.6% of patients.
Warnings and precautions
Abemaciclib is marketed as Verzenio by Eli Lilly and Company. Warnings and precautions relating to diarrhea, neutropenia, hepatotoxicity, venous thromboembolism (VTE), and embryofetal toxicity are detailed in the prescribing information. In the event of diarrhea, patients should be treated with antidiarrheal therapy and should increase oral fluids and notify their health care provider. Treatment should be interrupted for grade 3 or 4 diarrhea and then resumed at a lower dose upon return to grade 1.
To guard against neutropenia, complete blood counts should be performed prior to starting therapy, every 2 weeks for the first 2 months, monthly for the subsequent 2 months, and then as clinically indicated. Treatment should be interrupted or delayed or the dose reduced for grade 3 or 4 neutropenia and patients should report episodes of fever.
Liver function tests should be performed before starting abemaciclib, every 2 weeks for the first 2 months, monthly for the next 2 months, and then as
Patients should be monitored for signs and symptoms of VTE and pulmonary embolism, and treated appropriately. Pregnant women should be advised of the potential risk to a fetus, and those of reproductive potential should be counselled on the importance of using effective contraception during treatment and for at least 3 weeks after the last dose.3
1. Sledge Jr GW, Toi M, Neven P, et al. MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2- advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35(25):2875-2884.
2. Dickler MN, Tolaney SM, Rugo HS, et al. MONARCH 1, a phase 2 study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, in patients with refractory HR+/HER2- metastatic breast cancer. Clin Cancer Res. http://clincancerres.aacrjournals.org/content/early/2017/05/20/1078-0432.CCR-17-0754. Published online first on May 22, 2017. Accessed January 19, 2018.
3. Verzenio (abemaciclib) tablets, for oral use. Prescribing information. Eli Lilly and Co. http://uspl.lilly.com/verzenio/verzenio.html#pi. September 2017. Accessed November 20, 2017.
The fall 2017 approval by the US Food and Drug Administration (FDA) of abemaciclib made it the third cyclin-dependent kinase (CDK) inhibitor approved for the treatment of hormone receptor (HR)-positive breast cancer, and the first to receive an approved indication as monotherapy in that setting. Abemaciclib is a small-molecule inhibitor of the CDK4 and CDK6 proteins, which are key gatekeepers of the cell cycle and frequently dysregulated in HR-positive breast cancer. On the basis of the randomized, placebo-controlled, multicenter phase 3 MONARCH-2 trial, it was approved in combination with fulvestrant for the treatment of women with HR-positive, HER2-negative advanced or metastatic breast cancer who had progressed during endocrine therapy.1
A total of 669 women aged 18 years and older, with any menopausal status, an Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 or 1, measurable disease per Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1) or nonmeasurable bone-only disease, were enrolled. Patients had progressed during neoadjuvant or adjuvant endocrine therapy, within 12 months of adjuvant endocrine therapy, or during frontline endocrine treatment for metastatic disease.
Those who had received more than 1 endocrine therapy or any prior chemotherapy for metastatic breast cancer or prior treatment with everolimus or CDK4/6 inhibitors, as well as those with the presence of visceral crisis or evidence or history of central nervous system (CNS) metastases, were excluded from the study.
Patients were randomized 2:1 to receive 150 mg abemaciclib or placebo, both in combination with 500 mg fulvestrant. The initial dose of abemaciclib was 200 mg, but this was amended to 150mg after enrollment of the first 178 patients to alleviate diarrhea-related toxicity concerns. Randomization was stratified according to metastatic site (visceral, bone only, or other) and endocrine therapy resistance (primary or secondary).
Tumors were measured by computed tomography (CT) and magnetic-resonance imaging (MRI) according to RECIST-1.1 within 28 days before random assignment, every 8 weeks for the first year, every 12 weeks thereafter, and then within 2 weeks of clinical progression. Bone scintigraphy was also performed at baseline and then every 6th cycle starting with cycle 7. Hematologic and blood chemistry laboratory tests were performed centrally on days 1 and 15 of the first cycle and day 1 of all remaining cycles.
The primary endpoint was progression-free survival (PFS); median PFS was 16.4 months in the abemaciclib arm, compared with 9.3 months in the placebo arm in the intent-to-treat population (hazard ratio [HR], 0.553;P < .0000001), translating to a 45% reduction in the risk of disease progression or death with the combination. Objective response rate in the 2 groups among patients with measurable disease was 48.1% and 21.3%, respectively, which included a complete response rate of 3.5% in the abemaciclib arm. The median duration of response was not yet reached in the study group, compared with 25.6 months for placebo. Overall survival data were not yet mature.
The agency also approved abemaciclib as monotherapy for women and men with HR-positive, HER2-negative advanced or metastatic breast cancer with disease progression following endocrine therapy and prior chemotherapy in the metastatic setting. That approval was based on data from the single-arm MONARCH-1 trial of 132 patients who received 200 mg abemaciclib twice daily on a continuous schedule.2
Patients had adequate organ function, measurable disease per RECIST-1.1, and an ECOG performance status of 0 or 1. Patients must have progressed on or after previous endocrine therapy and have received prior treatment with at least 2 chemotherapy regimens, at least 1 of them, but no more than 2, having been administered in the metastatic setting. Exclusion criteria included prior receipt of a CDK inhibitor, major surgery within 14 days of the start of the study, and CNS metastases.
Tumor assessments were performed by CT or MRI according to RECIST-1.1 within the 4 weeks prior to the first dose of study drug and then subsequently at every other cycle. Responses were confirmed at least 4 weeks after the initial observation. The overall response rate was 19.7%, made up completely of partial responses. Median duration of response was 8.6 months, median PFS was 6 months and median OS was 17.7 months.
Adverse events
The most common adverse events experienced with the combination of abemaciclib and fulvestrant were neutropenia (23.6%) and diarrhea (13.4%). The rate of grade 4 neutropenia was higher in the combination arm (2.9% vs 0.4%) and there were 3 deaths with the combination that were linked to treatment-related AEs. In the monotherapy trial, abemaciclib treatment most commonly caused diarrhea (90.2%), fatigue (65.2%), nausea (64.4%), decreased appetite (45.5%), and abdominal pain (38.6%). Grade 3 diarrhea and fatigue occurred in 19.7% and 12.9% of patients, respectively. Serious AEs occurred in 24.2% of patients and AEs led to treatment discontinuation in 7.6% of patients.
Warnings and precautions
Abemaciclib is marketed as Verzenio by Eli Lilly and Company. Warnings and precautions relating to diarrhea, neutropenia, hepatotoxicity, venous thromboembolism (VTE), and embryofetal toxicity are detailed in the prescribing information. In the event of diarrhea, patients should be treated with antidiarrheal therapy and should increase oral fluids and notify their health care provider. Treatment should be interrupted for grade 3 or 4 diarrhea and then resumed at a lower dose upon return to grade 1.
To guard against neutropenia, complete blood counts should be performed prior to starting therapy, every 2 weeks for the first 2 months, monthly for the subsequent 2 months, and then as clinically indicated. Treatment should be interrupted or delayed or the dose reduced for grade 3 or 4 neutropenia and patients should report episodes of fever.
Liver function tests should be performed before starting abemaciclib, every 2 weeks for the first 2 months, monthly for the next 2 months, and then as
Patients should be monitored for signs and symptoms of VTE and pulmonary embolism, and treated appropriately. Pregnant women should be advised of the potential risk to a fetus, and those of reproductive potential should be counselled on the importance of using effective contraception during treatment and for at least 3 weeks after the last dose.3
The fall 2017 approval by the US Food and Drug Administration (FDA) of abemaciclib made it the third cyclin-dependent kinase (CDK) inhibitor approved for the treatment of hormone receptor (HR)-positive breast cancer, and the first to receive an approved indication as monotherapy in that setting. Abemaciclib is a small-molecule inhibitor of the CDK4 and CDK6 proteins, which are key gatekeepers of the cell cycle and frequently dysregulated in HR-positive breast cancer. On the basis of the randomized, placebo-controlled, multicenter phase 3 MONARCH-2 trial, it was approved in combination with fulvestrant for the treatment of women with HR-positive, HER2-negative advanced or metastatic breast cancer who had progressed during endocrine therapy.1
A total of 669 women aged 18 years and older, with any menopausal status, an Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 or 1, measurable disease per Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1) or nonmeasurable bone-only disease, were enrolled. Patients had progressed during neoadjuvant or adjuvant endocrine therapy, within 12 months of adjuvant endocrine therapy, or during frontline endocrine treatment for metastatic disease.
Those who had received more than 1 endocrine therapy or any prior chemotherapy for metastatic breast cancer or prior treatment with everolimus or CDK4/6 inhibitors, as well as those with the presence of visceral crisis or evidence or history of central nervous system (CNS) metastases, were excluded from the study.
Patients were randomized 2:1 to receive 150 mg abemaciclib or placebo, both in combination with 500 mg fulvestrant. The initial dose of abemaciclib was 200 mg, but this was amended to 150mg after enrollment of the first 178 patients to alleviate diarrhea-related toxicity concerns. Randomization was stratified according to metastatic site (visceral, bone only, or other) and endocrine therapy resistance (primary or secondary).
Tumors were measured by computed tomography (CT) and magnetic-resonance imaging (MRI) according to RECIST-1.1 within 28 days before random assignment, every 8 weeks for the first year, every 12 weeks thereafter, and then within 2 weeks of clinical progression. Bone scintigraphy was also performed at baseline and then every 6th cycle starting with cycle 7. Hematologic and blood chemistry laboratory tests were performed centrally on days 1 and 15 of the first cycle and day 1 of all remaining cycles.
The primary endpoint was progression-free survival (PFS); median PFS was 16.4 months in the abemaciclib arm, compared with 9.3 months in the placebo arm in the intent-to-treat population (hazard ratio [HR], 0.553;P < .0000001), translating to a 45% reduction in the risk of disease progression or death with the combination. Objective response rate in the 2 groups among patients with measurable disease was 48.1% and 21.3%, respectively, which included a complete response rate of 3.5% in the abemaciclib arm. The median duration of response was not yet reached in the study group, compared with 25.6 months for placebo. Overall survival data were not yet mature.
The agency also approved abemaciclib as monotherapy for women and men with HR-positive, HER2-negative advanced or metastatic breast cancer with disease progression following endocrine therapy and prior chemotherapy in the metastatic setting. That approval was based on data from the single-arm MONARCH-1 trial of 132 patients who received 200 mg abemaciclib twice daily on a continuous schedule.2
Patients had adequate organ function, measurable disease per RECIST-1.1, and an ECOG performance status of 0 or 1. Patients must have progressed on or after previous endocrine therapy and have received prior treatment with at least 2 chemotherapy regimens, at least 1 of them, but no more than 2, having been administered in the metastatic setting. Exclusion criteria included prior receipt of a CDK inhibitor, major surgery within 14 days of the start of the study, and CNS metastases.
Tumor assessments were performed by CT or MRI according to RECIST-1.1 within the 4 weeks prior to the first dose of study drug and then subsequently at every other cycle. Responses were confirmed at least 4 weeks after the initial observation. The overall response rate was 19.7%, made up completely of partial responses. Median duration of response was 8.6 months, median PFS was 6 months and median OS was 17.7 months.
Adverse events
The most common adverse events experienced with the combination of abemaciclib and fulvestrant were neutropenia (23.6%) and diarrhea (13.4%). The rate of grade 4 neutropenia was higher in the combination arm (2.9% vs 0.4%) and there were 3 deaths with the combination that were linked to treatment-related AEs. In the monotherapy trial, abemaciclib treatment most commonly caused diarrhea (90.2%), fatigue (65.2%), nausea (64.4%), decreased appetite (45.5%), and abdominal pain (38.6%). Grade 3 diarrhea and fatigue occurred in 19.7% and 12.9% of patients, respectively. Serious AEs occurred in 24.2% of patients and AEs led to treatment discontinuation in 7.6% of patients.
Warnings and precautions
Abemaciclib is marketed as Verzenio by Eli Lilly and Company. Warnings and precautions relating to diarrhea, neutropenia, hepatotoxicity, venous thromboembolism (VTE), and embryofetal toxicity are detailed in the prescribing information. In the event of diarrhea, patients should be treated with antidiarrheal therapy and should increase oral fluids and notify their health care provider. Treatment should be interrupted for grade 3 or 4 diarrhea and then resumed at a lower dose upon return to grade 1.
To guard against neutropenia, complete blood counts should be performed prior to starting therapy, every 2 weeks for the first 2 months, monthly for the subsequent 2 months, and then as clinically indicated. Treatment should be interrupted or delayed or the dose reduced for grade 3 or 4 neutropenia and patients should report episodes of fever.
Liver function tests should be performed before starting abemaciclib, every 2 weeks for the first 2 months, monthly for the next 2 months, and then as
Patients should be monitored for signs and symptoms of VTE and pulmonary embolism, and treated appropriately. Pregnant women should be advised of the potential risk to a fetus, and those of reproductive potential should be counselled on the importance of using effective contraception during treatment and for at least 3 weeks after the last dose.3
1. Sledge Jr GW, Toi M, Neven P, et al. MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2- advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35(25):2875-2884.
2. Dickler MN, Tolaney SM, Rugo HS, et al. MONARCH 1, a phase 2 study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, in patients with refractory HR+/HER2- metastatic breast cancer. Clin Cancer Res. http://clincancerres.aacrjournals.org/content/early/2017/05/20/1078-0432.CCR-17-0754. Published online first on May 22, 2017. Accessed January 19, 2018.
3. Verzenio (abemaciclib) tablets, for oral use. Prescribing information. Eli Lilly and Co. http://uspl.lilly.com/verzenio/verzenio.html#pi. September 2017. Accessed November 20, 2017.
1. Sledge Jr GW, Toi M, Neven P, et al. MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2- advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35(25):2875-2884.
2. Dickler MN, Tolaney SM, Rugo HS, et al. MONARCH 1, a phase 2 study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, in patients with refractory HR+/HER2- metastatic breast cancer. Clin Cancer Res. http://clincancerres.aacrjournals.org/content/early/2017/05/20/1078-0432.CCR-17-0754. Published online first on May 22, 2017. Accessed January 19, 2018.
3. Verzenio (abemaciclib) tablets, for oral use. Prescribing information. Eli Lilly and Co. http://uspl.lilly.com/verzenio/verzenio.html#pi. September 2017. Accessed November 20, 2017.
Checkpoint inhibitors forge new treatment paradigm for metastatic bladder cancer
Last spring, the US Food and Drug Administration (FDA) granted accelerated approval to 3 different immune checkpoint inhibitors for the treatment of patients with metastatic urothelial carcinoma in the second-line setting, bringing the total number of approved members of this drug class for this indication to 5.
Avelumab and durvalumab, like atezolizumab, are monoclonal antibodies that target the programmed cell death protein ligand-1 (PD-L1) and prevent it from binding to and activating the programmed cell death protein-1 (PD-1) and CD80 receptors, which transmit inhibitory signals into T cells. In this way, it is hypothesized that their use reactivates the anti-tumor immune response conducted by tumor-infiltrating T cells. Both drugs were approved for the treatment of patients with locally advanced or metastatic urothelial carcinoma who are refractory to platinum-based chemotherapy, and the approvals provide additional treatment options for this group of patients who typically have poor prognosis.1,2
Avelumab trial findings
The approval of avelumab was based on the urothelial cancer cohorts of the JAVELIN Solid Tumor trial, a phase 1, open-label, dose-escalation study.3 Patients aged 18 years and older, with an Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 or 1 (range, 0-5; 0, fully active, and 5, dead), life expectancy of at least 3 months, and cytologically or histologically confirmed metastatic or locally advanced solid tumors were eligible.
Patients were excluded from the study if they had a history of or active central nervous system metastases, had other malignancies within the previous 5 years, had undergone organ transplant, had conditions requiring immune suppression, had active HIV or hepatitis B or C infection, or had autoimmune diseases other than type 1 diabetes, vitiligo, psoriasis, or thyroid disease that does not require immunosuppressive treatment.
Patients were also required to have adequate end organ function (white blood cell count, ≥3 x 109 cells/L; absolute neutrophil count, ≥1.5 x 109 cells/L; lymphocyte count, ≥0.5 x 109 cells/L; platelet count, ≥100 x 109 platelets/L; hemoglobin, ≥9 g/dL; total bilirubin concentration, ≤1.5 x upper limit of normal [ULN] range; aspartate- and alanine- aminotransferase (ALT/AST) concentrations, ≤2.5 x ULN); and estimated creatinine clearance, >50 mL/min.
A total of 242 patients were treated with a 10 mg/kg intravenous dose of avelumab every 2 weeks until disease progression or unacceptable toxicity. Before avelumab infusion, all patients received premedication with an antihistamine and acetaminophen.
The primary endpoint was objective response rate (ORR), which was 13.3% among 226 patients followed for at least 13 weeks, including 4% complete response (CR) rate, and 16.1% among 161 patients followed for at least 6 months, including 5.6% CR rate. The median time to response was 2 months and the median response duration had not been reached at the time of data cut-off. PD-L1 expression was evaluable in 84% of patients and there was no discernable variation in the response rates according to the levels of PD-L1 expression on the tumor.
The most common adverse events (AEs) that occurred in at least 20% of patients included fatigue, infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection (UTI). Serious AEs occurred in 41% of patients and most commonly involved UTI, abdominal pain, musculoskeletal pain, creatinine increase/renal failure, dehydration, hematuria, intestinal obstruction, and pyrexia. Deaths owing to AEs occurred in 6% of patients and were related to pneumonitis, respiratory failure, sepsis/urosepsis, cerebrovascular accident, or gastrointestinal AEs.
Durvalumab approval
The agency’s approval of durvalumab rested on the results of an ongoing single-arm phase 1/2 trial (Study 1108).4 Eligibility criteria were the same as for the avelumab study. Patients were ineligible for the trial if they had received any immunotherapy within the previous 4 weeks, any monoclonal antibody within the previous 6 weeks, or had received concurrent chemotherapy, immunotherapy, biologic, or hormonal therapy.
Durvalumab was administered as an intravenous infusion at a dose of 10 mg/kg every 2 weeks, for up to 12 months or until disease progression or unacceptable toxicity. PD-L1 expression was evaluated by immunohistochemistry in tumor tissue obtained before treatment using the Ventana PD-L1 (SP263) assay (Ventana Medical Systems), which was approved by the FDA alongside durvalumab as a companion diagnostic. The first 20 patients were enrolled regardless of their PD-L1 expression, and the subsequent 43 patients were required to have PD-L1 expression of at least 5% of their tumor cells, but that requirement was removed at an interim analysis when objective responses occurred in patients with a PD-L1 expression of lessthan 5%.
In the most up-to-date analysis, published after FDA approval, a total of 191 patients had been treated. The ORR as assessed by blinded independent central review per RECIST-1.1, was 17.8%, including 7 CRs (3.7%). In patients with high PD-L1 expression, the ORR was 27.6%, compared with 5.1% in those with low or no PD-L1 expression. Responses were observed across all subgroups, including patients with a poor prognosis. The ORRs in patients with visceral and liver metastases were 15.3% and 7.3%, respectively. The median time to response was 1.41 months, and the median duration of response had not yet been reached.
The most common AEs experienced by patients treated with durvalumab included fatigue, musculoskeletal pain, constipation, decreased appetite, nausea, peripheral edema, and UTI. Serious treatment-related AEs occurred in 4.7% of patients, and treatment-related AEs leading to death occurred in 2 patients owing to autoimmune hepatitis and pneumonitis.
Toxicities and warnings for both therapies
Avelumab is marketed as Bavencio by EMD Serono, and durvalumab as Imfinzi by AstraZeneca. According to the prescribing information for both drugs, the recommended dose is 10 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks.5,6
Both drugs are associated with serious or potentially life-threatening toxicities for which warnings and precautions are detailed in the prescribing information, predominantly for immune-mediated toxicities such as pneumonitis, hepatitis, colitis, nephritis, and endocrinpathy. Patients should be monitored for signs and symptoms of these toxicities and managed appropriately. Avelumab and durvalumab should both be withheld for grade 2 or higher pneumonitis, hepatitis, colitis, severe or life-threatening adrenal insufficiency, thyroid disorders or hyperglycemia, and moderate or severe nephritis or renal dysfunction.
These drugs should be permanently discontinued in the event of life-threatening or recurrent AEs. Immune-mediated pneumonitis, colitis, and hepatitis and adrenal insufficiency can be managed with corticosteroids; hypothyroidism, with hormone-replacement therapy; and hyperglycemia, with hyperglycemics or insulin.
To manage infusion-related reactions, patients should be premedicated with antihistamines and acetaminophen before the first 4 infusions and closely monitored for symptoms such as pyrexia, chills, flushing, hypotension, and dyspnea. Infusion can be interrupted or slowed for mild to moderate infusion-related reactions, but should be stopped and the drug discontinued for severe or life-threatening reactions.
Durvalumab is also associated with a risk of infection and patients should be monitored for signs and symptoms of infection and treated with anti-infectives. Durvalumab should be withheld for grade 3 infections. Patients being treated with durvalumab or avelumab should also be warned of the potential for embryofetal toxicity and advised to take appropriate precautions.
1. United States Food and Drug Administration. FDA grants accelerated approval to avelumab for urothelial carcinoma. US FDA Web site. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm557162.htm. Last updated May 9, 2017. Accessed September 15, 2017.
2. United States Food and Drug Administration. Durvalumab (Imfinzi). US FDA Web site. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm555930.htm. Last updated May 1, 2017. Accessed September 15, 2017
3. Heery CR, O’Sullivan-Coyne G, Madan RA, Cordes L, et al. Avelumab for metastatic or locally advanced previously treated solid tumors (JAVELIN Solid Tumos): a phase 1a, multicohort, dose-escalation trial. Lancet Oncol. 2017;18(5):587-598.
4. Powles T, O’Donnell PH, Massard C, Arkenau H-T, et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma. Updated results from a phase 1/2 open-label study. JAMA Oncol. 2017;3(8):e172411.
5. Bavencio (avelumab) injection, for intravenous use. Prescribing information. EMD Serono Inc. https://www.bavencio.com/en_US/document/Prescribing-Information.pdf. Revised October 2017. Accessed September 18th, 2017.
6. Imfinzi (durvalumab) injection, for intravenous use. Prescribing information. AstraZeneca Pharmaceuticals. https://www.azpicentral.com/imfinzi/imfinzi.pdf#page=1. Revised May 2017. Accessed September 18, 2017.
Last spring, the US Food and Drug Administration (FDA) granted accelerated approval to 3 different immune checkpoint inhibitors for the treatment of patients with metastatic urothelial carcinoma in the second-line setting, bringing the total number of approved members of this drug class for this indication to 5.
Avelumab and durvalumab, like atezolizumab, are monoclonal antibodies that target the programmed cell death protein ligand-1 (PD-L1) and prevent it from binding to and activating the programmed cell death protein-1 (PD-1) and CD80 receptors, which transmit inhibitory signals into T cells. In this way, it is hypothesized that their use reactivates the anti-tumor immune response conducted by tumor-infiltrating T cells. Both drugs were approved for the treatment of patients with locally advanced or metastatic urothelial carcinoma who are refractory to platinum-based chemotherapy, and the approvals provide additional treatment options for this group of patients who typically have poor prognosis.1,2
Avelumab trial findings
The approval of avelumab was based on the urothelial cancer cohorts of the JAVELIN Solid Tumor trial, a phase 1, open-label, dose-escalation study.3 Patients aged 18 years and older, with an Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 or 1 (range, 0-5; 0, fully active, and 5, dead), life expectancy of at least 3 months, and cytologically or histologically confirmed metastatic or locally advanced solid tumors were eligible.
Patients were excluded from the study if they had a history of or active central nervous system metastases, had other malignancies within the previous 5 years, had undergone organ transplant, had conditions requiring immune suppression, had active HIV or hepatitis B or C infection, or had autoimmune diseases other than type 1 diabetes, vitiligo, psoriasis, or thyroid disease that does not require immunosuppressive treatment.
Patients were also required to have adequate end organ function (white blood cell count, ≥3 x 109 cells/L; absolute neutrophil count, ≥1.5 x 109 cells/L; lymphocyte count, ≥0.5 x 109 cells/L; platelet count, ≥100 x 109 platelets/L; hemoglobin, ≥9 g/dL; total bilirubin concentration, ≤1.5 x upper limit of normal [ULN] range; aspartate- and alanine- aminotransferase (ALT/AST) concentrations, ≤2.5 x ULN); and estimated creatinine clearance, >50 mL/min.
A total of 242 patients were treated with a 10 mg/kg intravenous dose of avelumab every 2 weeks until disease progression or unacceptable toxicity. Before avelumab infusion, all patients received premedication with an antihistamine and acetaminophen.
The primary endpoint was objective response rate (ORR), which was 13.3% among 226 patients followed for at least 13 weeks, including 4% complete response (CR) rate, and 16.1% among 161 patients followed for at least 6 months, including 5.6% CR rate. The median time to response was 2 months and the median response duration had not been reached at the time of data cut-off. PD-L1 expression was evaluable in 84% of patients and there was no discernable variation in the response rates according to the levels of PD-L1 expression on the tumor.
The most common adverse events (AEs) that occurred in at least 20% of patients included fatigue, infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection (UTI). Serious AEs occurred in 41% of patients and most commonly involved UTI, abdominal pain, musculoskeletal pain, creatinine increase/renal failure, dehydration, hematuria, intestinal obstruction, and pyrexia. Deaths owing to AEs occurred in 6% of patients and were related to pneumonitis, respiratory failure, sepsis/urosepsis, cerebrovascular accident, or gastrointestinal AEs.
Durvalumab approval
The agency’s approval of durvalumab rested on the results of an ongoing single-arm phase 1/2 trial (Study 1108).4 Eligibility criteria were the same as for the avelumab study. Patients were ineligible for the trial if they had received any immunotherapy within the previous 4 weeks, any monoclonal antibody within the previous 6 weeks, or had received concurrent chemotherapy, immunotherapy, biologic, or hormonal therapy.
Durvalumab was administered as an intravenous infusion at a dose of 10 mg/kg every 2 weeks, for up to 12 months or until disease progression or unacceptable toxicity. PD-L1 expression was evaluated by immunohistochemistry in tumor tissue obtained before treatment using the Ventana PD-L1 (SP263) assay (Ventana Medical Systems), which was approved by the FDA alongside durvalumab as a companion diagnostic. The first 20 patients were enrolled regardless of their PD-L1 expression, and the subsequent 43 patients were required to have PD-L1 expression of at least 5% of their tumor cells, but that requirement was removed at an interim analysis when objective responses occurred in patients with a PD-L1 expression of lessthan 5%.
In the most up-to-date analysis, published after FDA approval, a total of 191 patients had been treated. The ORR as assessed by blinded independent central review per RECIST-1.1, was 17.8%, including 7 CRs (3.7%). In patients with high PD-L1 expression, the ORR was 27.6%, compared with 5.1% in those with low or no PD-L1 expression. Responses were observed across all subgroups, including patients with a poor prognosis. The ORRs in patients with visceral and liver metastases were 15.3% and 7.3%, respectively. The median time to response was 1.41 months, and the median duration of response had not yet been reached.
The most common AEs experienced by patients treated with durvalumab included fatigue, musculoskeletal pain, constipation, decreased appetite, nausea, peripheral edema, and UTI. Serious treatment-related AEs occurred in 4.7% of patients, and treatment-related AEs leading to death occurred in 2 patients owing to autoimmune hepatitis and pneumonitis.
Toxicities and warnings for both therapies
Avelumab is marketed as Bavencio by EMD Serono, and durvalumab as Imfinzi by AstraZeneca. According to the prescribing information for both drugs, the recommended dose is 10 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks.5,6
Both drugs are associated with serious or potentially life-threatening toxicities for which warnings and precautions are detailed in the prescribing information, predominantly for immune-mediated toxicities such as pneumonitis, hepatitis, colitis, nephritis, and endocrinpathy. Patients should be monitored for signs and symptoms of these toxicities and managed appropriately. Avelumab and durvalumab should both be withheld for grade 2 or higher pneumonitis, hepatitis, colitis, severe or life-threatening adrenal insufficiency, thyroid disorders or hyperglycemia, and moderate or severe nephritis or renal dysfunction.
These drugs should be permanently discontinued in the event of life-threatening or recurrent AEs. Immune-mediated pneumonitis, colitis, and hepatitis and adrenal insufficiency can be managed with corticosteroids; hypothyroidism, with hormone-replacement therapy; and hyperglycemia, with hyperglycemics or insulin.
To manage infusion-related reactions, patients should be premedicated with antihistamines and acetaminophen before the first 4 infusions and closely monitored for symptoms such as pyrexia, chills, flushing, hypotension, and dyspnea. Infusion can be interrupted or slowed for mild to moderate infusion-related reactions, but should be stopped and the drug discontinued for severe or life-threatening reactions.
Durvalumab is also associated with a risk of infection and patients should be monitored for signs and symptoms of infection and treated with anti-infectives. Durvalumab should be withheld for grade 3 infections. Patients being treated with durvalumab or avelumab should also be warned of the potential for embryofetal toxicity and advised to take appropriate precautions.
Last spring, the US Food and Drug Administration (FDA) granted accelerated approval to 3 different immune checkpoint inhibitors for the treatment of patients with metastatic urothelial carcinoma in the second-line setting, bringing the total number of approved members of this drug class for this indication to 5.
Avelumab and durvalumab, like atezolizumab, are monoclonal antibodies that target the programmed cell death protein ligand-1 (PD-L1) and prevent it from binding to and activating the programmed cell death protein-1 (PD-1) and CD80 receptors, which transmit inhibitory signals into T cells. In this way, it is hypothesized that their use reactivates the anti-tumor immune response conducted by tumor-infiltrating T cells. Both drugs were approved for the treatment of patients with locally advanced or metastatic urothelial carcinoma who are refractory to platinum-based chemotherapy, and the approvals provide additional treatment options for this group of patients who typically have poor prognosis.1,2
Avelumab trial findings
The approval of avelumab was based on the urothelial cancer cohorts of the JAVELIN Solid Tumor trial, a phase 1, open-label, dose-escalation study.3 Patients aged 18 years and older, with an Eastern Cooperative Oncology Group (ECOG) Performance Status of 0 or 1 (range, 0-5; 0, fully active, and 5, dead), life expectancy of at least 3 months, and cytologically or histologically confirmed metastatic or locally advanced solid tumors were eligible.
Patients were excluded from the study if they had a history of or active central nervous system metastases, had other malignancies within the previous 5 years, had undergone organ transplant, had conditions requiring immune suppression, had active HIV or hepatitis B or C infection, or had autoimmune diseases other than type 1 diabetes, vitiligo, psoriasis, or thyroid disease that does not require immunosuppressive treatment.
Patients were also required to have adequate end organ function (white blood cell count, ≥3 x 109 cells/L; absolute neutrophil count, ≥1.5 x 109 cells/L; lymphocyte count, ≥0.5 x 109 cells/L; platelet count, ≥100 x 109 platelets/L; hemoglobin, ≥9 g/dL; total bilirubin concentration, ≤1.5 x upper limit of normal [ULN] range; aspartate- and alanine- aminotransferase (ALT/AST) concentrations, ≤2.5 x ULN); and estimated creatinine clearance, >50 mL/min.
A total of 242 patients were treated with a 10 mg/kg intravenous dose of avelumab every 2 weeks until disease progression or unacceptable toxicity. Before avelumab infusion, all patients received premedication with an antihistamine and acetaminophen.
The primary endpoint was objective response rate (ORR), which was 13.3% among 226 patients followed for at least 13 weeks, including 4% complete response (CR) rate, and 16.1% among 161 patients followed for at least 6 months, including 5.6% CR rate. The median time to response was 2 months and the median response duration had not been reached at the time of data cut-off. PD-L1 expression was evaluable in 84% of patients and there was no discernable variation in the response rates according to the levels of PD-L1 expression on the tumor.
The most common adverse events (AEs) that occurred in at least 20% of patients included fatigue, infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection (UTI). Serious AEs occurred in 41% of patients and most commonly involved UTI, abdominal pain, musculoskeletal pain, creatinine increase/renal failure, dehydration, hematuria, intestinal obstruction, and pyrexia. Deaths owing to AEs occurred in 6% of patients and were related to pneumonitis, respiratory failure, sepsis/urosepsis, cerebrovascular accident, or gastrointestinal AEs.
Durvalumab approval
The agency’s approval of durvalumab rested on the results of an ongoing single-arm phase 1/2 trial (Study 1108).4 Eligibility criteria were the same as for the avelumab study. Patients were ineligible for the trial if they had received any immunotherapy within the previous 4 weeks, any monoclonal antibody within the previous 6 weeks, or had received concurrent chemotherapy, immunotherapy, biologic, or hormonal therapy.
Durvalumab was administered as an intravenous infusion at a dose of 10 mg/kg every 2 weeks, for up to 12 months or until disease progression or unacceptable toxicity. PD-L1 expression was evaluated by immunohistochemistry in tumor tissue obtained before treatment using the Ventana PD-L1 (SP263) assay (Ventana Medical Systems), which was approved by the FDA alongside durvalumab as a companion diagnostic. The first 20 patients were enrolled regardless of their PD-L1 expression, and the subsequent 43 patients were required to have PD-L1 expression of at least 5% of their tumor cells, but that requirement was removed at an interim analysis when objective responses occurred in patients with a PD-L1 expression of lessthan 5%.
In the most up-to-date analysis, published after FDA approval, a total of 191 patients had been treated. The ORR as assessed by blinded independent central review per RECIST-1.1, was 17.8%, including 7 CRs (3.7%). In patients with high PD-L1 expression, the ORR was 27.6%, compared with 5.1% in those with low or no PD-L1 expression. Responses were observed across all subgroups, including patients with a poor prognosis. The ORRs in patients with visceral and liver metastases were 15.3% and 7.3%, respectively. The median time to response was 1.41 months, and the median duration of response had not yet been reached.
The most common AEs experienced by patients treated with durvalumab included fatigue, musculoskeletal pain, constipation, decreased appetite, nausea, peripheral edema, and UTI. Serious treatment-related AEs occurred in 4.7% of patients, and treatment-related AEs leading to death occurred in 2 patients owing to autoimmune hepatitis and pneumonitis.
Toxicities and warnings for both therapies
Avelumab is marketed as Bavencio by EMD Serono, and durvalumab as Imfinzi by AstraZeneca. According to the prescribing information for both drugs, the recommended dose is 10 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks.5,6
Both drugs are associated with serious or potentially life-threatening toxicities for which warnings and precautions are detailed in the prescribing information, predominantly for immune-mediated toxicities such as pneumonitis, hepatitis, colitis, nephritis, and endocrinpathy. Patients should be monitored for signs and symptoms of these toxicities and managed appropriately. Avelumab and durvalumab should both be withheld for grade 2 or higher pneumonitis, hepatitis, colitis, severe or life-threatening adrenal insufficiency, thyroid disorders or hyperglycemia, and moderate or severe nephritis or renal dysfunction.
These drugs should be permanently discontinued in the event of life-threatening or recurrent AEs. Immune-mediated pneumonitis, colitis, and hepatitis and adrenal insufficiency can be managed with corticosteroids; hypothyroidism, with hormone-replacement therapy; and hyperglycemia, with hyperglycemics or insulin.
To manage infusion-related reactions, patients should be premedicated with antihistamines and acetaminophen before the first 4 infusions and closely monitored for symptoms such as pyrexia, chills, flushing, hypotension, and dyspnea. Infusion can be interrupted or slowed for mild to moderate infusion-related reactions, but should be stopped and the drug discontinued for severe or life-threatening reactions.
Durvalumab is also associated with a risk of infection and patients should be monitored for signs and symptoms of infection and treated with anti-infectives. Durvalumab should be withheld for grade 3 infections. Patients being treated with durvalumab or avelumab should also be warned of the potential for embryofetal toxicity and advised to take appropriate precautions.
1. United States Food and Drug Administration. FDA grants accelerated approval to avelumab for urothelial carcinoma. US FDA Web site. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm557162.htm. Last updated May 9, 2017. Accessed September 15, 2017.
2. United States Food and Drug Administration. Durvalumab (Imfinzi). US FDA Web site. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm555930.htm. Last updated May 1, 2017. Accessed September 15, 2017
3. Heery CR, O’Sullivan-Coyne G, Madan RA, Cordes L, et al. Avelumab for metastatic or locally advanced previously treated solid tumors (JAVELIN Solid Tumos): a phase 1a, multicohort, dose-escalation trial. Lancet Oncol. 2017;18(5):587-598.
4. Powles T, O’Donnell PH, Massard C, Arkenau H-T, et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma. Updated results from a phase 1/2 open-label study. JAMA Oncol. 2017;3(8):e172411.
5. Bavencio (avelumab) injection, for intravenous use. Prescribing information. EMD Serono Inc. https://www.bavencio.com/en_US/document/Prescribing-Information.pdf. Revised October 2017. Accessed September 18th, 2017.
6. Imfinzi (durvalumab) injection, for intravenous use. Prescribing information. AstraZeneca Pharmaceuticals. https://www.azpicentral.com/imfinzi/imfinzi.pdf#page=1. Revised May 2017. Accessed September 18, 2017.
1. United States Food and Drug Administration. FDA grants accelerated approval to avelumab for urothelial carcinoma. US FDA Web site. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm557162.htm. Last updated May 9, 2017. Accessed September 15, 2017.
2. United States Food and Drug Administration. Durvalumab (Imfinzi). US FDA Web site. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm555930.htm. Last updated May 1, 2017. Accessed September 15, 2017
3. Heery CR, O’Sullivan-Coyne G, Madan RA, Cordes L, et al. Avelumab for metastatic or locally advanced previously treated solid tumors (JAVELIN Solid Tumos): a phase 1a, multicohort, dose-escalation trial. Lancet Oncol. 2017;18(5):587-598.
4. Powles T, O’Donnell PH, Massard C, Arkenau H-T, et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma. Updated results from a phase 1/2 open-label study. JAMA Oncol. 2017;3(8):e172411.
5. Bavencio (avelumab) injection, for intravenous use. Prescribing information. EMD Serono Inc. https://www.bavencio.com/en_US/document/Prescribing-Information.pdf. Revised October 2017. Accessed September 18th, 2017.
6. Imfinzi (durvalumab) injection, for intravenous use. Prescribing information. AstraZeneca Pharmaceuticals. https://www.azpicentral.com/imfinzi/imfinzi.pdf#page=1. Revised May 2017. Accessed September 18, 2017.
Pembrolizumab for dMMR/MSI-H tumors marks first tumor agnostic FDA approval
The United States Food and Drug Administration’s approval earlier this year of pembrolizumab marks the first tumor agnostic indication for a cancer drug.1,2 Accelerated approval was granted for the treatment of adult and pediatric patients with any unresectable or metastatic solid tumor that displays mismatch repair deficiencies (dMMR) or high levels of microsatellite instability (MSI-H) and who have progressed after previous treatment and have no satisfactory alternatives. It is also approved specifically for patients with MSI-H or dMMR colorectal cancer (CRC) that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
Pembrolizumab is a programmed cell death protein-1 (PD-1) receptor inhibitor that blocks the interaction between PD-1 and its ligand, PD-L1, restoring the activity of tumor-infiltrating T cells and boosting the anti-tumor immune response. It is thought to be particularly effective in dMMR/MSI-H tumors because they have a high mutational load and therefore display an abundance of antigens on their surfaces to provoke an immune response.
Approval for the drug was based on the demonstration of durable responses in 149 patients with MSI-H or dMMR cancers across 5 uncontrolled, multicohort, multicenter, single-arm trials. In all, 90 of the patients had CRC, and the remaining 59 patients had 1 of 14 other cancer types that included endometrial, biliary, gastric or gastroesophageal, pancreatic, and breast cancers.
Patients in these trials received pembrolizumab at 1 of 2 different doses, either 200 mg every 3 weeks or 10 mg/kg every 2 weeks, until unacceptable toxicity or disease progression that was symptomatic, rapidly progressive, required urgent intervention, or coincided with a decline in performance status. Treatment was administered for a maximum of 2 years. Patients with an active autoimmune disease or a medical condition that required immunosuppression were ineligible for treatment in all 5 studies.
The median age of enrolled patients was 55 years; 56% were men; 77% white, 19% Asian, 2% black; 98% had metastatic or unresectable disease; and all had an Eastern Cooperative Oncology Group Performance Status of 0 or 1 (range, 0-5, where 0 denotes full activity and 1, restricted in physically strenuous activity but ambulatory). MSI-H and MMR status were identified prospectively using polymerase chain reaction and immunohistochemical analyses, respectively.
The primary endpoint was objective response rate (ORR), according to Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1), as assessed by blinded independent central radiologist review, and response duration. The ORR across all five studies
The safety profile was consistent with previously reported safety data for pembrolizumab. The most common adverse events included fatigue, pruritus, diarrhea, decreased appetite, rash, pyrexia, cough, dyspnea, musculoskeletal pain, constipation, and nausea.
The prescribing information includes a “limitation of use” that states that pembroliumab’s safety and efficacy haven’t been established in pediatric patients with MSI-H cancers of the central nervous system.3 It also details warnings and precautions about immune-mediated toxicities, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and renal dysfunction, among others.
Patients should be monitored for signs and symptoms of these toxicities and treated appropriately. Treatment should be withheld and corticosteroids should be administered for grade 2 or higher pneumonitis, colitis, hepatitis, and nephritis; and corticosteroids and hormone replacement as clinically indicated for endocrinopathies. It should also be withheld for aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels >3-5 times the upper limit of normal (ULN) or total bilirubin levels >1.5-3 times ULN.
Pembrolizumab should be permanently discontinued upon grade 3, 4, or recurrent grade 2 pneumonitis, colitis, nephritis/renal dysfunction, and endocrinopathies or for AST or ALT levels >5 times ULN or total bilirubin levels >3 times ULN. For patients with liver metastases who begin treatment with grade 2 AST or ALT, treatment should be permanently discontinued following increases of more than 50%, relative to baseline, that last for at least 1 week.
Health care providers should also bear in mind that pembrolizumab can, more rarely, cause other immune-mediated toxicities, such as arthritis and exfoliative rash that may require treatment and, based on its mechanism of action, pembrolizumab can also cause fetal harm. Patients with reproductive potential should be advised of the implications. Pembrolizumab is marketed as Keytruda by Merck & Co Inc.
1. United States Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for tissue/site agnostic indication. US FDA Web site. https://www.fda.gov/drugs/informationondrugs/ approveddrugs/ucm560040.htm. Last updated May 30, 2017. Accessed July 15, 2017.
2. Merck. News Release. FDA Approves Merck’s KEYTRUDA (pembrolizumab) for Adult and Pediatric Patients with Unresectable or Metastatic, Microsatellite Instability-High (MSI-H) or Mismatch Repair De[1]cient (dMMR) Solid Tumors. http://www.mrknewsroom. com/news-release/prescription-medicine-news/fda-approvesmercks- keytruda-pembrolizumab-adult-and-pediatr. Last updated May 23, 2017. Accessed July 17, 2017.
3. Keytruda (pembrolizumab) for injection, for intravenous use. Prescribing information. Merck & Co Inc. https://www.merck.com/ product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf. Posted May 2017. Accessed July 15, 2017.
The United States Food and Drug Administration’s approval earlier this year of pembrolizumab marks the first tumor agnostic indication for a cancer drug.1,2 Accelerated approval was granted for the treatment of adult and pediatric patients with any unresectable or metastatic solid tumor that displays mismatch repair deficiencies (dMMR) or high levels of microsatellite instability (MSI-H) and who have progressed after previous treatment and have no satisfactory alternatives. It is also approved specifically for patients with MSI-H or dMMR colorectal cancer (CRC) that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
Pembrolizumab is a programmed cell death protein-1 (PD-1) receptor inhibitor that blocks the interaction between PD-1 and its ligand, PD-L1, restoring the activity of tumor-infiltrating T cells and boosting the anti-tumor immune response. It is thought to be particularly effective in dMMR/MSI-H tumors because they have a high mutational load and therefore display an abundance of antigens on their surfaces to provoke an immune response.
Approval for the drug was based on the demonstration of durable responses in 149 patients with MSI-H or dMMR cancers across 5 uncontrolled, multicohort, multicenter, single-arm trials. In all, 90 of the patients had CRC, and the remaining 59 patients had 1 of 14 other cancer types that included endometrial, biliary, gastric or gastroesophageal, pancreatic, and breast cancers.
Patients in these trials received pembrolizumab at 1 of 2 different doses, either 200 mg every 3 weeks or 10 mg/kg every 2 weeks, until unacceptable toxicity or disease progression that was symptomatic, rapidly progressive, required urgent intervention, or coincided with a decline in performance status. Treatment was administered for a maximum of 2 years. Patients with an active autoimmune disease or a medical condition that required immunosuppression were ineligible for treatment in all 5 studies.
The median age of enrolled patients was 55 years; 56% were men; 77% white, 19% Asian, 2% black; 98% had metastatic or unresectable disease; and all had an Eastern Cooperative Oncology Group Performance Status of 0 or 1 (range, 0-5, where 0 denotes full activity and 1, restricted in physically strenuous activity but ambulatory). MSI-H and MMR status were identified prospectively using polymerase chain reaction and immunohistochemical analyses, respectively.
The primary endpoint was objective response rate (ORR), according to Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1), as assessed by blinded independent central radiologist review, and response duration. The ORR across all five studies
The safety profile was consistent with previously reported safety data for pembrolizumab. The most common adverse events included fatigue, pruritus, diarrhea, decreased appetite, rash, pyrexia, cough, dyspnea, musculoskeletal pain, constipation, and nausea.
The prescribing information includes a “limitation of use” that states that pembroliumab’s safety and efficacy haven’t been established in pediatric patients with MSI-H cancers of the central nervous system.3 It also details warnings and precautions about immune-mediated toxicities, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and renal dysfunction, among others.
Patients should be monitored for signs and symptoms of these toxicities and treated appropriately. Treatment should be withheld and corticosteroids should be administered for grade 2 or higher pneumonitis, colitis, hepatitis, and nephritis; and corticosteroids and hormone replacement as clinically indicated for endocrinopathies. It should also be withheld for aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels >3-5 times the upper limit of normal (ULN) or total bilirubin levels >1.5-3 times ULN.
Pembrolizumab should be permanently discontinued upon grade 3, 4, or recurrent grade 2 pneumonitis, colitis, nephritis/renal dysfunction, and endocrinopathies or for AST or ALT levels >5 times ULN or total bilirubin levels >3 times ULN. For patients with liver metastases who begin treatment with grade 2 AST or ALT, treatment should be permanently discontinued following increases of more than 50%, relative to baseline, that last for at least 1 week.
Health care providers should also bear in mind that pembrolizumab can, more rarely, cause other immune-mediated toxicities, such as arthritis and exfoliative rash that may require treatment and, based on its mechanism of action, pembrolizumab can also cause fetal harm. Patients with reproductive potential should be advised of the implications. Pembrolizumab is marketed as Keytruda by Merck & Co Inc.
The United States Food and Drug Administration’s approval earlier this year of pembrolizumab marks the first tumor agnostic indication for a cancer drug.1,2 Accelerated approval was granted for the treatment of adult and pediatric patients with any unresectable or metastatic solid tumor that displays mismatch repair deficiencies (dMMR) or high levels of microsatellite instability (MSI-H) and who have progressed after previous treatment and have no satisfactory alternatives. It is also approved specifically for patients with MSI-H or dMMR colorectal cancer (CRC) that has progressed after treatment with a fluoropyrimidine, oxaliplatin, and irinotecan.
Pembrolizumab is a programmed cell death protein-1 (PD-1) receptor inhibitor that blocks the interaction between PD-1 and its ligand, PD-L1, restoring the activity of tumor-infiltrating T cells and boosting the anti-tumor immune response. It is thought to be particularly effective in dMMR/MSI-H tumors because they have a high mutational load and therefore display an abundance of antigens on their surfaces to provoke an immune response.
Approval for the drug was based on the demonstration of durable responses in 149 patients with MSI-H or dMMR cancers across 5 uncontrolled, multicohort, multicenter, single-arm trials. In all, 90 of the patients had CRC, and the remaining 59 patients had 1 of 14 other cancer types that included endometrial, biliary, gastric or gastroesophageal, pancreatic, and breast cancers.
Patients in these trials received pembrolizumab at 1 of 2 different doses, either 200 mg every 3 weeks or 10 mg/kg every 2 weeks, until unacceptable toxicity or disease progression that was symptomatic, rapidly progressive, required urgent intervention, or coincided with a decline in performance status. Treatment was administered for a maximum of 2 years. Patients with an active autoimmune disease or a medical condition that required immunosuppression were ineligible for treatment in all 5 studies.
The median age of enrolled patients was 55 years; 56% were men; 77% white, 19% Asian, 2% black; 98% had metastatic or unresectable disease; and all had an Eastern Cooperative Oncology Group Performance Status of 0 or 1 (range, 0-5, where 0 denotes full activity and 1, restricted in physically strenuous activity but ambulatory). MSI-H and MMR status were identified prospectively using polymerase chain reaction and immunohistochemical analyses, respectively.
The primary endpoint was objective response rate (ORR), according to Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1), as assessed by blinded independent central radiologist review, and response duration. The ORR across all five studies
The safety profile was consistent with previously reported safety data for pembrolizumab. The most common adverse events included fatigue, pruritus, diarrhea, decreased appetite, rash, pyrexia, cough, dyspnea, musculoskeletal pain, constipation, and nausea.
The prescribing information includes a “limitation of use” that states that pembroliumab’s safety and efficacy haven’t been established in pediatric patients with MSI-H cancers of the central nervous system.3 It also details warnings and precautions about immune-mediated toxicities, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and renal dysfunction, among others.
Patients should be monitored for signs and symptoms of these toxicities and treated appropriately. Treatment should be withheld and corticosteroids should be administered for grade 2 or higher pneumonitis, colitis, hepatitis, and nephritis; and corticosteroids and hormone replacement as clinically indicated for endocrinopathies. It should also be withheld for aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels >3-5 times the upper limit of normal (ULN) or total bilirubin levels >1.5-3 times ULN.
Pembrolizumab should be permanently discontinued upon grade 3, 4, or recurrent grade 2 pneumonitis, colitis, nephritis/renal dysfunction, and endocrinopathies or for AST or ALT levels >5 times ULN or total bilirubin levels >3 times ULN. For patients with liver metastases who begin treatment with grade 2 AST or ALT, treatment should be permanently discontinued following increases of more than 50%, relative to baseline, that last for at least 1 week.
Health care providers should also bear in mind that pembrolizumab can, more rarely, cause other immune-mediated toxicities, such as arthritis and exfoliative rash that may require treatment and, based on its mechanism of action, pembrolizumab can also cause fetal harm. Patients with reproductive potential should be advised of the implications. Pembrolizumab is marketed as Keytruda by Merck & Co Inc.
1. United States Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for tissue/site agnostic indication. US FDA Web site. https://www.fda.gov/drugs/informationondrugs/ approveddrugs/ucm560040.htm. Last updated May 30, 2017. Accessed July 15, 2017.
2. Merck. News Release. FDA Approves Merck’s KEYTRUDA (pembrolizumab) for Adult and Pediatric Patients with Unresectable or Metastatic, Microsatellite Instability-High (MSI-H) or Mismatch Repair De[1]cient (dMMR) Solid Tumors. http://www.mrknewsroom. com/news-release/prescription-medicine-news/fda-approvesmercks- keytruda-pembrolizumab-adult-and-pediatr. Last updated May 23, 2017. Accessed July 17, 2017.
3. Keytruda (pembrolizumab) for injection, for intravenous use. Prescribing information. Merck & Co Inc. https://www.merck.com/ product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf. Posted May 2017. Accessed July 15, 2017.
1. United States Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for tissue/site agnostic indication. US FDA Web site. https://www.fda.gov/drugs/informationondrugs/ approveddrugs/ucm560040.htm. Last updated May 30, 2017. Accessed July 15, 2017.
2. Merck. News Release. FDA Approves Merck’s KEYTRUDA (pembrolizumab) for Adult and Pediatric Patients with Unresectable or Metastatic, Microsatellite Instability-High (MSI-H) or Mismatch Repair De[1]cient (dMMR) Solid Tumors. http://www.mrknewsroom. com/news-release/prescription-medicine-news/fda-approvesmercks- keytruda-pembrolizumab-adult-and-pediatr. Last updated May 23, 2017. Accessed July 17, 2017.
3. Keytruda (pembrolizumab) for injection, for intravenous use. Prescribing information. Merck & Co Inc. https://www.merck.com/ product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf. Posted May 2017. Accessed July 15, 2017.
Brigatinib approval yields additional treatment options for crizotinib-resistant, ALK-positive NSCLC patients
The accelerated approval by the United States Food and Drug Administration (FDA) of the anaplastic lymphoma kinase (ALK) inhibitor brigatinib, marked the fourth approved drug in this class.1 The most recent approval expands the available treatment options for patients with metastatic ALK-positive non–small-cell lung cancer (NSCLC) whose disease is no longer responding to the first-line ALK inhibitor crizotinib. The FDA based its decision on the results of the phase 2 ALTA trial, in which a significant proportion of patients experienced tumor shrinkage.2
The pivotal trial was a noncomparative, 2-arm, open-label, multicenter study that was carried out during June 2014-September 2015 at 71 centers across 18 countries. Eligible patients were 18 years or older, with locally advanced or metastatic ALK-positive NSCLC, disease progression while taking crizotinib, at least 1 measurable lesion, adequate organ and hematologic function, and Eastern Cooperative Oncology Group (ECOG) performance status of ≤2 (range, 0-5, where 0 means the patient is fully active, and 2, ambulatory and capable of all self-care but not able to carry out any work activities).
Patients were excluded from the trial if they had received previous ALK inhibitor therapy, other than crizotinib, or had received crizotinib within 3 days of the first dose of brigatinib, or they had received chemotherapy, radiation therapy, or investigational drugs within 14 days or monoclonal antibody therapy within 30 days of the first dose of the study drug. Anyone with a history or the presence of pulmonary interstitial disease or drug-related pneumonitis or symptomatic central nervous system (CNS) metastases that were neurologically unstable or required an increasing dose of corticosteroids was also ineligible.
A total of 222 patients were randomized to receive one of two brigatinib doses, either 90 mg daily or 180 mg daily after a 7-day lead-in at 90 mg (the latter to help mitigate pulmonary adverse events observed in previous studies). Randomization was stratified according to baseline brain metastases (present or absent) and best investigator-assessed response to crizotinib (complete response [CR] or partial response [PR] vs other or unknown)
Chest and abdomen imaging by computed-tomography (CT) or magnetic resonance imaging (MRI) with contrast were performed to assess disease at screening and every 8 weeks through cycle 15, and then every 12 weeks until disease progression. Contrast-enhanced brain MRI was carried out at screening and repeated after baseline for the 68% of patients who had CNS metastases at the time of enrollment.
The primary endpoint was confirmed investigator-assessed objective response rate (ORR) per Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1), and secondary endpoints included CNS response, duration of response (DoR), progression-free and overall survival (PFS and OS, respectively). ORRs for the 90-mg and 180-mg doses were 48% and 53%, respectively. Responses occurred quickly and were durable in both arms; after a median follow-up of 8 months, median DoR was 13.8 months for both doses. Among the patients with brain metastases, the intracranial response rates for the two doses were 42% and 67%, respectively, notable because of the poor ability of crizotinib to penetrate the blood-brain barrier.
Other secondary outcomes also favored the 180-mg dose. Investigator-assessed PFS for the 90-mg and 180-mg doses were 9.2 months and 12.9 months, respectively, and estimated 1-year OS was 71% and 80%, respectively, the latter representing a nonstatistically significant 43% reduction in the risk of death with the 180 mg dose. There were 4 confirmed CRs in the 180-mg arm and 1 in the 90-mg arm.
The safety of brigatinib was evaluated in 219 patients who received at least 1 dose of brigatinib. Treatment was discontinued in 8% of patients in the 180-mg arm and 3% in the 90-mg arm because of adverse events (AEs). The most common AEs were nausea, diarrhea, fatigue, cough, and headache, and visual disturbances also occurred. The most common serious AEs were pneumonia and interstitial lung disease/pneumonitis.
The prescribing information details warnings and precautions about these and other potential toxicities, including hypertension, bradycardia, creatine phosphokinase (CPK) and pancreatic enzyme elevation, and hyperglycemia.3 Patients should be monitored for new or worsening respiratory symptoms, especially during the first week of initiating brigatinib treatment; blood pressure should be controlled before treatment initiation and monitored after 2 weeks and at least monthly thereafter; heart rate and blood pressure should be monitored frequently; patients should be advised to report any visual symptoms, or any unexplained muscle pain, tenderness or weakness; CPK, lipase, and amylase levels should be monitored during treatment, and fasting glucose tested before starting treatment and periodically thereafter.
Brigatinib should be withheld in any patient with new or worsening respiratory symptoms, for grade 3 hypertension despite optimal antihypertensive therapy, for symptomatic bradycardia, for patients with new or worsening visual symptoms of grade 2 or above, for grade 3 or 4 CPK or pancreatic enzyme elevation, or if adequate hyperglycemia control cannot be achieved. Treatment should be permanently discontinued for grade 3 or 4 or recurrent interstitial lung disease/pneumonitis, grade 4 or recurrent grade 3 hypertension, life-threatening bradycardia, and grade 4 visual disturbance.
Based on its mechanism of action, brigatinib can cause fetal harm and patients of reproductive potential should be advised of the risks and necessary precautions. Brigatinib is marketed as Alunbrig. It was discovered by Ariad Pharmaceuticals Inc, which was acquired by Takeda in February 2017.
1. United States Food and Drug Administration. Brigatinib. US FDA Web site. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm555841.htm. Last updated April 28, 2017. Accessed July 15, 2017
2. Kim D-W, Tiseo M, Ahn M-J, Reckamp KL, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase-positive non–small-cell lung cancer: a randomized, multicenter phase II trial. J Clin Oncol. 2017;35(22):2490-2498.
3. Alunbrig (brigatinib) tablets, for oral use. Prescribing information. Ariad Pharmaceuticals Inc. https://www.alunbrig.com/assets/pi.pdf. Posted April 2017. Accessed July 15, 2017.
The accelerated approval by the United States Food and Drug Administration (FDA) of the anaplastic lymphoma kinase (ALK) inhibitor brigatinib, marked the fourth approved drug in this class.1 The most recent approval expands the available treatment options for patients with metastatic ALK-positive non–small-cell lung cancer (NSCLC) whose disease is no longer responding to the first-line ALK inhibitor crizotinib. The FDA based its decision on the results of the phase 2 ALTA trial, in which a significant proportion of patients experienced tumor shrinkage.2
The pivotal trial was a noncomparative, 2-arm, open-label, multicenter study that was carried out during June 2014-September 2015 at 71 centers across 18 countries. Eligible patients were 18 years or older, with locally advanced or metastatic ALK-positive NSCLC, disease progression while taking crizotinib, at least 1 measurable lesion, adequate organ and hematologic function, and Eastern Cooperative Oncology Group (ECOG) performance status of ≤2 (range, 0-5, where 0 means the patient is fully active, and 2, ambulatory and capable of all self-care but not able to carry out any work activities).
Patients were excluded from the trial if they had received previous ALK inhibitor therapy, other than crizotinib, or had received crizotinib within 3 days of the first dose of brigatinib, or they had received chemotherapy, radiation therapy, or investigational drugs within 14 days or monoclonal antibody therapy within 30 days of the first dose of the study drug. Anyone with a history or the presence of pulmonary interstitial disease or drug-related pneumonitis or symptomatic central nervous system (CNS) metastases that were neurologically unstable or required an increasing dose of corticosteroids was also ineligible.
A total of 222 patients were randomized to receive one of two brigatinib doses, either 90 mg daily or 180 mg daily after a 7-day lead-in at 90 mg (the latter to help mitigate pulmonary adverse events observed in previous studies). Randomization was stratified according to baseline brain metastases (present or absent) and best investigator-assessed response to crizotinib (complete response [CR] or partial response [PR] vs other or unknown)
Chest and abdomen imaging by computed-tomography (CT) or magnetic resonance imaging (MRI) with contrast were performed to assess disease at screening and every 8 weeks through cycle 15, and then every 12 weeks until disease progression. Contrast-enhanced brain MRI was carried out at screening and repeated after baseline for the 68% of patients who had CNS metastases at the time of enrollment.
The primary endpoint was confirmed investigator-assessed objective response rate (ORR) per Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1), and secondary endpoints included CNS response, duration of response (DoR), progression-free and overall survival (PFS and OS, respectively). ORRs for the 90-mg and 180-mg doses were 48% and 53%, respectively. Responses occurred quickly and were durable in both arms; after a median follow-up of 8 months, median DoR was 13.8 months for both doses. Among the patients with brain metastases, the intracranial response rates for the two doses were 42% and 67%, respectively, notable because of the poor ability of crizotinib to penetrate the blood-brain barrier.
Other secondary outcomes also favored the 180-mg dose. Investigator-assessed PFS for the 90-mg and 180-mg doses were 9.2 months and 12.9 months, respectively, and estimated 1-year OS was 71% and 80%, respectively, the latter representing a nonstatistically significant 43% reduction in the risk of death with the 180 mg dose. There were 4 confirmed CRs in the 180-mg arm and 1 in the 90-mg arm.
The safety of brigatinib was evaluated in 219 patients who received at least 1 dose of brigatinib. Treatment was discontinued in 8% of patients in the 180-mg arm and 3% in the 90-mg arm because of adverse events (AEs). The most common AEs were nausea, diarrhea, fatigue, cough, and headache, and visual disturbances also occurred. The most common serious AEs were pneumonia and interstitial lung disease/pneumonitis.
The prescribing information details warnings and precautions about these and other potential toxicities, including hypertension, bradycardia, creatine phosphokinase (CPK) and pancreatic enzyme elevation, and hyperglycemia.3 Patients should be monitored for new or worsening respiratory symptoms, especially during the first week of initiating brigatinib treatment; blood pressure should be controlled before treatment initiation and monitored after 2 weeks and at least monthly thereafter; heart rate and blood pressure should be monitored frequently; patients should be advised to report any visual symptoms, or any unexplained muscle pain, tenderness or weakness; CPK, lipase, and amylase levels should be monitored during treatment, and fasting glucose tested before starting treatment and periodically thereafter.
Brigatinib should be withheld in any patient with new or worsening respiratory symptoms, for grade 3 hypertension despite optimal antihypertensive therapy, for symptomatic bradycardia, for patients with new or worsening visual symptoms of grade 2 or above, for grade 3 or 4 CPK or pancreatic enzyme elevation, or if adequate hyperglycemia control cannot be achieved. Treatment should be permanently discontinued for grade 3 or 4 or recurrent interstitial lung disease/pneumonitis, grade 4 or recurrent grade 3 hypertension, life-threatening bradycardia, and grade 4 visual disturbance.
Based on its mechanism of action, brigatinib can cause fetal harm and patients of reproductive potential should be advised of the risks and necessary precautions. Brigatinib is marketed as Alunbrig. It was discovered by Ariad Pharmaceuticals Inc, which was acquired by Takeda in February 2017.
The accelerated approval by the United States Food and Drug Administration (FDA) of the anaplastic lymphoma kinase (ALK) inhibitor brigatinib, marked the fourth approved drug in this class.1 The most recent approval expands the available treatment options for patients with metastatic ALK-positive non–small-cell lung cancer (NSCLC) whose disease is no longer responding to the first-line ALK inhibitor crizotinib. The FDA based its decision on the results of the phase 2 ALTA trial, in which a significant proportion of patients experienced tumor shrinkage.2
The pivotal trial was a noncomparative, 2-arm, open-label, multicenter study that was carried out during June 2014-September 2015 at 71 centers across 18 countries. Eligible patients were 18 years or older, with locally advanced or metastatic ALK-positive NSCLC, disease progression while taking crizotinib, at least 1 measurable lesion, adequate organ and hematologic function, and Eastern Cooperative Oncology Group (ECOG) performance status of ≤2 (range, 0-5, where 0 means the patient is fully active, and 2, ambulatory and capable of all self-care but not able to carry out any work activities).
Patients were excluded from the trial if they had received previous ALK inhibitor therapy, other than crizotinib, or had received crizotinib within 3 days of the first dose of brigatinib, or they had received chemotherapy, radiation therapy, or investigational drugs within 14 days or monoclonal antibody therapy within 30 days of the first dose of the study drug. Anyone with a history or the presence of pulmonary interstitial disease or drug-related pneumonitis or symptomatic central nervous system (CNS) metastases that were neurologically unstable or required an increasing dose of corticosteroids was also ineligible.
A total of 222 patients were randomized to receive one of two brigatinib doses, either 90 mg daily or 180 mg daily after a 7-day lead-in at 90 mg (the latter to help mitigate pulmonary adverse events observed in previous studies). Randomization was stratified according to baseline brain metastases (present or absent) and best investigator-assessed response to crizotinib (complete response [CR] or partial response [PR] vs other or unknown)
Chest and abdomen imaging by computed-tomography (CT) or magnetic resonance imaging (MRI) with contrast were performed to assess disease at screening and every 8 weeks through cycle 15, and then every 12 weeks until disease progression. Contrast-enhanced brain MRI was carried out at screening and repeated after baseline for the 68% of patients who had CNS metastases at the time of enrollment.
The primary endpoint was confirmed investigator-assessed objective response rate (ORR) per Response Evaluation Criteria in Solid Tumors (RECIST, version 1.1), and secondary endpoints included CNS response, duration of response (DoR), progression-free and overall survival (PFS and OS, respectively). ORRs for the 90-mg and 180-mg doses were 48% and 53%, respectively. Responses occurred quickly and were durable in both arms; after a median follow-up of 8 months, median DoR was 13.8 months for both doses. Among the patients with brain metastases, the intracranial response rates for the two doses were 42% and 67%, respectively, notable because of the poor ability of crizotinib to penetrate the blood-brain barrier.
Other secondary outcomes also favored the 180-mg dose. Investigator-assessed PFS for the 90-mg and 180-mg doses were 9.2 months and 12.9 months, respectively, and estimated 1-year OS was 71% and 80%, respectively, the latter representing a nonstatistically significant 43% reduction in the risk of death with the 180 mg dose. There were 4 confirmed CRs in the 180-mg arm and 1 in the 90-mg arm.
The safety of brigatinib was evaluated in 219 patients who received at least 1 dose of brigatinib. Treatment was discontinued in 8% of patients in the 180-mg arm and 3% in the 90-mg arm because of adverse events (AEs). The most common AEs were nausea, diarrhea, fatigue, cough, and headache, and visual disturbances also occurred. The most common serious AEs were pneumonia and interstitial lung disease/pneumonitis.
The prescribing information details warnings and precautions about these and other potential toxicities, including hypertension, bradycardia, creatine phosphokinase (CPK) and pancreatic enzyme elevation, and hyperglycemia.3 Patients should be monitored for new or worsening respiratory symptoms, especially during the first week of initiating brigatinib treatment; blood pressure should be controlled before treatment initiation and monitored after 2 weeks and at least monthly thereafter; heart rate and blood pressure should be monitored frequently; patients should be advised to report any visual symptoms, or any unexplained muscle pain, tenderness or weakness; CPK, lipase, and amylase levels should be monitored during treatment, and fasting glucose tested before starting treatment and periodically thereafter.
Brigatinib should be withheld in any patient with new or worsening respiratory symptoms, for grade 3 hypertension despite optimal antihypertensive therapy, for symptomatic bradycardia, for patients with new or worsening visual symptoms of grade 2 or above, for grade 3 or 4 CPK or pancreatic enzyme elevation, or if adequate hyperglycemia control cannot be achieved. Treatment should be permanently discontinued for grade 3 or 4 or recurrent interstitial lung disease/pneumonitis, grade 4 or recurrent grade 3 hypertension, life-threatening bradycardia, and grade 4 visual disturbance.
Based on its mechanism of action, brigatinib can cause fetal harm and patients of reproductive potential should be advised of the risks and necessary precautions. Brigatinib is marketed as Alunbrig. It was discovered by Ariad Pharmaceuticals Inc, which was acquired by Takeda in February 2017.
1. United States Food and Drug Administration. Brigatinib. US FDA Web site. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm555841.htm. Last updated April 28, 2017. Accessed July 15, 2017
2. Kim D-W, Tiseo M, Ahn M-J, Reckamp KL, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase-positive non–small-cell lung cancer: a randomized, multicenter phase II trial. J Clin Oncol. 2017;35(22):2490-2498.
3. Alunbrig (brigatinib) tablets, for oral use. Prescribing information. Ariad Pharmaceuticals Inc. https://www.alunbrig.com/assets/pi.pdf. Posted April 2017. Accessed July 15, 2017.
1. United States Food and Drug Administration. Brigatinib. US FDA Web site. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm555841.htm. Last updated April 28, 2017. Accessed July 15, 2017
2. Kim D-W, Tiseo M, Ahn M-J, Reckamp KL, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase-positive non–small-cell lung cancer: a randomized, multicenter phase II trial. J Clin Oncol. 2017;35(22):2490-2498.
3. Alunbrig (brigatinib) tablets, for oral use. Prescribing information. Ariad Pharmaceuticals Inc. https://www.alunbrig.com/assets/pi.pdf. Posted April 2017. Accessed July 15, 2017.