User login
- Part 1: Making the correct diagnosis
(September 2011) - Part 3: Vestibulodynia
(November 2011)
As we discussed in the first installment of this three-part series in the September issue of OBG Management, the causes of vulvar pain are many, and the diagnosis of this common complaint can be difficult. Once the diagnosis of vulvodynia has been made, however, the challenge shifts to finding an effective treatment. Here, our expert panel discusses the many options available, the data (or lack of it) behind each therapy, and what to do in refractory cases.
In Part 3 of this series, in the November issue, the focus will be vestibulodynia.

The lower vagina and vulva are richly supplied with peripheral nerves and are, therefore, sensitive to pain, particularly the region of the hymeneal ring. Although the pudendal nerve (arrow) courses through the area, it is an uncommon source of vulvar pain.
Management of vulvar pain begins with simple measures
Dr. Lonky: How do you approach treatment of vulvar pain syndromes?
Dr. Haefner: I often advise the patient to begin with simple measures. For example, I recommend that she wear cotton underwear during the day, but no underwear at night. If she perspires with exercise, wicking underwear may be helpful. I also counsel the patient to avoid vulvar irritants, douches, and the application of soap of any kind to the vulva. Cool gel packs are sometimes helpful.
When it comes to intercourse, I recommend adequate lubrication using any of a number of effective products, such as olive oil, vitamin E oil, Replens, Slippery Stuff, Astroglide, KY Liquid, and others.
There is an extensive list of lubricants at http://www.med.umich.edu/sexualhealth/resources/guide.htm
Topical agents might offer relief—but so might placebo
Dr. Lonky: What is the role of topical medications, including anesthetics, for treating vulvar pain syndromes?
Dr. Edwards: I don’t find topical medications to be particularly useful in the treatment of vulvodynia, except for lidocaine 2% jelly, or lidocaine 5% ointment, which tends to burn with application—but I never start a patient on only one medication, so judging the effectiveness of a topical therapy is difficult in that context. Good studies of topical medications in the treatment of vulvar pain syndromes are lacking, other than the recent report on amitriptyline and baclofen.1
Dr. Haefner: For minor degrees of pain, consider lidocaine 5% ointment.
Lidocaine/prilocaine (eutectic mixture of local anesthesia or LMX) may be used but can be irritating.
Doxepin 5% cream can be applied to skin daily, gradually increasing the number of daily applications to as many as four.
Topical amitriptyline 2% with baclofen 2% in a water washable base has also been used for point tenderness (squirt 0.5 cc from a syringe onto the finger and apply it to the affected area three times a day).1
Dr. Gunter: Topical estrogen is prescribed by many providers, but we lack studies supporting its efficacy, except for reversing hypoestrogenic changes in postmenopausal women. Some providers use a high-dose, compounded topical estrogen with lidocaine for vestibulodynia. Certainly, local hypoestrogenic changes should be reversed in postmenopausal women before a diagnosis of vulvodynia or vestibulodynia is given.
As for other topical therapies, they are widely used. Some women report improvement with application of plain petrolatum.2 Response rates of 33% to 46% after use of a topical placebo for vestibulodynia are well described in the literature.3,4
Topical analgesics are used frequently, either sporadically (during pain flares) or regularly (daily application). One method of application for localized vestibulodynia involves liberally coating a cotton ball with lidocaine 5% and then applying it to the vestibule overnight (for at least 8 hours of exposure). In this study, after 7 weeks, 76% of women were able to be sexually active, compared with 36% before the start of treatment. However, a randomized, placebo-controlled trial that included lidocaine 5% cream in one arm identified only a 20% reduction in pain for women who had localized vestibulodynia—although, in this trial, the lidocaine was massaged into the vestibule four times daily.5 In this study, interestingly enough, topical lidocaine was less effective than topical placebo, which produced a 33% response rate.3
Lidocaine gel has also been used, although some women report more local irritation with gel than with ointment.
Dr. Lonky: Do we have any data on topical application of other drugs?
Dr. Gunter: Compounded adjuvant medications have been evaluated. In a retrospective study of topical gabapentin in a Lipoderm base, women who had generalized or localized vulvodynia applied a dose of 2%, 4%, or 6% three times daily. Of these women, 80% experienced a reduction of at least 50% in the pain score. In addition, 67% of patients who had localized vestibular pain were able to resume intercourse.6
A retrospective review of 38 women who used 2% amitriptyline and 2% baclofen in a Lipoderm cream for localized vestibular pain found that 53% experienced an improvement in symptoms of at least 60%, but there was no change in the frequency of sexual intercourse.1
Do tricyclic antidepressants ease chronic pain?
Dr. Lonky: Let’s talk, for a moment, about the use of oral tricyclic antidepressants in the treatment of vulvar pain syndromes. What do we know?
Dr. Haefner: Tricyclic antidepressants are a common treatment for vulvar pain. This group of drugs (including amitriptyline [Elavil], nortriptyline [Pamelor], and desipramine [Norpramin]) has been used to treat many idiopathic chronic pain conditions. Published and presented reports indicate that these drugs elicit about a 60% response rate for various pain conditions. A trial by the National Institutes of Health (NIH) is under way, analyzing the use of antidepressants in women who have vulvar pain.
Although treatment with tricyclic antidepressants has generally been reserved for women who have generalized vulvodynia, recent reports have found these medications to be helpful in the treatment of vestibular pain as well. The mechanism of action is thought to be related to inhibition of the reuptake of transmitters—specifically, norepinephrine and serotonin. However, the mechanism of action may be more closely related to anticholinergic effects. Tricyclics affect sodium channels and the N-methyl-d-aspartate (NMDA) receptor.
If you choose to prescribe one of these medications, consider emphasizing to the patient its effect on the sensation of pain rather than its effect on depression.
Dr. Lonky: Are there any types of patients who should not take a tricyclic?
Dr. Haefner: Yes. A patient should not take a tricyclic if she is pregnant, breastfeeding, or planning to conceive. These medicines also add to the effects of alcohol and other central nervous system depressants.
Dr. Lonky: What dosage is recommended?
Dr. Haefner: The dosage for pain control varies, depending on the age of the patient and the particular agent used. Amitriptyline is often used as a first-line medication. I start the patient on 10 to 25 mg nightly and increase that amount by 10 to 25 mg weekly, not to exceed 150 mg daily. A sample regimen might be 10 mg at bedtime for 1 week. If symptoms persist, increase the dose to 20 mg at bedtime for another week, and so on. Once a dose is established that provides relief, the patient should continue to take that amount nightly. Advise the patient not to discontinue the drug abruptly. Rather, it should be weaned.
In patients who are 60 years or older, I give a starting dose of 5 to 10 mg and increase it by 10 mg weekly.
In all age groups, it is important to advise patients to avoid consuming more than one alcoholic beverage daily while taking this medication. And in reproductive-age women, contraception is critical.
Dr. Edwards: I call these drugs tricyclic medications rather than antidepressants. They are extremely useful in managing the neuropathic component of vulvar pain. Despite a recent, apparently well-conducted study showing a lack of benefit, my 25 years of personal clinical experience with tricyclics convince me that I should wait for follow-up studies before abandoning this therapy.3
The pain literature reports that higher doses than previously reported of tricyclic medications are needed for optimal management of neuropathic pain. Doses from 100 to 150 mg are often required for substantial improvement, and a major design flaw in many studies of the effect of tricyclic medications on vulvodynia is the use of an insufficient dose.
Because of their low cost and their effectiveness, tricyclic medications are my first-line therapy for women who do not suffer severe constipation or dry eyes. The effect on depression is a useful side effect, I find.
Dr. Gunter: Although adjuvant medications, such as antidepressants and anticonvulsants, are considered by more than 80% of practitioners to be effective for vulvodynia, it is important to understand that only one randomized, double-blind, placebo-controlled prospective study has evaluated this approach, and that study found a placebo response rate of 33%.3,7
Randomized studies indicate that low-dose amitriptyline (10–20 mg) and desipramine (150 mg) are ineffective for provoked vestibulodynia.3,8 Cohort and retrospective studies with higher doses of amitriptyline (40 to 60 mg/day) indicate that improvement in pain scores of 50% or more can be achieved for 47% to 59% of women who have localized provoked vestibulodynia and generalized unprovoked vulvodynia.9-11
Tricyclic antidepressants and anticonvulsants should be prescribed with caution for patients 65 years and older because they increase the risk of falls.
I give nortriptyline as a first-line agent to women who have both provoked and unprovoked pain. In general, it has fewer anticholinergic side effects than amitriptyline and is generic—it also is taken once daily. For women who have unprovoked pain, I use gabapentin as a second-line agent.
Dr. Lonky: Are any other antidepressants useful in the treatment of vulvar pain?
Dr. Haefner: I sometimes give duloxetine [Cymbalta], starting with an oral daily dose of 30 mg for 1 week. If symptoms persist, I increase the daily dose to a total of 60 mg. (If the patient is depressed, I have her take 30 mg twice daily; if she isn’t depressed, I have her take the full dose of 60 mg in the morning.) I also occasionally utilize venlafaxine [Effexor XR] for pain control, starting with an oral morning dose of 37.5 mg. This dose can be increased to 75 mg/day.
Dr. Edwards: Literature on venlafaxine for neuropathic pain suggests maximal effects at doses of 150 to 225 mg of the extended release formulation, which is often well tolerated. I start patients on 37.5 mg and increase weekly until I reach the 150-mg threshold.12
Are anticonvulsants effective pain relievers?
Dr. Lonky: How effective are oral anticonvulsants such as gabapentin [Neurontin]?
Dr. Haefner: Gabapentin has been used to treat chronic pain conditions. The drug is available in 100-mg, 300-mg, 400-mg, 600-mg, and 800-mg tablets. It is typically initiated at an oral dose of 300 mg daily for 3 days. The dosage is then increased to 300 mg twice daily for 3 days and, finally, to 300 mg three times daily. If necessary, it can gradually be increased to a total of 3,600 mg daily (usually divided into three doses). No more than 1,200 mg should be administered in a single dose. Side effects include somnolence, mental changes, dizziness, and weight gain.
Dr. Edwards: After tricyclic medications, I find gabapentin to be the most beneficial and easily tolerated agent. I give it to patients who have contraindications to tricyclics and who lack a strong component of depression.
Dr. Gunter: Retrospective reviews have found gabapentin to produce improvement of 80% or more in pain scores for 64% to 82% of women who have generalized unprovoked vulvodynia. And a small open-label, prospective trial of lamotrigine [Lamictal] found that it produced statistically significant improvement for generalized vulvodynia.13-15
Dr. Lonky: What do you know about the use of the anticonvulsants pregabalin [Lyrica] and topiramate [Topamax] to treat vulvar pain syndromes?
Dr. Gunter: Pregabalin was reported to reduce symptoms by 80% for generalized, unprovoked vulvodynia in one case report.16
Dr. Edwards: I find that pregabalin is less well tolerated (and more expensive) than gabapentin, so it is one of the last agents I prescribe. I reported a small, uncontrolled series of patients who were treated with pregabalin. Of those who tolerated the drug, two thirds of the women improved by approximately 62%, as judged by a visual analog scale.
Dr. Haefner: Pregabalin is a relatively new addition to the armamentarium. I give 50 mg orally for 4 days to start. If symptoms persist, I increase the dose to 50 mg twice a day for 4 days. If symptoms still persist, I up the dose again to 50 mg three times daily and gradually increase it to 100 mg three times daily, if necessary. Some reports describe a dose as high as 300 mg twice daily (maximum).
As for topiramate, I have been using it much more frequently for vulvodynia and noticing many fewer side effects than with gabapentin.
you offer them?
A patient who has a short duration of pain often responds to topical medications. In contrast, someone who has experienced pain for years is unlikely to get adequate relief from topical medications alone. These patients often require oral tricyclic antidepressants or anticonvulsants, or both. I often start these medications before deciding whether physical therapy is necessary. If the drugs do not provide adequate relief, then I refer the patient to physical therapy.
In some cases, I begin with physical therapy and add other treatments, if necessary. A patient who has localized vulvodynia who tightens her bulbocavernosus and levator ani muscles upon gentle touch may benefit from starting with physical therapy.
I reserve surgery—vestibulectomy—for the patient who has localized pain that has not responded to numerous treatments.
—Hope K. Haefner, MD
Does capsaicin interrupt the pain circuit?
Dr. Lonky: Capsaicin has been mentioned in the literature as a therapy for vulvar pain. Is it effective? How does it work?
Dr. Haefner: Capsaicin activates A-delta sensory neurons and unmyelinated C fibers. It is a vanillyl amide that evokes the sensation of burning pain. It has been proposed as a means of desensitization, which occurs as an acute reaction mediated by neuropeptides (including substance P).17 Steinberg and colleagues found that topical capsaicin significantly decreased pain with intercourse.17 Patients applied capsaicin 0.025% cream for 20 minutes daily for 12 weeks.
In a study by Murina and colleagues, 33 women were treated with topical capsaicin 0.05%. The capsaicin cream was applied to the vulva twice daily for 30 days, then once daily for 30 days, then twice weekly for 4 months. In this study, however, the response to treatment was only partial.18
Dr. Edwards: I have never had a patient willing to try capsaicin after I describe the therapy to them.
Dr. Gunter: Two studies have evaluated daily applications of capsaicin in concentrations of 0.025% and 0.05%—one of them the study by Murina and colleagues that Dr. Haefner mentioned.2,18 The initial release of substance P causes significant burning on application, so pretreatment with local anesthetic to help the patient tolerate the capsaicin is recommended, which could potentially confound the results. In one study, daily pain scores, as well as pain with intercourse, improved significantly for 59% of participants, but no patient experienced complete resolution of symptoms—and within 2 weeks after capsaicin was discontinued, symptoms returned.2,18 I have had only one patient in 15 years of practice who was willing to try capsaicin and who could get past the initial burning.
Another application for botulinum toxin type A?
Dr. Lonky: Is botulinum toxin type A [Botox] at all effective?
Dr. Haefner: Botulinum toxin type A has been utilized to treat provoked vestibulodynia as well as vaginismus and was beneficial.19-23 It blocks the cholinergic innervation of the target tissue. The therapeutic dose ranges from 20 IU to 300 IU.24
A placebo-controlled trial found that injection of 20 IU of botulinum toxin into the vestibule of women with vestibulodynia did not reduce pain, improve sexual functioning, or impact the quality of life, compared with placebo.25 However, this study utilized a lower dose of botulinum toxin than was used in many of the other studies.
Dr. Edwards: I have only used botulinum toxin type A in a low dose. I injected 6 IU of botulinum toxin A into the periphery of the vestibule at 3, 6, 9, and 12 o’clock in six patients, and half improved modestly. I am not prepared to use electromyography (EMG) localization in my office, but from anecdotal reports, as well as several small series and placebo-controlled trials, I would conclude that some patients improve. Those who have hypertonic pelvic floor muscles are likely to be the best candidates for this treatment.
Because the agent relieves pain only modestly, and because it is not covered by insurance for this application, I refer the patient to a gynecologist in my area who administers the drug under EMG localization.
Dr. Gunter: Given the well-documented effect on muscle spasticity, as well as studies that suggest they are also anti-nociceptive agents, botulinum toxins are certainly an attractive concept for vulvodynia. A small case series and a case report indicated significant improvement with vestibular injections of 20 to 40 U of botulinum toxin. However, a randomized, placebo-controlled, double-blind study indicated no significant improvement for women with localized vestibular pain.25-27
I discuss botulinum toxin A with my patients. I explain that my clinical experience does differ from results published in the literature. I find that many women with vestibulodynia opt to try an injection before proceeding to vestibulectomy.
When combined with pelvic floor physical therapy, botulinum toxins are highly effective at treating muscle spasm and can be very useful for women who have a component to their pain of vaginismus or high-tone pelvic floor dysfunction.
How useful are steroids and nerve blocks?
Dr. Lonky: Is there a role for local injections of glucocorticoids or serial nerve blocks?
Dr. Edwards: The occasional patient with very localized pain (trigger point) responds fairly well in my office to intralesional corticosteroids. I have not used or seen reports describing administration of intralesional corticosteroids into a larger area, although two practitioners have told me informally that it is useful in their hands.
As a dermatologist, I cannot perform blocks. I have referred patients to gyn and pain clinics for this purpose, but neither venue has been willing to administer the blocks.
Dr. Haefner: Patients who present with small, localized areas of pain may benefit from local injections. In small areas—for example, a painful spot 1 cm in diameter—triamcinolone acetonide in combination with bupivacaine may be helpful. It is important to use a small dose of steroid in a small area, however, because tissue erosion or ulceration can occur with too high a dose of steroid in the skin. For large areas, as much as 40 mg of triamcinolone acetonide may be utilized in a single monthly dose. Generally, the dose is repeated monthly, if necessary, as many as three or four times.
For large areas, bupivacaine 0.25% is utilized, and for small areas, bupivacaine 0.5% is injected into the vulva along with the steroid. The steroid should be drawn into the syringe first (because the vial can be used at a later time), followed by bupivacaine, which is a single-dose vial.
Pudendal nerve blocks using bupivacaine have been helpful in some patients—particularly those who have unilateral pain.
Dr. Gunter: Local injections with a variety of agents for localized, provoked vestibulodynia have been described, including steroids, botulinum toxins, and interferon. It is important to interpret these studies with caution, however, as placebo response rates with injection therapy are significant.25
A retrospective review of submucous injections of methylprednisolone and lidocaine found that 68% of women had a complete or marked response, and two case reports describe success with betamethasone.26,28-30 I offer steroid injections to women who have vestibulodynia before proceeding to vestibulectomy; I find that about 50% get at least partial relief. As Dr. Haefner indicated from her own experience, my success seems best with steroid injections in the vestibule when the painful area is smaller.
Using injectable steroids and botulinum toxins, I estimate that I can prevent 33% to 40% of vestibulectomies. Although this may not be better than the placebo response rate and certainly represents biased patient selection (patients are not required to try local injection before vestibulectomy for vestibulodynia), those who are successful are uniformly happy for trying it, and those for whom it did not work are not unhappy that they “gave it a try,” as these women are all motivated to avoid surgery, if possible.
Pudendal nerve blocks with triamcinolone are also described for women who have generalized unprovoked vulvodynia due to suspected pudendal neuralgia. Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—have also been performed with good results for generalized vulvodynia. I have had good success with pudendal nerve blocks for unilateral pain that is suspected to be pudendal in origin and also with ganglion impar blocks for women with generalized vulvodynia, especially postmenopausal women. I perform all of my own nerve blocks (FIGURE).
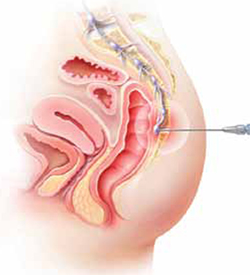
Ganglion impar block
Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—may provide relief from generalized vulvodynia in some women.
Does physical therapy play a role in easing vulvar pain?
Dr. Lonky: What is the role of physical therapy and pelvic floor muscle rehabilitation?
Dr. Gunter: All women who have high-tone pelvic floor dysfunction should be referred to a physical therapist. Many women who lack muscle spasm but experience vulvar pain can still benefit from physical therapy, as gentle stretching and vibration therapy can sometimes be helpful. A physical therapist can also perform biofeedback.
Dr. Edwards: Physical therapy is crucial. It is my first-line therapy overall, with adjunctive oral medication for neuropathic pain. Besides addressing pelvic floor abnormalities, physical therapy can serve as desensitization therapy and psychological support.
Dr. Haefner: Physical therapy has been successful in the treatment of a number of disorders, including migraine and tension headaches, asthma, and anxiety disorders. It is also used in the treatment of vulvar pain. Physical therapists who have experience in vulvar pain may be extremely helpful, particularly if there is concomitant vaginismus—which isn’t uncommon in this population.
For vulvodynia, techniques include internal (vaginal and rectal) and external soft-tissue mobilization and myofascial release; trigger-point pressure; visceral, urogenital, and joint manipulation; electrical stimulation; therapeutic exercises; active pelvic floor retraining; biofeedback; bladder and bowel retraining; and therapeutic ultrasound.
Biofeedback may be used to assist in developing self-regulation strategies for confronting and reducing pain. Patients who have vestibular pain in general have an increased resting tone and a decreased contraction tone. With the aid of an electronic measurement and amplification system or biofeedback machine, an individual can view a display of numbers on a meter, or colored lights, to assess nerve and muscle tension. In this way, she may be able to develop voluntary control over the biological systems involved in pain, discomfort, and disease.
The duration of physical therapy overall and the frequency of visits varies from person to person. Success rates in the range of 60% to 80% have been reported.
How should we respond when medical treatment fails?
Dr. Lonky: What is the proper approach to the patient who has recalcitrant vulvar pain who fails all medical treatments and is not a candidate for vestibulectomy because her pain is outside the vestibule?
Dr. Edwards: The pain clinic. Actually, in a perfect world, the role of the gynecologist or dermatologist would be to give the patient a diagnosis, after which a pain clinic would offer treatment.
All patients should receive counseling. And clinicians who lack expertise should refer the patient to a vulvodynia specialist.
Dr. Haefner: This type of patient may benefit from physical therapy. Bupivacaine steroid injections could also be considered. A sacral nerve stimulator should be considered if the other measures fail to provide adequate relief.
I agree that counseling is extremely helpful in the patient who has vulvodynia. Sexual counseling, with tips on positions for intercourse, lubricants, and control of uncomfortable situations, is of utmost importance.
Dr. Gunter: I offer oral medications and nerve blocks (typically, ganglion impar blocks), and many patients do well.
I also highly recommend advanced programs for mind-body techniques.
Patients who fail all therapies may be candidates for a nerve stimulator, depending on psychiatric comorbidities and response to selective diagnostic nerve blocks.
What’s in the pipeline?
Dr. Lonky: What therapies for vulvar pain are on the horizon?
Dr. Edwards: I believe that cognitive behavioral therapy, sex therapy, and couple counseling will play a larger role in the management of vulvar pain.
Dr. Gunter: Any therapy used in other pain conditions will probably eventually find its way to the management of vulvodynia.
Some investigators believe that Tarlov cysts play a role in vulvar pain and recommend that all women undergo sacral spine and nerve-root magnetic resonance imaging. The problem is that many asymptomatic women have Tarlov cysts, and the surgery to remove them is not at all risk-free. I strongly believe that more research is needed before we can suggest that Tarlov cysts be removed.
Dr. Haefner: Transcutaneous electrical stimulation and biofeedback have been used successfully in the treatment of vulvodynia.31 Some patients benefit from spinal cord stimulators, such as the sacral nerve stimulator, for pain control. Sacral nerve modulation (SNM) works primarily by modulation of the nerve signals to and from the pelvic floor muscles, bladder, and rectum. It applies low-amplitude electrical stimulation to the third sacral nerve via electrodes in a tined lead passing through the S3 foramen, which contains afferent sensory, efferent autonomic motor, and voluntary somatic nerves. Other studies have utilized a different spinal cord level. More studies are needed to demonstrate the full effect of SNM on vulvodynia.
A comprehensive review of the various treatments for vulvodynia can be found in the Journal of Lower Genital Tract Disease.2
Dr. Lonky: Thanks again for your expertise. We’ll focus on provoked vestibulodynia in the final installment of this series on vulvar pain, in the November 2011 issue of OBG Management.
Vulvar pain therapies mentioned in this discussion
| Lifestyle changes Cotton and/or wicking underwear Avoidance of vulvar irritants, douches, soap Use of lubricants during intercourse |
| Physical therapy Internal (vaginal and rectal) and external soft-tissue mobilization and myofascial release Trigger-point pressure Visceral, urogenital, and joint manipulation Electrical stimulation Therapeutic exercises Active pelvic floor retraining Biofeedback Bladder and bowel retraining Therapeutic ultrasound |
| Topical agents Lidocaine 2% jelly Lidocaine 5% ointment Lidocaine/prilocaine Doxepin 5% cream Amitriptyline 2%/baclofen 2% Estrogen Petrolatum Gabapentin |
Oral agents Tricyclic antidepressants
Other antidepressants
Anticonvulsants
|
| Other agents Capsaicin Botulinum toxin type A Corticosteroids Nerve block |
We want to hear from you! Tell us what you think.
1. Nyirjesy P, Lev-Sagie A, Mathew L, Culhane JF. Topical amitriptyline-baclofen cream for the treatment of provoked vestibulodynia. J Lower Genital Tract Dis. 2009;13(4):230-236.
2. Haefner HK, Collins ME, Davis GD, et al. The vulvodynia guideline. J Lower Genital Tract Dis. 2005;9(1):40-51.
3. Foster DC, Kotok MB, Huang L, et al. Oral desipramine and topical lidocaine for vulvodynia: a randomized controlled trial. Obstet Gynecol. 2010;116(3):583-593.
4. Nyirjesy P, Sobel JD, Weitz MV, Leaman DJ, Small MJ, Gelone SP. Cromolyn cream for recalcitrant idiopathic vulvar vestibulitis: results of a placebo-controlled trial. Sex Transm Infect. 2001;77(1):53-57.
5. Zolnoun DA, Hartmann KE, Steege JF. Overnight 5% lidocaine ointment for treatment of vulvar vestibulitis. Obstet Gynecol. 2003;102(1):84-87.
6. Boardman LA, Cooper AS, Blais LR, Raker CA. Topical gabapentin in the treatment of localized and generalized vulvodynia. Obstet Gynecol. 2008;112(3):579-585.
7. Reed BD, Haefner HK, Edwards L. A survey on diagnosis and treatment of vulvodynia researchers and members of the International Society for the Study of Vulvovaginal Disease. J Reprod Med. 2008;53(12):921-929.
8. Brown CS, Wan J, Bachmann G, Rosen R. Self-management amitriptyline, and amitriptyline plus triamcinolone in the management of vulvodynia. J Women Health (Larchmt). 2009;18(2):163-169.
9. Reed BD, Caron AM, Gorenflo DW, Haefner HK. Treatment of vulvodynia with tricyclic antidepressants: efficacy and associated factors. J Low Genit Tract Dis. 2006;10(4):245-251.
10. Munday PE. Response to treatment in dysaesthetic vulvodynia. J Obstet Gynecol. 2001;21(6):610-613.
11. McKay M. Dysesthetic (“essential”) vulvodynia: treatment with amitriptyline. J Reprod Med. 1993;38(1):9-13.
12. Dworkin RH, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237-251.
13. Harris G, Horowitz B, Borgida A. Evaluation of gabapentin in the treatment of generalized vulvodynia unprovoked. J Reprod Med. 2007;52(2):103-106.
14. Ben-David B, Friedman M. Gabapentin therapy for vulvodynia. Anesth Analg. 1999;89(6):1459-1460.
15. Meltzer-Brody SE, Zolnoun D, Steege JF, Rinaldi KL, Leserman J. Open-label trial of lamotrigine focusing on efficacy in vulvodynia. J Reprod Med. 2009;54(3):171-178.
16. Jerome L. Pregabalin-induced remission in a 62-year-old woman with a 20-year history of vulvodynia. Pain Res Manag. 2007;12(3):212-214.
17. Steinberg AC, Oyama IA, Rejba AE, Kellogg-Spadt S, Whitmore KE. Capsaicin for the treatment of vulvar vestibulitis. Am J Obstet Gynecol. 2005;192(5):1549-1553.
18. Murina F, Radici G, Bianco V. Capsaicin and the treatment of vulvar vestibulitis syndrome: a valuable alternative? Med General Med. 2004;6(4):48.-
19. Park AJ, Paraiso MFR. Successful use of botulinum toxin type A in the treatment of refractory postoperative dyspareunia. Obstet Gynecol. 2009;114(2 pt 2):484-487.
20. Brown CS, Glazer HI, Vogt V, Menkes D, Bachmann G. Subjective and objective outcomes of botulinum toxin type A treatment in vestibulodynia: pilot data. J Reprod Med. 2006;51(8):635-641.
21. Dykstra DD, Presthus J. Botulinum toxin type A for the treatment of provoked vestibulodynia: an open-label pilot study. J Reprod Med. 2006;51(6):467-470.
22. Romito S, Bottanelli M, Pellegrini M, Vicentini S, Rizzuto N, Bertolasi L. Botulinum toxin for the treatment of genital pain syndromes. Gynecol Obstet Invest. 2004;58(3):164-167.
23. Bertolasi L, Frasson E, Cappelletti JY, Vicentini S, Bordignon M, Graziottin A. Botulinum neurotoxin type A injections for vaginismus secondary to vulvar vestibulitis syndrome. Obstet Gynecol. 2009;114(5):1008-1016.
24. Presthus JB, Dykstra DD. Botulinum toxin therapy for vulvodynia. NVA News. National Vulvodynia Association. 2007;12(3).
25. Peterson CD, Giraldi A, Lundvall L, Kristensen E. Botulinum toxin type A—a novel treatment for provoked vestibulodynia? Results from a randomized placebo-controlled, double-blinded study. J Sex Med. 2009;6(9):2523-2537.
26. Yoon H, Chung WS, Shim BS. Botulinum toxin A for the management of vulvodynia. Int J Impot Res. 2007;19(1):84-87.
27. Gunter J, Brewer A, Tawfik O. Botulinum toxin A for vulvodynia: a case report. J Pain. 2004;5(4):238-240.
28. Segal D, Tifheret H, Lazr S. Submucous infiltration of betamethasone and lidocaine in the treatment of vulvar vestibulitis. Eur J Obstet Gynecol Reprod Biol. 2003;107(1):105-106.
29. Murina F, Tassan P, Roberti P, Bianco V. Treatment of vulvar vestibulitis with submucous infiltrations of methylprednisolone and lidocaine. An alternative approach. J Reprod Med. 2001;46(8):713-716.
30. Dede M, Yenen MC, Yilmaz A, Baser I. Successful treatment of persistent vulvodynia with submucous infiltration of betamethasone and lidocaine. Eur J Obstet Gynecol Reprod Biol. 2006;124(2):258-259.
31. Dionisi B, Anglana F, Inghirami P, Lippa P, Senatori R. Use of transcutaneous electrical stimulation and biofeedback for the treatment of vulvodynia (vulvar vestibular syndrome): results of 3 years of experience [in Italian]. Minerva Ginecol. 2008;60(6):485-491.
- Part 1: Making the correct diagnosis
(September 2011) - Part 3: Vestibulodynia
(November 2011)
As we discussed in the first installment of this three-part series in the September issue of OBG Management, the causes of vulvar pain are many, and the diagnosis of this common complaint can be difficult. Once the diagnosis of vulvodynia has been made, however, the challenge shifts to finding an effective treatment. Here, our expert panel discusses the many options available, the data (or lack of it) behind each therapy, and what to do in refractory cases.
In Part 3 of this series, in the November issue, the focus will be vestibulodynia.

The lower vagina and vulva are richly supplied with peripheral nerves and are, therefore, sensitive to pain, particularly the region of the hymeneal ring. Although the pudendal nerve (arrow) courses through the area, it is an uncommon source of vulvar pain.
Management of vulvar pain begins with simple measures
Dr. Lonky: How do you approach treatment of vulvar pain syndromes?
Dr. Haefner: I often advise the patient to begin with simple measures. For example, I recommend that she wear cotton underwear during the day, but no underwear at night. If she perspires with exercise, wicking underwear may be helpful. I also counsel the patient to avoid vulvar irritants, douches, and the application of soap of any kind to the vulva. Cool gel packs are sometimes helpful.
When it comes to intercourse, I recommend adequate lubrication using any of a number of effective products, such as olive oil, vitamin E oil, Replens, Slippery Stuff, Astroglide, KY Liquid, and others.
There is an extensive list of lubricants at http://www.med.umich.edu/sexualhealth/resources/guide.htm
Topical agents might offer relief—but so might placebo
Dr. Lonky: What is the role of topical medications, including anesthetics, for treating vulvar pain syndromes?
Dr. Edwards: I don’t find topical medications to be particularly useful in the treatment of vulvodynia, except for lidocaine 2% jelly, or lidocaine 5% ointment, which tends to burn with application—but I never start a patient on only one medication, so judging the effectiveness of a topical therapy is difficult in that context. Good studies of topical medications in the treatment of vulvar pain syndromes are lacking, other than the recent report on amitriptyline and baclofen.1
Dr. Haefner: For minor degrees of pain, consider lidocaine 5% ointment.
Lidocaine/prilocaine (eutectic mixture of local anesthesia or LMX) may be used but can be irritating.
Doxepin 5% cream can be applied to skin daily, gradually increasing the number of daily applications to as many as four.
Topical amitriptyline 2% with baclofen 2% in a water washable base has also been used for point tenderness (squirt 0.5 cc from a syringe onto the finger and apply it to the affected area three times a day).1
Dr. Gunter: Topical estrogen is prescribed by many providers, but we lack studies supporting its efficacy, except for reversing hypoestrogenic changes in postmenopausal women. Some providers use a high-dose, compounded topical estrogen with lidocaine for vestibulodynia. Certainly, local hypoestrogenic changes should be reversed in postmenopausal women before a diagnosis of vulvodynia or vestibulodynia is given.
As for other topical therapies, they are widely used. Some women report improvement with application of plain petrolatum.2 Response rates of 33% to 46% after use of a topical placebo for vestibulodynia are well described in the literature.3,4
Topical analgesics are used frequently, either sporadically (during pain flares) or regularly (daily application). One method of application for localized vestibulodynia involves liberally coating a cotton ball with lidocaine 5% and then applying it to the vestibule overnight (for at least 8 hours of exposure). In this study, after 7 weeks, 76% of women were able to be sexually active, compared with 36% before the start of treatment. However, a randomized, placebo-controlled trial that included lidocaine 5% cream in one arm identified only a 20% reduction in pain for women who had localized vestibulodynia—although, in this trial, the lidocaine was massaged into the vestibule four times daily.5 In this study, interestingly enough, topical lidocaine was less effective than topical placebo, which produced a 33% response rate.3
Lidocaine gel has also been used, although some women report more local irritation with gel than with ointment.
Dr. Lonky: Do we have any data on topical application of other drugs?
Dr. Gunter: Compounded adjuvant medications have been evaluated. In a retrospective study of topical gabapentin in a Lipoderm base, women who had generalized or localized vulvodynia applied a dose of 2%, 4%, or 6% three times daily. Of these women, 80% experienced a reduction of at least 50% in the pain score. In addition, 67% of patients who had localized vestibular pain were able to resume intercourse.6
A retrospective review of 38 women who used 2% amitriptyline and 2% baclofen in a Lipoderm cream for localized vestibular pain found that 53% experienced an improvement in symptoms of at least 60%, but there was no change in the frequency of sexual intercourse.1
Do tricyclic antidepressants ease chronic pain?
Dr. Lonky: Let’s talk, for a moment, about the use of oral tricyclic antidepressants in the treatment of vulvar pain syndromes. What do we know?
Dr. Haefner: Tricyclic antidepressants are a common treatment for vulvar pain. This group of drugs (including amitriptyline [Elavil], nortriptyline [Pamelor], and desipramine [Norpramin]) has been used to treat many idiopathic chronic pain conditions. Published and presented reports indicate that these drugs elicit about a 60% response rate for various pain conditions. A trial by the National Institutes of Health (NIH) is under way, analyzing the use of antidepressants in women who have vulvar pain.
Although treatment with tricyclic antidepressants has generally been reserved for women who have generalized vulvodynia, recent reports have found these medications to be helpful in the treatment of vestibular pain as well. The mechanism of action is thought to be related to inhibition of the reuptake of transmitters—specifically, norepinephrine and serotonin. However, the mechanism of action may be more closely related to anticholinergic effects. Tricyclics affect sodium channels and the N-methyl-d-aspartate (NMDA) receptor.
If you choose to prescribe one of these medications, consider emphasizing to the patient its effect on the sensation of pain rather than its effect on depression.
Dr. Lonky: Are there any types of patients who should not take a tricyclic?
Dr. Haefner: Yes. A patient should not take a tricyclic if she is pregnant, breastfeeding, or planning to conceive. These medicines also add to the effects of alcohol and other central nervous system depressants.
Dr. Lonky: What dosage is recommended?
Dr. Haefner: The dosage for pain control varies, depending on the age of the patient and the particular agent used. Amitriptyline is often used as a first-line medication. I start the patient on 10 to 25 mg nightly and increase that amount by 10 to 25 mg weekly, not to exceed 150 mg daily. A sample regimen might be 10 mg at bedtime for 1 week. If symptoms persist, increase the dose to 20 mg at bedtime for another week, and so on. Once a dose is established that provides relief, the patient should continue to take that amount nightly. Advise the patient not to discontinue the drug abruptly. Rather, it should be weaned.
In patients who are 60 years or older, I give a starting dose of 5 to 10 mg and increase it by 10 mg weekly.
In all age groups, it is important to advise patients to avoid consuming more than one alcoholic beverage daily while taking this medication. And in reproductive-age women, contraception is critical.
Dr. Edwards: I call these drugs tricyclic medications rather than antidepressants. They are extremely useful in managing the neuropathic component of vulvar pain. Despite a recent, apparently well-conducted study showing a lack of benefit, my 25 years of personal clinical experience with tricyclics convince me that I should wait for follow-up studies before abandoning this therapy.3
The pain literature reports that higher doses than previously reported of tricyclic medications are needed for optimal management of neuropathic pain. Doses from 100 to 150 mg are often required for substantial improvement, and a major design flaw in many studies of the effect of tricyclic medications on vulvodynia is the use of an insufficient dose.
Because of their low cost and their effectiveness, tricyclic medications are my first-line therapy for women who do not suffer severe constipation or dry eyes. The effect on depression is a useful side effect, I find.
Dr. Gunter: Although adjuvant medications, such as antidepressants and anticonvulsants, are considered by more than 80% of practitioners to be effective for vulvodynia, it is important to understand that only one randomized, double-blind, placebo-controlled prospective study has evaluated this approach, and that study found a placebo response rate of 33%.3,7
Randomized studies indicate that low-dose amitriptyline (10–20 mg) and desipramine (150 mg) are ineffective for provoked vestibulodynia.3,8 Cohort and retrospective studies with higher doses of amitriptyline (40 to 60 mg/day) indicate that improvement in pain scores of 50% or more can be achieved for 47% to 59% of women who have localized provoked vestibulodynia and generalized unprovoked vulvodynia.9-11
Tricyclic antidepressants and anticonvulsants should be prescribed with caution for patients 65 years and older because they increase the risk of falls.
I give nortriptyline as a first-line agent to women who have both provoked and unprovoked pain. In general, it has fewer anticholinergic side effects than amitriptyline and is generic—it also is taken once daily. For women who have unprovoked pain, I use gabapentin as a second-line agent.
Dr. Lonky: Are any other antidepressants useful in the treatment of vulvar pain?
Dr. Haefner: I sometimes give duloxetine [Cymbalta], starting with an oral daily dose of 30 mg for 1 week. If symptoms persist, I increase the daily dose to a total of 60 mg. (If the patient is depressed, I have her take 30 mg twice daily; if she isn’t depressed, I have her take the full dose of 60 mg in the morning.) I also occasionally utilize venlafaxine [Effexor XR] for pain control, starting with an oral morning dose of 37.5 mg. This dose can be increased to 75 mg/day.
Dr. Edwards: Literature on venlafaxine for neuropathic pain suggests maximal effects at doses of 150 to 225 mg of the extended release formulation, which is often well tolerated. I start patients on 37.5 mg and increase weekly until I reach the 150-mg threshold.12
Are anticonvulsants effective pain relievers?
Dr. Lonky: How effective are oral anticonvulsants such as gabapentin [Neurontin]?
Dr. Haefner: Gabapentin has been used to treat chronic pain conditions. The drug is available in 100-mg, 300-mg, 400-mg, 600-mg, and 800-mg tablets. It is typically initiated at an oral dose of 300 mg daily for 3 days. The dosage is then increased to 300 mg twice daily for 3 days and, finally, to 300 mg three times daily. If necessary, it can gradually be increased to a total of 3,600 mg daily (usually divided into three doses). No more than 1,200 mg should be administered in a single dose. Side effects include somnolence, mental changes, dizziness, and weight gain.
Dr. Edwards: After tricyclic medications, I find gabapentin to be the most beneficial and easily tolerated agent. I give it to patients who have contraindications to tricyclics and who lack a strong component of depression.
Dr. Gunter: Retrospective reviews have found gabapentin to produce improvement of 80% or more in pain scores for 64% to 82% of women who have generalized unprovoked vulvodynia. And a small open-label, prospective trial of lamotrigine [Lamictal] found that it produced statistically significant improvement for generalized vulvodynia.13-15
Dr. Lonky: What do you know about the use of the anticonvulsants pregabalin [Lyrica] and topiramate [Topamax] to treat vulvar pain syndromes?
Dr. Gunter: Pregabalin was reported to reduce symptoms by 80% for generalized, unprovoked vulvodynia in one case report.16
Dr. Edwards: I find that pregabalin is less well tolerated (and more expensive) than gabapentin, so it is one of the last agents I prescribe. I reported a small, uncontrolled series of patients who were treated with pregabalin. Of those who tolerated the drug, two thirds of the women improved by approximately 62%, as judged by a visual analog scale.
Dr. Haefner: Pregabalin is a relatively new addition to the armamentarium. I give 50 mg orally for 4 days to start. If symptoms persist, I increase the dose to 50 mg twice a day for 4 days. If symptoms still persist, I up the dose again to 50 mg three times daily and gradually increase it to 100 mg three times daily, if necessary. Some reports describe a dose as high as 300 mg twice daily (maximum).
As for topiramate, I have been using it much more frequently for vulvodynia and noticing many fewer side effects than with gabapentin.
you offer them?
A patient who has a short duration of pain often responds to topical medications. In contrast, someone who has experienced pain for years is unlikely to get adequate relief from topical medications alone. These patients often require oral tricyclic antidepressants or anticonvulsants, or both. I often start these medications before deciding whether physical therapy is necessary. If the drugs do not provide adequate relief, then I refer the patient to physical therapy.
In some cases, I begin with physical therapy and add other treatments, if necessary. A patient who has localized vulvodynia who tightens her bulbocavernosus and levator ani muscles upon gentle touch may benefit from starting with physical therapy.
I reserve surgery—vestibulectomy—for the patient who has localized pain that has not responded to numerous treatments.
—Hope K. Haefner, MD
Does capsaicin interrupt the pain circuit?
Dr. Lonky: Capsaicin has been mentioned in the literature as a therapy for vulvar pain. Is it effective? How does it work?
Dr. Haefner: Capsaicin activates A-delta sensory neurons and unmyelinated C fibers. It is a vanillyl amide that evokes the sensation of burning pain. It has been proposed as a means of desensitization, which occurs as an acute reaction mediated by neuropeptides (including substance P).17 Steinberg and colleagues found that topical capsaicin significantly decreased pain with intercourse.17 Patients applied capsaicin 0.025% cream for 20 minutes daily for 12 weeks.
In a study by Murina and colleagues, 33 women were treated with topical capsaicin 0.05%. The capsaicin cream was applied to the vulva twice daily for 30 days, then once daily for 30 days, then twice weekly for 4 months. In this study, however, the response to treatment was only partial.18
Dr. Edwards: I have never had a patient willing to try capsaicin after I describe the therapy to them.
Dr. Gunter: Two studies have evaluated daily applications of capsaicin in concentrations of 0.025% and 0.05%—one of them the study by Murina and colleagues that Dr. Haefner mentioned.2,18 The initial release of substance P causes significant burning on application, so pretreatment with local anesthetic to help the patient tolerate the capsaicin is recommended, which could potentially confound the results. In one study, daily pain scores, as well as pain with intercourse, improved significantly for 59% of participants, but no patient experienced complete resolution of symptoms—and within 2 weeks after capsaicin was discontinued, symptoms returned.2,18 I have had only one patient in 15 years of practice who was willing to try capsaicin and who could get past the initial burning.
Another application for botulinum toxin type A?
Dr. Lonky: Is botulinum toxin type A [Botox] at all effective?
Dr. Haefner: Botulinum toxin type A has been utilized to treat provoked vestibulodynia as well as vaginismus and was beneficial.19-23 It blocks the cholinergic innervation of the target tissue. The therapeutic dose ranges from 20 IU to 300 IU.24
A placebo-controlled trial found that injection of 20 IU of botulinum toxin into the vestibule of women with vestibulodynia did not reduce pain, improve sexual functioning, or impact the quality of life, compared with placebo.25 However, this study utilized a lower dose of botulinum toxin than was used in many of the other studies.
Dr. Edwards: I have only used botulinum toxin type A in a low dose. I injected 6 IU of botulinum toxin A into the periphery of the vestibule at 3, 6, 9, and 12 o’clock in six patients, and half improved modestly. I am not prepared to use electromyography (EMG) localization in my office, but from anecdotal reports, as well as several small series and placebo-controlled trials, I would conclude that some patients improve. Those who have hypertonic pelvic floor muscles are likely to be the best candidates for this treatment.
Because the agent relieves pain only modestly, and because it is not covered by insurance for this application, I refer the patient to a gynecologist in my area who administers the drug under EMG localization.
Dr. Gunter: Given the well-documented effect on muscle spasticity, as well as studies that suggest they are also anti-nociceptive agents, botulinum toxins are certainly an attractive concept for vulvodynia. A small case series and a case report indicated significant improvement with vestibular injections of 20 to 40 U of botulinum toxin. However, a randomized, placebo-controlled, double-blind study indicated no significant improvement for women with localized vestibular pain.25-27
I discuss botulinum toxin A with my patients. I explain that my clinical experience does differ from results published in the literature. I find that many women with vestibulodynia opt to try an injection before proceeding to vestibulectomy.
When combined with pelvic floor physical therapy, botulinum toxins are highly effective at treating muscle spasm and can be very useful for women who have a component to their pain of vaginismus or high-tone pelvic floor dysfunction.
How useful are steroids and nerve blocks?
Dr. Lonky: Is there a role for local injections of glucocorticoids or serial nerve blocks?
Dr. Edwards: The occasional patient with very localized pain (trigger point) responds fairly well in my office to intralesional corticosteroids. I have not used or seen reports describing administration of intralesional corticosteroids into a larger area, although two practitioners have told me informally that it is useful in their hands.
As a dermatologist, I cannot perform blocks. I have referred patients to gyn and pain clinics for this purpose, but neither venue has been willing to administer the blocks.
Dr. Haefner: Patients who present with small, localized areas of pain may benefit from local injections. In small areas—for example, a painful spot 1 cm in diameter—triamcinolone acetonide in combination with bupivacaine may be helpful. It is important to use a small dose of steroid in a small area, however, because tissue erosion or ulceration can occur with too high a dose of steroid in the skin. For large areas, as much as 40 mg of triamcinolone acetonide may be utilized in a single monthly dose. Generally, the dose is repeated monthly, if necessary, as many as three or four times.
For large areas, bupivacaine 0.25% is utilized, and for small areas, bupivacaine 0.5% is injected into the vulva along with the steroid. The steroid should be drawn into the syringe first (because the vial can be used at a later time), followed by bupivacaine, which is a single-dose vial.
Pudendal nerve blocks using bupivacaine have been helpful in some patients—particularly those who have unilateral pain.
Dr. Gunter: Local injections with a variety of agents for localized, provoked vestibulodynia have been described, including steroids, botulinum toxins, and interferon. It is important to interpret these studies with caution, however, as placebo response rates with injection therapy are significant.25
A retrospective review of submucous injections of methylprednisolone and lidocaine found that 68% of women had a complete or marked response, and two case reports describe success with betamethasone.26,28-30 I offer steroid injections to women who have vestibulodynia before proceeding to vestibulectomy; I find that about 50% get at least partial relief. As Dr. Haefner indicated from her own experience, my success seems best with steroid injections in the vestibule when the painful area is smaller.
Using injectable steroids and botulinum toxins, I estimate that I can prevent 33% to 40% of vestibulectomies. Although this may not be better than the placebo response rate and certainly represents biased patient selection (patients are not required to try local injection before vestibulectomy for vestibulodynia), those who are successful are uniformly happy for trying it, and those for whom it did not work are not unhappy that they “gave it a try,” as these women are all motivated to avoid surgery, if possible.
Pudendal nerve blocks with triamcinolone are also described for women who have generalized unprovoked vulvodynia due to suspected pudendal neuralgia. Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—have also been performed with good results for generalized vulvodynia. I have had good success with pudendal nerve blocks for unilateral pain that is suspected to be pudendal in origin and also with ganglion impar blocks for women with generalized vulvodynia, especially postmenopausal women. I perform all of my own nerve blocks (FIGURE).
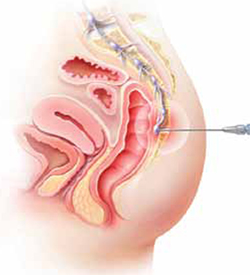
Ganglion impar block
Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—may provide relief from generalized vulvodynia in some women.
Does physical therapy play a role in easing vulvar pain?
Dr. Lonky: What is the role of physical therapy and pelvic floor muscle rehabilitation?
Dr. Gunter: All women who have high-tone pelvic floor dysfunction should be referred to a physical therapist. Many women who lack muscle spasm but experience vulvar pain can still benefit from physical therapy, as gentle stretching and vibration therapy can sometimes be helpful. A physical therapist can also perform biofeedback.
Dr. Edwards: Physical therapy is crucial. It is my first-line therapy overall, with adjunctive oral medication for neuropathic pain. Besides addressing pelvic floor abnormalities, physical therapy can serve as desensitization therapy and psychological support.
Dr. Haefner: Physical therapy has been successful in the treatment of a number of disorders, including migraine and tension headaches, asthma, and anxiety disorders. It is also used in the treatment of vulvar pain. Physical therapists who have experience in vulvar pain may be extremely helpful, particularly if there is concomitant vaginismus—which isn’t uncommon in this population.
For vulvodynia, techniques include internal (vaginal and rectal) and external soft-tissue mobilization and myofascial release; trigger-point pressure; visceral, urogenital, and joint manipulation; electrical stimulation; therapeutic exercises; active pelvic floor retraining; biofeedback; bladder and bowel retraining; and therapeutic ultrasound.
Biofeedback may be used to assist in developing self-regulation strategies for confronting and reducing pain. Patients who have vestibular pain in general have an increased resting tone and a decreased contraction tone. With the aid of an electronic measurement and amplification system or biofeedback machine, an individual can view a display of numbers on a meter, or colored lights, to assess nerve and muscle tension. In this way, she may be able to develop voluntary control over the biological systems involved in pain, discomfort, and disease.
The duration of physical therapy overall and the frequency of visits varies from person to person. Success rates in the range of 60% to 80% have been reported.
How should we respond when medical treatment fails?
Dr. Lonky: What is the proper approach to the patient who has recalcitrant vulvar pain who fails all medical treatments and is not a candidate for vestibulectomy because her pain is outside the vestibule?
Dr. Edwards: The pain clinic. Actually, in a perfect world, the role of the gynecologist or dermatologist would be to give the patient a diagnosis, after which a pain clinic would offer treatment.
All patients should receive counseling. And clinicians who lack expertise should refer the patient to a vulvodynia specialist.
Dr. Haefner: This type of patient may benefit from physical therapy. Bupivacaine steroid injections could also be considered. A sacral nerve stimulator should be considered if the other measures fail to provide adequate relief.
I agree that counseling is extremely helpful in the patient who has vulvodynia. Sexual counseling, with tips on positions for intercourse, lubricants, and control of uncomfortable situations, is of utmost importance.
Dr. Gunter: I offer oral medications and nerve blocks (typically, ganglion impar blocks), and many patients do well.
I also highly recommend advanced programs for mind-body techniques.
Patients who fail all therapies may be candidates for a nerve stimulator, depending on psychiatric comorbidities and response to selective diagnostic nerve blocks.
What’s in the pipeline?
Dr. Lonky: What therapies for vulvar pain are on the horizon?
Dr. Edwards: I believe that cognitive behavioral therapy, sex therapy, and couple counseling will play a larger role in the management of vulvar pain.
Dr. Gunter: Any therapy used in other pain conditions will probably eventually find its way to the management of vulvodynia.
Some investigators believe that Tarlov cysts play a role in vulvar pain and recommend that all women undergo sacral spine and nerve-root magnetic resonance imaging. The problem is that many asymptomatic women have Tarlov cysts, and the surgery to remove them is not at all risk-free. I strongly believe that more research is needed before we can suggest that Tarlov cysts be removed.
Dr. Haefner: Transcutaneous electrical stimulation and biofeedback have been used successfully in the treatment of vulvodynia.31 Some patients benefit from spinal cord stimulators, such as the sacral nerve stimulator, for pain control. Sacral nerve modulation (SNM) works primarily by modulation of the nerve signals to and from the pelvic floor muscles, bladder, and rectum. It applies low-amplitude electrical stimulation to the third sacral nerve via electrodes in a tined lead passing through the S3 foramen, which contains afferent sensory, efferent autonomic motor, and voluntary somatic nerves. Other studies have utilized a different spinal cord level. More studies are needed to demonstrate the full effect of SNM on vulvodynia.
A comprehensive review of the various treatments for vulvodynia can be found in the Journal of Lower Genital Tract Disease.2
Dr. Lonky: Thanks again for your expertise. We’ll focus on provoked vestibulodynia in the final installment of this series on vulvar pain, in the November 2011 issue of OBG Management.
Vulvar pain therapies mentioned in this discussion
| Lifestyle changes Cotton and/or wicking underwear Avoidance of vulvar irritants, douches, soap Use of lubricants during intercourse |
| Physical therapy Internal (vaginal and rectal) and external soft-tissue mobilization and myofascial release Trigger-point pressure Visceral, urogenital, and joint manipulation Electrical stimulation Therapeutic exercises Active pelvic floor retraining Biofeedback Bladder and bowel retraining Therapeutic ultrasound |
| Topical agents Lidocaine 2% jelly Lidocaine 5% ointment Lidocaine/prilocaine Doxepin 5% cream Amitriptyline 2%/baclofen 2% Estrogen Petrolatum Gabapentin |
Oral agents Tricyclic antidepressants
Other antidepressants
Anticonvulsants
|
| Other agents Capsaicin Botulinum toxin type A Corticosteroids Nerve block |
We want to hear from you! Tell us what you think.
- Part 1: Making the correct diagnosis
(September 2011) - Part 3: Vestibulodynia
(November 2011)
As we discussed in the first installment of this three-part series in the September issue of OBG Management, the causes of vulvar pain are many, and the diagnosis of this common complaint can be difficult. Once the diagnosis of vulvodynia has been made, however, the challenge shifts to finding an effective treatment. Here, our expert panel discusses the many options available, the data (or lack of it) behind each therapy, and what to do in refractory cases.
In Part 3 of this series, in the November issue, the focus will be vestibulodynia.

The lower vagina and vulva are richly supplied with peripheral nerves and are, therefore, sensitive to pain, particularly the region of the hymeneal ring. Although the pudendal nerve (arrow) courses through the area, it is an uncommon source of vulvar pain.
Management of vulvar pain begins with simple measures
Dr. Lonky: How do you approach treatment of vulvar pain syndromes?
Dr. Haefner: I often advise the patient to begin with simple measures. For example, I recommend that she wear cotton underwear during the day, but no underwear at night. If she perspires with exercise, wicking underwear may be helpful. I also counsel the patient to avoid vulvar irritants, douches, and the application of soap of any kind to the vulva. Cool gel packs are sometimes helpful.
When it comes to intercourse, I recommend adequate lubrication using any of a number of effective products, such as olive oil, vitamin E oil, Replens, Slippery Stuff, Astroglide, KY Liquid, and others.
There is an extensive list of lubricants at http://www.med.umich.edu/sexualhealth/resources/guide.htm
Topical agents might offer relief—but so might placebo
Dr. Lonky: What is the role of topical medications, including anesthetics, for treating vulvar pain syndromes?
Dr. Edwards: I don’t find topical medications to be particularly useful in the treatment of vulvodynia, except for lidocaine 2% jelly, or lidocaine 5% ointment, which tends to burn with application—but I never start a patient on only one medication, so judging the effectiveness of a topical therapy is difficult in that context. Good studies of topical medications in the treatment of vulvar pain syndromes are lacking, other than the recent report on amitriptyline and baclofen.1
Dr. Haefner: For minor degrees of pain, consider lidocaine 5% ointment.
Lidocaine/prilocaine (eutectic mixture of local anesthesia or LMX) may be used but can be irritating.
Doxepin 5% cream can be applied to skin daily, gradually increasing the number of daily applications to as many as four.
Topical amitriptyline 2% with baclofen 2% in a water washable base has also been used for point tenderness (squirt 0.5 cc from a syringe onto the finger and apply it to the affected area three times a day).1
Dr. Gunter: Topical estrogen is prescribed by many providers, but we lack studies supporting its efficacy, except for reversing hypoestrogenic changes in postmenopausal women. Some providers use a high-dose, compounded topical estrogen with lidocaine for vestibulodynia. Certainly, local hypoestrogenic changes should be reversed in postmenopausal women before a diagnosis of vulvodynia or vestibulodynia is given.
As for other topical therapies, they are widely used. Some women report improvement with application of plain petrolatum.2 Response rates of 33% to 46% after use of a topical placebo for vestibulodynia are well described in the literature.3,4
Topical analgesics are used frequently, either sporadically (during pain flares) or regularly (daily application). One method of application for localized vestibulodynia involves liberally coating a cotton ball with lidocaine 5% and then applying it to the vestibule overnight (for at least 8 hours of exposure). In this study, after 7 weeks, 76% of women were able to be sexually active, compared with 36% before the start of treatment. However, a randomized, placebo-controlled trial that included lidocaine 5% cream in one arm identified only a 20% reduction in pain for women who had localized vestibulodynia—although, in this trial, the lidocaine was massaged into the vestibule four times daily.5 In this study, interestingly enough, topical lidocaine was less effective than topical placebo, which produced a 33% response rate.3
Lidocaine gel has also been used, although some women report more local irritation with gel than with ointment.
Dr. Lonky: Do we have any data on topical application of other drugs?
Dr. Gunter: Compounded adjuvant medications have been evaluated. In a retrospective study of topical gabapentin in a Lipoderm base, women who had generalized or localized vulvodynia applied a dose of 2%, 4%, or 6% three times daily. Of these women, 80% experienced a reduction of at least 50% in the pain score. In addition, 67% of patients who had localized vestibular pain were able to resume intercourse.6
A retrospective review of 38 women who used 2% amitriptyline and 2% baclofen in a Lipoderm cream for localized vestibular pain found that 53% experienced an improvement in symptoms of at least 60%, but there was no change in the frequency of sexual intercourse.1
Do tricyclic antidepressants ease chronic pain?
Dr. Lonky: Let’s talk, for a moment, about the use of oral tricyclic antidepressants in the treatment of vulvar pain syndromes. What do we know?
Dr. Haefner: Tricyclic antidepressants are a common treatment for vulvar pain. This group of drugs (including amitriptyline [Elavil], nortriptyline [Pamelor], and desipramine [Norpramin]) has been used to treat many idiopathic chronic pain conditions. Published and presented reports indicate that these drugs elicit about a 60% response rate for various pain conditions. A trial by the National Institutes of Health (NIH) is under way, analyzing the use of antidepressants in women who have vulvar pain.
Although treatment with tricyclic antidepressants has generally been reserved for women who have generalized vulvodynia, recent reports have found these medications to be helpful in the treatment of vestibular pain as well. The mechanism of action is thought to be related to inhibition of the reuptake of transmitters—specifically, norepinephrine and serotonin. However, the mechanism of action may be more closely related to anticholinergic effects. Tricyclics affect sodium channels and the N-methyl-d-aspartate (NMDA) receptor.
If you choose to prescribe one of these medications, consider emphasizing to the patient its effect on the sensation of pain rather than its effect on depression.
Dr. Lonky: Are there any types of patients who should not take a tricyclic?
Dr. Haefner: Yes. A patient should not take a tricyclic if she is pregnant, breastfeeding, or planning to conceive. These medicines also add to the effects of alcohol and other central nervous system depressants.
Dr. Lonky: What dosage is recommended?
Dr. Haefner: The dosage for pain control varies, depending on the age of the patient and the particular agent used. Amitriptyline is often used as a first-line medication. I start the patient on 10 to 25 mg nightly and increase that amount by 10 to 25 mg weekly, not to exceed 150 mg daily. A sample regimen might be 10 mg at bedtime for 1 week. If symptoms persist, increase the dose to 20 mg at bedtime for another week, and so on. Once a dose is established that provides relief, the patient should continue to take that amount nightly. Advise the patient not to discontinue the drug abruptly. Rather, it should be weaned.
In patients who are 60 years or older, I give a starting dose of 5 to 10 mg and increase it by 10 mg weekly.
In all age groups, it is important to advise patients to avoid consuming more than one alcoholic beverage daily while taking this medication. And in reproductive-age women, contraception is critical.
Dr. Edwards: I call these drugs tricyclic medications rather than antidepressants. They are extremely useful in managing the neuropathic component of vulvar pain. Despite a recent, apparently well-conducted study showing a lack of benefit, my 25 years of personal clinical experience with tricyclics convince me that I should wait for follow-up studies before abandoning this therapy.3
The pain literature reports that higher doses than previously reported of tricyclic medications are needed for optimal management of neuropathic pain. Doses from 100 to 150 mg are often required for substantial improvement, and a major design flaw in many studies of the effect of tricyclic medications on vulvodynia is the use of an insufficient dose.
Because of their low cost and their effectiveness, tricyclic medications are my first-line therapy for women who do not suffer severe constipation or dry eyes. The effect on depression is a useful side effect, I find.
Dr. Gunter: Although adjuvant medications, such as antidepressants and anticonvulsants, are considered by more than 80% of practitioners to be effective for vulvodynia, it is important to understand that only one randomized, double-blind, placebo-controlled prospective study has evaluated this approach, and that study found a placebo response rate of 33%.3,7
Randomized studies indicate that low-dose amitriptyline (10–20 mg) and desipramine (150 mg) are ineffective for provoked vestibulodynia.3,8 Cohort and retrospective studies with higher doses of amitriptyline (40 to 60 mg/day) indicate that improvement in pain scores of 50% or more can be achieved for 47% to 59% of women who have localized provoked vestibulodynia and generalized unprovoked vulvodynia.9-11
Tricyclic antidepressants and anticonvulsants should be prescribed with caution for patients 65 years and older because they increase the risk of falls.
I give nortriptyline as a first-line agent to women who have both provoked and unprovoked pain. In general, it has fewer anticholinergic side effects than amitriptyline and is generic—it also is taken once daily. For women who have unprovoked pain, I use gabapentin as a second-line agent.
Dr. Lonky: Are any other antidepressants useful in the treatment of vulvar pain?
Dr. Haefner: I sometimes give duloxetine [Cymbalta], starting with an oral daily dose of 30 mg for 1 week. If symptoms persist, I increase the daily dose to a total of 60 mg. (If the patient is depressed, I have her take 30 mg twice daily; if she isn’t depressed, I have her take the full dose of 60 mg in the morning.) I also occasionally utilize venlafaxine [Effexor XR] for pain control, starting with an oral morning dose of 37.5 mg. This dose can be increased to 75 mg/day.
Dr. Edwards: Literature on venlafaxine for neuropathic pain suggests maximal effects at doses of 150 to 225 mg of the extended release formulation, which is often well tolerated. I start patients on 37.5 mg and increase weekly until I reach the 150-mg threshold.12
Are anticonvulsants effective pain relievers?
Dr. Lonky: How effective are oral anticonvulsants such as gabapentin [Neurontin]?
Dr. Haefner: Gabapentin has been used to treat chronic pain conditions. The drug is available in 100-mg, 300-mg, 400-mg, 600-mg, and 800-mg tablets. It is typically initiated at an oral dose of 300 mg daily for 3 days. The dosage is then increased to 300 mg twice daily for 3 days and, finally, to 300 mg three times daily. If necessary, it can gradually be increased to a total of 3,600 mg daily (usually divided into three doses). No more than 1,200 mg should be administered in a single dose. Side effects include somnolence, mental changes, dizziness, and weight gain.
Dr. Edwards: After tricyclic medications, I find gabapentin to be the most beneficial and easily tolerated agent. I give it to patients who have contraindications to tricyclics and who lack a strong component of depression.
Dr. Gunter: Retrospective reviews have found gabapentin to produce improvement of 80% or more in pain scores for 64% to 82% of women who have generalized unprovoked vulvodynia. And a small open-label, prospective trial of lamotrigine [Lamictal] found that it produced statistically significant improvement for generalized vulvodynia.13-15
Dr. Lonky: What do you know about the use of the anticonvulsants pregabalin [Lyrica] and topiramate [Topamax] to treat vulvar pain syndromes?
Dr. Gunter: Pregabalin was reported to reduce symptoms by 80% for generalized, unprovoked vulvodynia in one case report.16
Dr. Edwards: I find that pregabalin is less well tolerated (and more expensive) than gabapentin, so it is one of the last agents I prescribe. I reported a small, uncontrolled series of patients who were treated with pregabalin. Of those who tolerated the drug, two thirds of the women improved by approximately 62%, as judged by a visual analog scale.
Dr. Haefner: Pregabalin is a relatively new addition to the armamentarium. I give 50 mg orally for 4 days to start. If symptoms persist, I increase the dose to 50 mg twice a day for 4 days. If symptoms still persist, I up the dose again to 50 mg three times daily and gradually increase it to 100 mg three times daily, if necessary. Some reports describe a dose as high as 300 mg twice daily (maximum).
As for topiramate, I have been using it much more frequently for vulvodynia and noticing many fewer side effects than with gabapentin.
you offer them?
A patient who has a short duration of pain often responds to topical medications. In contrast, someone who has experienced pain for years is unlikely to get adequate relief from topical medications alone. These patients often require oral tricyclic antidepressants or anticonvulsants, or both. I often start these medications before deciding whether physical therapy is necessary. If the drugs do not provide adequate relief, then I refer the patient to physical therapy.
In some cases, I begin with physical therapy and add other treatments, if necessary. A patient who has localized vulvodynia who tightens her bulbocavernosus and levator ani muscles upon gentle touch may benefit from starting with physical therapy.
I reserve surgery—vestibulectomy—for the patient who has localized pain that has not responded to numerous treatments.
—Hope K. Haefner, MD
Does capsaicin interrupt the pain circuit?
Dr. Lonky: Capsaicin has been mentioned in the literature as a therapy for vulvar pain. Is it effective? How does it work?
Dr. Haefner: Capsaicin activates A-delta sensory neurons and unmyelinated C fibers. It is a vanillyl amide that evokes the sensation of burning pain. It has been proposed as a means of desensitization, which occurs as an acute reaction mediated by neuropeptides (including substance P).17 Steinberg and colleagues found that topical capsaicin significantly decreased pain with intercourse.17 Patients applied capsaicin 0.025% cream for 20 minutes daily for 12 weeks.
In a study by Murina and colleagues, 33 women were treated with topical capsaicin 0.05%. The capsaicin cream was applied to the vulva twice daily for 30 days, then once daily for 30 days, then twice weekly for 4 months. In this study, however, the response to treatment was only partial.18
Dr. Edwards: I have never had a patient willing to try capsaicin after I describe the therapy to them.
Dr. Gunter: Two studies have evaluated daily applications of capsaicin in concentrations of 0.025% and 0.05%—one of them the study by Murina and colleagues that Dr. Haefner mentioned.2,18 The initial release of substance P causes significant burning on application, so pretreatment with local anesthetic to help the patient tolerate the capsaicin is recommended, which could potentially confound the results. In one study, daily pain scores, as well as pain with intercourse, improved significantly for 59% of participants, but no patient experienced complete resolution of symptoms—and within 2 weeks after capsaicin was discontinued, symptoms returned.2,18 I have had only one patient in 15 years of practice who was willing to try capsaicin and who could get past the initial burning.
Another application for botulinum toxin type A?
Dr. Lonky: Is botulinum toxin type A [Botox] at all effective?
Dr. Haefner: Botulinum toxin type A has been utilized to treat provoked vestibulodynia as well as vaginismus and was beneficial.19-23 It blocks the cholinergic innervation of the target tissue. The therapeutic dose ranges from 20 IU to 300 IU.24
A placebo-controlled trial found that injection of 20 IU of botulinum toxin into the vestibule of women with vestibulodynia did not reduce pain, improve sexual functioning, or impact the quality of life, compared with placebo.25 However, this study utilized a lower dose of botulinum toxin than was used in many of the other studies.
Dr. Edwards: I have only used botulinum toxin type A in a low dose. I injected 6 IU of botulinum toxin A into the periphery of the vestibule at 3, 6, 9, and 12 o’clock in six patients, and half improved modestly. I am not prepared to use electromyography (EMG) localization in my office, but from anecdotal reports, as well as several small series and placebo-controlled trials, I would conclude that some patients improve. Those who have hypertonic pelvic floor muscles are likely to be the best candidates for this treatment.
Because the agent relieves pain only modestly, and because it is not covered by insurance for this application, I refer the patient to a gynecologist in my area who administers the drug under EMG localization.
Dr. Gunter: Given the well-documented effect on muscle spasticity, as well as studies that suggest they are also anti-nociceptive agents, botulinum toxins are certainly an attractive concept for vulvodynia. A small case series and a case report indicated significant improvement with vestibular injections of 20 to 40 U of botulinum toxin. However, a randomized, placebo-controlled, double-blind study indicated no significant improvement for women with localized vestibular pain.25-27
I discuss botulinum toxin A with my patients. I explain that my clinical experience does differ from results published in the literature. I find that many women with vestibulodynia opt to try an injection before proceeding to vestibulectomy.
When combined with pelvic floor physical therapy, botulinum toxins are highly effective at treating muscle spasm and can be very useful for women who have a component to their pain of vaginismus or high-tone pelvic floor dysfunction.
How useful are steroids and nerve blocks?
Dr. Lonky: Is there a role for local injections of glucocorticoids or serial nerve blocks?
Dr. Edwards: The occasional patient with very localized pain (trigger point) responds fairly well in my office to intralesional corticosteroids. I have not used or seen reports describing administration of intralesional corticosteroids into a larger area, although two practitioners have told me informally that it is useful in their hands.
As a dermatologist, I cannot perform blocks. I have referred patients to gyn and pain clinics for this purpose, but neither venue has been willing to administer the blocks.
Dr. Haefner: Patients who present with small, localized areas of pain may benefit from local injections. In small areas—for example, a painful spot 1 cm in diameter—triamcinolone acetonide in combination with bupivacaine may be helpful. It is important to use a small dose of steroid in a small area, however, because tissue erosion or ulceration can occur with too high a dose of steroid in the skin. For large areas, as much as 40 mg of triamcinolone acetonide may be utilized in a single monthly dose. Generally, the dose is repeated monthly, if necessary, as many as three or four times.
For large areas, bupivacaine 0.25% is utilized, and for small areas, bupivacaine 0.5% is injected into the vulva along with the steroid. The steroid should be drawn into the syringe first (because the vial can be used at a later time), followed by bupivacaine, which is a single-dose vial.
Pudendal nerve blocks using bupivacaine have been helpful in some patients—particularly those who have unilateral pain.
Dr. Gunter: Local injections with a variety of agents for localized, provoked vestibulodynia have been described, including steroids, botulinum toxins, and interferon. It is important to interpret these studies with caution, however, as placebo response rates with injection therapy are significant.25
A retrospective review of submucous injections of methylprednisolone and lidocaine found that 68% of women had a complete or marked response, and two case reports describe success with betamethasone.26,28-30 I offer steroid injections to women who have vestibulodynia before proceeding to vestibulectomy; I find that about 50% get at least partial relief. As Dr. Haefner indicated from her own experience, my success seems best with steroid injections in the vestibule when the painful area is smaller.
Using injectable steroids and botulinum toxins, I estimate that I can prevent 33% to 40% of vestibulectomies. Although this may not be better than the placebo response rate and certainly represents biased patient selection (patients are not required to try local injection before vestibulectomy for vestibulodynia), those who are successful are uniformly happy for trying it, and those for whom it did not work are not unhappy that they “gave it a try,” as these women are all motivated to avoid surgery, if possible.
Pudendal nerve blocks with triamcinolone are also described for women who have generalized unprovoked vulvodynia due to suspected pudendal neuralgia. Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—have also been performed with good results for generalized vulvodynia. I have had good success with pudendal nerve blocks for unilateral pain that is suspected to be pudendal in origin and also with ganglion impar blocks for women with generalized vulvodynia, especially postmenopausal women. I perform all of my own nerve blocks (FIGURE).
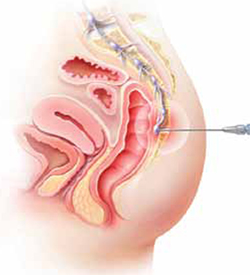
Ganglion impar block
Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—may provide relief from generalized vulvodynia in some women.
Does physical therapy play a role in easing vulvar pain?
Dr. Lonky: What is the role of physical therapy and pelvic floor muscle rehabilitation?
Dr. Gunter: All women who have high-tone pelvic floor dysfunction should be referred to a physical therapist. Many women who lack muscle spasm but experience vulvar pain can still benefit from physical therapy, as gentle stretching and vibration therapy can sometimes be helpful. A physical therapist can also perform biofeedback.
Dr. Edwards: Physical therapy is crucial. It is my first-line therapy overall, with adjunctive oral medication for neuropathic pain. Besides addressing pelvic floor abnormalities, physical therapy can serve as desensitization therapy and psychological support.
Dr. Haefner: Physical therapy has been successful in the treatment of a number of disorders, including migraine and tension headaches, asthma, and anxiety disorders. It is also used in the treatment of vulvar pain. Physical therapists who have experience in vulvar pain may be extremely helpful, particularly if there is concomitant vaginismus—which isn’t uncommon in this population.
For vulvodynia, techniques include internal (vaginal and rectal) and external soft-tissue mobilization and myofascial release; trigger-point pressure; visceral, urogenital, and joint manipulation; electrical stimulation; therapeutic exercises; active pelvic floor retraining; biofeedback; bladder and bowel retraining; and therapeutic ultrasound.
Biofeedback may be used to assist in developing self-regulation strategies for confronting and reducing pain. Patients who have vestibular pain in general have an increased resting tone and a decreased contraction tone. With the aid of an electronic measurement and amplification system or biofeedback machine, an individual can view a display of numbers on a meter, or colored lights, to assess nerve and muscle tension. In this way, she may be able to develop voluntary control over the biological systems involved in pain, discomfort, and disease.
The duration of physical therapy overall and the frequency of visits varies from person to person. Success rates in the range of 60% to 80% have been reported.
How should we respond when medical treatment fails?
Dr. Lonky: What is the proper approach to the patient who has recalcitrant vulvar pain who fails all medical treatments and is not a candidate for vestibulectomy because her pain is outside the vestibule?
Dr. Edwards: The pain clinic. Actually, in a perfect world, the role of the gynecologist or dermatologist would be to give the patient a diagnosis, after which a pain clinic would offer treatment.
All patients should receive counseling. And clinicians who lack expertise should refer the patient to a vulvodynia specialist.
Dr. Haefner: This type of patient may benefit from physical therapy. Bupivacaine steroid injections could also be considered. A sacral nerve stimulator should be considered if the other measures fail to provide adequate relief.
I agree that counseling is extremely helpful in the patient who has vulvodynia. Sexual counseling, with tips on positions for intercourse, lubricants, and control of uncomfortable situations, is of utmost importance.
Dr. Gunter: I offer oral medications and nerve blocks (typically, ganglion impar blocks), and many patients do well.
I also highly recommend advanced programs for mind-body techniques.
Patients who fail all therapies may be candidates for a nerve stimulator, depending on psychiatric comorbidities and response to selective diagnostic nerve blocks.
What’s in the pipeline?
Dr. Lonky: What therapies for vulvar pain are on the horizon?
Dr. Edwards: I believe that cognitive behavioral therapy, sex therapy, and couple counseling will play a larger role in the management of vulvar pain.
Dr. Gunter: Any therapy used in other pain conditions will probably eventually find its way to the management of vulvodynia.
Some investigators believe that Tarlov cysts play a role in vulvar pain and recommend that all women undergo sacral spine and nerve-root magnetic resonance imaging. The problem is that many asymptomatic women have Tarlov cysts, and the surgery to remove them is not at all risk-free. I strongly believe that more research is needed before we can suggest that Tarlov cysts be removed.
Dr. Haefner: Transcutaneous electrical stimulation and biofeedback have been used successfully in the treatment of vulvodynia.31 Some patients benefit from spinal cord stimulators, such as the sacral nerve stimulator, for pain control. Sacral nerve modulation (SNM) works primarily by modulation of the nerve signals to and from the pelvic floor muscles, bladder, and rectum. It applies low-amplitude electrical stimulation to the third sacral nerve via electrodes in a tined lead passing through the S3 foramen, which contains afferent sensory, efferent autonomic motor, and voluntary somatic nerves. Other studies have utilized a different spinal cord level. More studies are needed to demonstrate the full effect of SNM on vulvodynia.
A comprehensive review of the various treatments for vulvodynia can be found in the Journal of Lower Genital Tract Disease.2
Dr. Lonky: Thanks again for your expertise. We’ll focus on provoked vestibulodynia in the final installment of this series on vulvar pain, in the November 2011 issue of OBG Management.
Vulvar pain therapies mentioned in this discussion
| Lifestyle changes Cotton and/or wicking underwear Avoidance of vulvar irritants, douches, soap Use of lubricants during intercourse |
| Physical therapy Internal (vaginal and rectal) and external soft-tissue mobilization and myofascial release Trigger-point pressure Visceral, urogenital, and joint manipulation Electrical stimulation Therapeutic exercises Active pelvic floor retraining Biofeedback Bladder and bowel retraining Therapeutic ultrasound |
| Topical agents Lidocaine 2% jelly Lidocaine 5% ointment Lidocaine/prilocaine Doxepin 5% cream Amitriptyline 2%/baclofen 2% Estrogen Petrolatum Gabapentin |
Oral agents Tricyclic antidepressants
Other antidepressants
Anticonvulsants
|
| Other agents Capsaicin Botulinum toxin type A Corticosteroids Nerve block |
We want to hear from you! Tell us what you think.
1. Nyirjesy P, Lev-Sagie A, Mathew L, Culhane JF. Topical amitriptyline-baclofen cream for the treatment of provoked vestibulodynia. J Lower Genital Tract Dis. 2009;13(4):230-236.
2. Haefner HK, Collins ME, Davis GD, et al. The vulvodynia guideline. J Lower Genital Tract Dis. 2005;9(1):40-51.
3. Foster DC, Kotok MB, Huang L, et al. Oral desipramine and topical lidocaine for vulvodynia: a randomized controlled trial. Obstet Gynecol. 2010;116(3):583-593.
4. Nyirjesy P, Sobel JD, Weitz MV, Leaman DJ, Small MJ, Gelone SP. Cromolyn cream for recalcitrant idiopathic vulvar vestibulitis: results of a placebo-controlled trial. Sex Transm Infect. 2001;77(1):53-57.
5. Zolnoun DA, Hartmann KE, Steege JF. Overnight 5% lidocaine ointment for treatment of vulvar vestibulitis. Obstet Gynecol. 2003;102(1):84-87.
6. Boardman LA, Cooper AS, Blais LR, Raker CA. Topical gabapentin in the treatment of localized and generalized vulvodynia. Obstet Gynecol. 2008;112(3):579-585.
7. Reed BD, Haefner HK, Edwards L. A survey on diagnosis and treatment of vulvodynia researchers and members of the International Society for the Study of Vulvovaginal Disease. J Reprod Med. 2008;53(12):921-929.
8. Brown CS, Wan J, Bachmann G, Rosen R. Self-management amitriptyline, and amitriptyline plus triamcinolone in the management of vulvodynia. J Women Health (Larchmt). 2009;18(2):163-169.
9. Reed BD, Caron AM, Gorenflo DW, Haefner HK. Treatment of vulvodynia with tricyclic antidepressants: efficacy and associated factors. J Low Genit Tract Dis. 2006;10(4):245-251.
10. Munday PE. Response to treatment in dysaesthetic vulvodynia. J Obstet Gynecol. 2001;21(6):610-613.
11. McKay M. Dysesthetic (“essential”) vulvodynia: treatment with amitriptyline. J Reprod Med. 1993;38(1):9-13.
12. Dworkin RH, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237-251.
13. Harris G, Horowitz B, Borgida A. Evaluation of gabapentin in the treatment of generalized vulvodynia unprovoked. J Reprod Med. 2007;52(2):103-106.
14. Ben-David B, Friedman M. Gabapentin therapy for vulvodynia. Anesth Analg. 1999;89(6):1459-1460.
15. Meltzer-Brody SE, Zolnoun D, Steege JF, Rinaldi KL, Leserman J. Open-label trial of lamotrigine focusing on efficacy in vulvodynia. J Reprod Med. 2009;54(3):171-178.
16. Jerome L. Pregabalin-induced remission in a 62-year-old woman with a 20-year history of vulvodynia. Pain Res Manag. 2007;12(3):212-214.
17. Steinberg AC, Oyama IA, Rejba AE, Kellogg-Spadt S, Whitmore KE. Capsaicin for the treatment of vulvar vestibulitis. Am J Obstet Gynecol. 2005;192(5):1549-1553.
18. Murina F, Radici G, Bianco V. Capsaicin and the treatment of vulvar vestibulitis syndrome: a valuable alternative? Med General Med. 2004;6(4):48.-
19. Park AJ, Paraiso MFR. Successful use of botulinum toxin type A in the treatment of refractory postoperative dyspareunia. Obstet Gynecol. 2009;114(2 pt 2):484-487.
20. Brown CS, Glazer HI, Vogt V, Menkes D, Bachmann G. Subjective and objective outcomes of botulinum toxin type A treatment in vestibulodynia: pilot data. J Reprod Med. 2006;51(8):635-641.
21. Dykstra DD, Presthus J. Botulinum toxin type A for the treatment of provoked vestibulodynia: an open-label pilot study. J Reprod Med. 2006;51(6):467-470.
22. Romito S, Bottanelli M, Pellegrini M, Vicentini S, Rizzuto N, Bertolasi L. Botulinum toxin for the treatment of genital pain syndromes. Gynecol Obstet Invest. 2004;58(3):164-167.
23. Bertolasi L, Frasson E, Cappelletti JY, Vicentini S, Bordignon M, Graziottin A. Botulinum neurotoxin type A injections for vaginismus secondary to vulvar vestibulitis syndrome. Obstet Gynecol. 2009;114(5):1008-1016.
24. Presthus JB, Dykstra DD. Botulinum toxin therapy for vulvodynia. NVA News. National Vulvodynia Association. 2007;12(3).
25. Peterson CD, Giraldi A, Lundvall L, Kristensen E. Botulinum toxin type A—a novel treatment for provoked vestibulodynia? Results from a randomized placebo-controlled, double-blinded study. J Sex Med. 2009;6(9):2523-2537.
26. Yoon H, Chung WS, Shim BS. Botulinum toxin A for the management of vulvodynia. Int J Impot Res. 2007;19(1):84-87.
27. Gunter J, Brewer A, Tawfik O. Botulinum toxin A for vulvodynia: a case report. J Pain. 2004;5(4):238-240.
28. Segal D, Tifheret H, Lazr S. Submucous infiltration of betamethasone and lidocaine in the treatment of vulvar vestibulitis. Eur J Obstet Gynecol Reprod Biol. 2003;107(1):105-106.
29. Murina F, Tassan P, Roberti P, Bianco V. Treatment of vulvar vestibulitis with submucous infiltrations of methylprednisolone and lidocaine. An alternative approach. J Reprod Med. 2001;46(8):713-716.
30. Dede M, Yenen MC, Yilmaz A, Baser I. Successful treatment of persistent vulvodynia with submucous infiltration of betamethasone and lidocaine. Eur J Obstet Gynecol Reprod Biol. 2006;124(2):258-259.
31. Dionisi B, Anglana F, Inghirami P, Lippa P, Senatori R. Use of transcutaneous electrical stimulation and biofeedback for the treatment of vulvodynia (vulvar vestibular syndrome): results of 3 years of experience [in Italian]. Minerva Ginecol. 2008;60(6):485-491.
1. Nyirjesy P, Lev-Sagie A, Mathew L, Culhane JF. Topical amitriptyline-baclofen cream for the treatment of provoked vestibulodynia. J Lower Genital Tract Dis. 2009;13(4):230-236.
2. Haefner HK, Collins ME, Davis GD, et al. The vulvodynia guideline. J Lower Genital Tract Dis. 2005;9(1):40-51.
3. Foster DC, Kotok MB, Huang L, et al. Oral desipramine and topical lidocaine for vulvodynia: a randomized controlled trial. Obstet Gynecol. 2010;116(3):583-593.
4. Nyirjesy P, Sobel JD, Weitz MV, Leaman DJ, Small MJ, Gelone SP. Cromolyn cream for recalcitrant idiopathic vulvar vestibulitis: results of a placebo-controlled trial. Sex Transm Infect. 2001;77(1):53-57.
5. Zolnoun DA, Hartmann KE, Steege JF. Overnight 5% lidocaine ointment for treatment of vulvar vestibulitis. Obstet Gynecol. 2003;102(1):84-87.
6. Boardman LA, Cooper AS, Blais LR, Raker CA. Topical gabapentin in the treatment of localized and generalized vulvodynia. Obstet Gynecol. 2008;112(3):579-585.
7. Reed BD, Haefner HK, Edwards L. A survey on diagnosis and treatment of vulvodynia researchers and members of the International Society for the Study of Vulvovaginal Disease. J Reprod Med. 2008;53(12):921-929.
8. Brown CS, Wan J, Bachmann G, Rosen R. Self-management amitriptyline, and amitriptyline plus triamcinolone in the management of vulvodynia. J Women Health (Larchmt). 2009;18(2):163-169.
9. Reed BD, Caron AM, Gorenflo DW, Haefner HK. Treatment of vulvodynia with tricyclic antidepressants: efficacy and associated factors. J Low Genit Tract Dis. 2006;10(4):245-251.
10. Munday PE. Response to treatment in dysaesthetic vulvodynia. J Obstet Gynecol. 2001;21(6):610-613.
11. McKay M. Dysesthetic (“essential”) vulvodynia: treatment with amitriptyline. J Reprod Med. 1993;38(1):9-13.
12. Dworkin RH, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237-251.
13. Harris G, Horowitz B, Borgida A. Evaluation of gabapentin in the treatment of generalized vulvodynia unprovoked. J Reprod Med. 2007;52(2):103-106.
14. Ben-David B, Friedman M. Gabapentin therapy for vulvodynia. Anesth Analg. 1999;89(6):1459-1460.
15. Meltzer-Brody SE, Zolnoun D, Steege JF, Rinaldi KL, Leserman J. Open-label trial of lamotrigine focusing on efficacy in vulvodynia. J Reprod Med. 2009;54(3):171-178.
16. Jerome L. Pregabalin-induced remission in a 62-year-old woman with a 20-year history of vulvodynia. Pain Res Manag. 2007;12(3):212-214.
17. Steinberg AC, Oyama IA, Rejba AE, Kellogg-Spadt S, Whitmore KE. Capsaicin for the treatment of vulvar vestibulitis. Am J Obstet Gynecol. 2005;192(5):1549-1553.
18. Murina F, Radici G, Bianco V. Capsaicin and the treatment of vulvar vestibulitis syndrome: a valuable alternative? Med General Med. 2004;6(4):48.-
19. Park AJ, Paraiso MFR. Successful use of botulinum toxin type A in the treatment of refractory postoperative dyspareunia. Obstet Gynecol. 2009;114(2 pt 2):484-487.
20. Brown CS, Glazer HI, Vogt V, Menkes D, Bachmann G. Subjective and objective outcomes of botulinum toxin type A treatment in vestibulodynia: pilot data. J Reprod Med. 2006;51(8):635-641.
21. Dykstra DD, Presthus J. Botulinum toxin type A for the treatment of provoked vestibulodynia: an open-label pilot study. J Reprod Med. 2006;51(6):467-470.
22. Romito S, Bottanelli M, Pellegrini M, Vicentini S, Rizzuto N, Bertolasi L. Botulinum toxin for the treatment of genital pain syndromes. Gynecol Obstet Invest. 2004;58(3):164-167.
23. Bertolasi L, Frasson E, Cappelletti JY, Vicentini S, Bordignon M, Graziottin A. Botulinum neurotoxin type A injections for vaginismus secondary to vulvar vestibulitis syndrome. Obstet Gynecol. 2009;114(5):1008-1016.
24. Presthus JB, Dykstra DD. Botulinum toxin therapy for vulvodynia. NVA News. National Vulvodynia Association. 2007;12(3).
25. Peterson CD, Giraldi A, Lundvall L, Kristensen E. Botulinum toxin type A—a novel treatment for provoked vestibulodynia? Results from a randomized placebo-controlled, double-blinded study. J Sex Med. 2009;6(9):2523-2537.
26. Yoon H, Chung WS, Shim BS. Botulinum toxin A for the management of vulvodynia. Int J Impot Res. 2007;19(1):84-87.
27. Gunter J, Brewer A, Tawfik O. Botulinum toxin A for vulvodynia: a case report. J Pain. 2004;5(4):238-240.
28. Segal D, Tifheret H, Lazr S. Submucous infiltration of betamethasone and lidocaine in the treatment of vulvar vestibulitis. Eur J Obstet Gynecol Reprod Biol. 2003;107(1):105-106.
29. Murina F, Tassan P, Roberti P, Bianco V. Treatment of vulvar vestibulitis with submucous infiltrations of methylprednisolone and lidocaine. An alternative approach. J Reprod Med. 2001;46(8):713-716.
30. Dede M, Yenen MC, Yilmaz A, Baser I. Successful treatment of persistent vulvodynia with submucous infiltration of betamethasone and lidocaine. Eur J Obstet Gynecol Reprod Biol. 2006;124(2):258-259.
31. Dionisi B, Anglana F, Inghirami P, Lippa P, Senatori R. Use of transcutaneous electrical stimulation and biofeedback for the treatment of vulvodynia (vulvar vestibular syndrome): results of 3 years of experience [in Italian]. Minerva Ginecol. 2008;60(6):485-491.



