User login
Phase 2 data: Inotuzumab, approved in adults with B-ALL, shows promise in kids, too
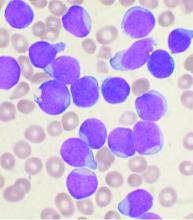
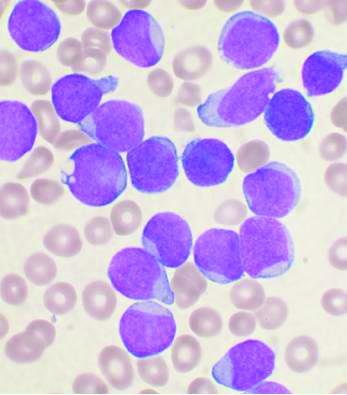
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
ORLANDO – Inotuzumab ozogamicin (InO), a CD22-targeted antibody approved for adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL), showed promising safety and efficacy in children and young adults with R/R B-ALL in a phase 2 trial.
Of 48 patients aged 1-21 years enrolled in the Children’s Oncology Group (COG) Protocol AALL1621 and evaluable for response and toxicity after treatment with the approved adult InO dose, 19 achieved a complete response (CR) and 9 achieved a complete response with incomplete count recovery (CRi) after the first treatment cycle, for an overall CR/CRi rate of 58.3%, Maureen M. O’Brien, MD, reported at the annual meeting of the American Society of Hematology.
Of those with CR/CRi, 19 (65.5%) achieved minimal residual disease less than 0.01%, said Dr. O’Brien, a pediatric hematologist and medical director of the Leukemia/Lymphoma Program at the Cancer and Blood Diseases Institute, Cincinnati Children’s Hospital Medical Center.
Three patients had a partial response (PR), nine had stable disease (SD), and eight had progressive disease (PD), and one of each with PR and SD achieved CR/CRi after a second treatment cycle.
“Of note, two patients who were characterized as [having] progressive disease actually had marrow complete response with incomplete count recovery, but had progressive CNS disease,” she said.
Patients included in the single-arm trial had CD22-positive B-ALL, defined as B-ALL with greater than 20% of blasts expressing CD22, and were in at least their second relapse, were refractory to two prior induction regimens, or had a relapse after hematopoietic stem cell transplantation (HSCT). One exception was that patients with Down syndrome were allowed inclusion after a first relapse, she noted.
Median patient age was 9 years, four patients had CNS 3 status, three had Down syndrome, and most were heavily pretreated, with 32 in at least their second relapse.
“Most patients had significant marrow disease burden, with a median marrow blast percentage of 81%,” Dr. O’Brien said. “In terms of prior therapy, 23% had prior transplant, 23% had prior CD19 [chimeric antigen receptor (CAR)] T-cell therapy – including two patients with prior CD22 CAR T, and 29% of patients had received prior blinatumomab.”
All patients received one cycle of InO at a dose of 1.8mg/m2, with .8mg/m2 given on day 1 and 0.5mg/m2 given on days 8 and 15. Intrathecal therapy was determined based on CNS status.
Patients with at least stable disease at day 28 were eligible for a second cycle; those with CR or CRi received InO at a dose of 0.5 mg/m2 on days 1, 8, and 15 in cycle 2, and those without CR/CRi received the same fractionated dose as in cycle 1. Patients with CR/CRi after two cycles were eligible for up to six total cycles at investigator discretion, Dr. O’Brien explained, adding that 26 of 40 patients eligible for cycle 2 proceeded, including 13 of 18 with MRD less than .01%, 6 of 10 with MRD of 0.01% or greater, and 7 of 12 with PR/SD.
After cycle 2, all 13 with MRD less than .01% maintained that MRD level, 3 of 6 with MRD of .01% or greater achieved MRD less than .01%, 2 of 7 with PR/SD achieved CRi with MRD of .01% or greater – and one of those 2 was MRD negative after a third cycle.
Seven patients received three or more cycles.
“Therapy was extremely well tolerated,” Dr. O’Brien said, noting that the most common nonhematological grade 3 or higher adverse events occurring in at least 5% of patients in cycle 1 were febrile neutropenia and infection, occurring in 27.1% and 16.7% of patients, respectively. “But toxicity was quite minimal.”
Hepatic toxicity included four cases of grade 3 alanine transaminase and one grade 3 bilirubin toxicity in cycle 1, and one grade 3 ALT in cycle 2.
“Importantly, there were no inotuzumab dose modifications or delays due to hepatic toxicity,” she said.
Nine patients experienced 11 dose-limiting toxicities in cycle 1, including 7 involving prolonged count recovery beyond day 42, which was not attributable to disease, and 4 nonhematologic events, including drug reaction with eosinophilia and systemic symptoms, bronchopulmonary hemorrhage, respiratory distress, and a postintrathecal methotrexate stroke.
Sinusoidal obstruction syndrome (SOS) developed in 5 of the 48 patients, all in patients who underwent transplant after InO treatment. Only one of the five had undergone a prior transplant. All SOS cases were grade 3 and were treated with defibrotide; four cases resolved quickly, and one was resolving at the time of death from other causes, she said.
“We found no evidence of association with age, conditioning regimen, SOS prophylaxis, cumulative InO exposure, or time from InO to transplant, bearing in mind that it is a small number of cases, so analysis is limited,” she added.
Central CD22 evaluation in 27 patients with pre– and post–cycle 1 samples showed that 11 of those patients had residual disease at the end of cycle 1.
“There is clearly a subset of patients for whom the resistance mechanism does not seem to have any bearing on CD22, as it was still highly expressed at the time of relapse, but there are a significant number of patients who have downregulation of CD22 expression or a subset of blasts that were CD22 negative at the time of relapse,” she said. “Notably, two of three patients with baseline partial CD22 expression – so less than 90% ... did not achieve a morphologic complete response, and both of these patients had KMT2A rearrangements.”
The findings are important, because 10%-20% of children and young adults with B-ALL will relapse, and therapies that can bridge patients to HSCT or CAR T-cell therapy are critical for improving outcomes, Dr. O’Brien said, explaining that InO, a humanized CD22 IgG4 antibody conjugated to calicheamicin, was approved in adults based on “the impressive results from the INNOVATE trial, compared with chemotherapy,” but prospective data on its efficacy and safety in pediatric patients are lacking.
Retrospective data from a compassionate use program in children demonstrated a response rate of 67% in a heavily pretreated population, and phase 1 data from the ITCC-059 trial presented in a poster at the ASH meeting also showed “quite impressive results,” but a major concern has been hepatic toxicity, including SOS, she said.
Given the observed safety and efficacy in the current phase 2 trial, investigation in children will continue, she said, explaining that “COG is now undertaking a phase 3 trial – AALL1732 – which will randomize patients to chemotherapy [with or without] inotuzumab for patients aged 1-25 with newly diagnosed high-risk B-ALL.”
COG AALL1621 was funded by NCTN grants, St. Baldrick’s Foundation, and Pfizer. Dr. O’Brien reported research funding from Pfizer, Celgene, AbbVie, Amgen, Bristol-Myers Squibb, and BTG.
SOURCE: O’Brien M et al. ASH 2019, Abstract 741.
REPORTING FROM ASH 2019
Deferiprone noninferior to deferoxamine for iron overload in SCD, rare anemias
ORLANDO – The oral iron chelator deferiprone showed noninferiority to deferoxamine for treating iron overload in patients with sickle cell disease and other rare anemias in a randomized open-label trial.
The least squares mean change from baseline in liver iron concentration (LIC) – the primary study endpoint – was –4.04 mg/g dry weight (dw) in 152 patients randomized to receive deferiprone, and –4.45 mg/g dw in 76 who received deferoxamine, Janet L. Kwiatkowski, MD, of the Children’s Hospital of Philadelphia reported at the annual meeting of the American Society of Hematology.
The upper limit of the stringent 96.01% confidence interval used for the evaluation of noninferiority in the study was 1.57, thus the findings demonstrated noninferiority of deferiprone, Dr. Kwiatkowski said.
Deferiprone also showed noninferiority for the secondary endpoints of change in cardiac iron (about –0.02 ms on T2* MRI, log-transformed for both groups) and serum ferritin levels (–415 vs. –750 mcg/L for deferiprone vs. deferoxamine) at 12 months. The difference between the groups was not statistically significant for either endpoint.
Study participants, who had a mean age of 16.9 years, were aged 2 years and older with LIC between 7 and 30 mg/g dw. They were recruited from 33 sites in nine countries and randomized 2:1 to receive deferiprone or deferoxamine for up to 12 months; in patients with lower transfusional iron input and/or less severe iron load, deferiprone was dosed at 75 mg/kg daily and deferoxamine was dosed at 20 mg/kg for children and 40 mg/kg for adults. In those with higher iron input and/or more severe iron load, the deferiprone dose was 99 mg/kg daily and the deferoxamine doses were up to 40 mg/kg in children and up to 50 mg/kg for adults.
“Over the course of the treatment period, the dosage could be adjusted downward if there were side effects, or upward if there was no improvement in iron burden,” Dr Kwiatkowski said, adding that after 12 months, patients had the option of continuing on to a 2-year extension trial in which everyone received deferiprone.
No significant demographic differences were noted between the groups; 84% in both groups had sickle cell disease, and the remaining patients had other, rarer forms of transfusion-dependent anemia. Baseline iron burden was similar in the groups.
The rates of acceptable compliance over the course of the study were also similar at 69% and 79% in the deferiprone and deferoxamine arms, respectively, she noted.
No statistically significant difference between the groups was seen in the overall rate of adverse events, treatment-related AEs, serious AEs, or withdrawals from the study due to AEs. Agranulocytosis occurred in one deferiprone patient and zero deferoxamine patients, and mild or moderate neutropenia occurred in four patients and one patient in the groups, respectively.
All episodes resolved, no difference was seen in the rates of any of the serious AEs, and no unexpected serious adverse events occurred, she said.
Patients with sickle cell disease or other rare anemias whose care includes chronic blood transfusions require iron chelation to prevent iron overload. Currently, only deferoxamine and deferasirox are approved chelators in these patient populations, she said, noting that in 2011 deferiprone received accelerated Food and Drug Administration approval for the treatment of thalassemia.
The current study was conducted because of an FDA requirement for postmarket assessment of deferiprone’s efficacy and safety in patients with sickle cell disease and other anemias who develop transfusional iron overload. It was initiated prior to the approval of deferasirox for the first-line treatment of SCD, therefore it was compared only with deferoxamine, she explained.
Dr. Kwiatkowski reported research funding from Apopharma, bluebird bio, Novartis, and Terumo, and consultancy for Agios, bluebird bio, Celgene, and Imara.
ORLANDO – The oral iron chelator deferiprone showed noninferiority to deferoxamine for treating iron overload in patients with sickle cell disease and other rare anemias in a randomized open-label trial.
The least squares mean change from baseline in liver iron concentration (LIC) – the primary study endpoint – was –4.04 mg/g dry weight (dw) in 152 patients randomized to receive deferiprone, and –4.45 mg/g dw in 76 who received deferoxamine, Janet L. Kwiatkowski, MD, of the Children’s Hospital of Philadelphia reported at the annual meeting of the American Society of Hematology.
The upper limit of the stringent 96.01% confidence interval used for the evaluation of noninferiority in the study was 1.57, thus the findings demonstrated noninferiority of deferiprone, Dr. Kwiatkowski said.
Deferiprone also showed noninferiority for the secondary endpoints of change in cardiac iron (about –0.02 ms on T2* MRI, log-transformed for both groups) and serum ferritin levels (–415 vs. –750 mcg/L for deferiprone vs. deferoxamine) at 12 months. The difference between the groups was not statistically significant for either endpoint.
Study participants, who had a mean age of 16.9 years, were aged 2 years and older with LIC between 7 and 30 mg/g dw. They were recruited from 33 sites in nine countries and randomized 2:1 to receive deferiprone or deferoxamine for up to 12 months; in patients with lower transfusional iron input and/or less severe iron load, deferiprone was dosed at 75 mg/kg daily and deferoxamine was dosed at 20 mg/kg for children and 40 mg/kg for adults. In those with higher iron input and/or more severe iron load, the deferiprone dose was 99 mg/kg daily and the deferoxamine doses were up to 40 mg/kg in children and up to 50 mg/kg for adults.
“Over the course of the treatment period, the dosage could be adjusted downward if there were side effects, or upward if there was no improvement in iron burden,” Dr Kwiatkowski said, adding that after 12 months, patients had the option of continuing on to a 2-year extension trial in which everyone received deferiprone.
No significant demographic differences were noted between the groups; 84% in both groups had sickle cell disease, and the remaining patients had other, rarer forms of transfusion-dependent anemia. Baseline iron burden was similar in the groups.
The rates of acceptable compliance over the course of the study were also similar at 69% and 79% in the deferiprone and deferoxamine arms, respectively, she noted.
No statistically significant difference between the groups was seen in the overall rate of adverse events, treatment-related AEs, serious AEs, or withdrawals from the study due to AEs. Agranulocytosis occurred in one deferiprone patient and zero deferoxamine patients, and mild or moderate neutropenia occurred in four patients and one patient in the groups, respectively.
All episodes resolved, no difference was seen in the rates of any of the serious AEs, and no unexpected serious adverse events occurred, she said.
Patients with sickle cell disease or other rare anemias whose care includes chronic blood transfusions require iron chelation to prevent iron overload. Currently, only deferoxamine and deferasirox are approved chelators in these patient populations, she said, noting that in 2011 deferiprone received accelerated Food and Drug Administration approval for the treatment of thalassemia.
The current study was conducted because of an FDA requirement for postmarket assessment of deferiprone’s efficacy and safety in patients with sickle cell disease and other anemias who develop transfusional iron overload. It was initiated prior to the approval of deferasirox for the first-line treatment of SCD, therefore it was compared only with deferoxamine, she explained.
Dr. Kwiatkowski reported research funding from Apopharma, bluebird bio, Novartis, and Terumo, and consultancy for Agios, bluebird bio, Celgene, and Imara.
ORLANDO – The oral iron chelator deferiprone showed noninferiority to deferoxamine for treating iron overload in patients with sickle cell disease and other rare anemias in a randomized open-label trial.
The least squares mean change from baseline in liver iron concentration (LIC) – the primary study endpoint – was –4.04 mg/g dry weight (dw) in 152 patients randomized to receive deferiprone, and –4.45 mg/g dw in 76 who received deferoxamine, Janet L. Kwiatkowski, MD, of the Children’s Hospital of Philadelphia reported at the annual meeting of the American Society of Hematology.
The upper limit of the stringent 96.01% confidence interval used for the evaluation of noninferiority in the study was 1.57, thus the findings demonstrated noninferiority of deferiprone, Dr. Kwiatkowski said.
Deferiprone also showed noninferiority for the secondary endpoints of change in cardiac iron (about –0.02 ms on T2* MRI, log-transformed for both groups) and serum ferritin levels (–415 vs. –750 mcg/L for deferiprone vs. deferoxamine) at 12 months. The difference between the groups was not statistically significant for either endpoint.
Study participants, who had a mean age of 16.9 years, were aged 2 years and older with LIC between 7 and 30 mg/g dw. They were recruited from 33 sites in nine countries and randomized 2:1 to receive deferiprone or deferoxamine for up to 12 months; in patients with lower transfusional iron input and/or less severe iron load, deferiprone was dosed at 75 mg/kg daily and deferoxamine was dosed at 20 mg/kg for children and 40 mg/kg for adults. In those with higher iron input and/or more severe iron load, the deferiprone dose was 99 mg/kg daily and the deferoxamine doses were up to 40 mg/kg in children and up to 50 mg/kg for adults.
“Over the course of the treatment period, the dosage could be adjusted downward if there were side effects, or upward if there was no improvement in iron burden,” Dr Kwiatkowski said, adding that after 12 months, patients had the option of continuing on to a 2-year extension trial in which everyone received deferiprone.
No significant demographic differences were noted between the groups; 84% in both groups had sickle cell disease, and the remaining patients had other, rarer forms of transfusion-dependent anemia. Baseline iron burden was similar in the groups.
The rates of acceptable compliance over the course of the study were also similar at 69% and 79% in the deferiprone and deferoxamine arms, respectively, she noted.
No statistically significant difference between the groups was seen in the overall rate of adverse events, treatment-related AEs, serious AEs, or withdrawals from the study due to AEs. Agranulocytosis occurred in one deferiprone patient and zero deferoxamine patients, and mild or moderate neutropenia occurred in four patients and one patient in the groups, respectively.
All episodes resolved, no difference was seen in the rates of any of the serious AEs, and no unexpected serious adverse events occurred, she said.
Patients with sickle cell disease or other rare anemias whose care includes chronic blood transfusions require iron chelation to prevent iron overload. Currently, only deferoxamine and deferasirox are approved chelators in these patient populations, she said, noting that in 2011 deferiprone received accelerated Food and Drug Administration approval for the treatment of thalassemia.
The current study was conducted because of an FDA requirement for postmarket assessment of deferiprone’s efficacy and safety in patients with sickle cell disease and other anemias who develop transfusional iron overload. It was initiated prior to the approval of deferasirox for the first-line treatment of SCD, therefore it was compared only with deferoxamine, she explained.
Dr. Kwiatkowski reported research funding from Apopharma, bluebird bio, Novartis, and Terumo, and consultancy for Agios, bluebird bio, Celgene, and Imara.
REPORTING FROM ASH 2019
Phase 2 study shows regimen benefit with dasatinib in Ph+ALL therapy
ORLANDO – A dasatinib-based two-step treatment regimen before allogeneic hematopoietic cell transplantation (alloHCT) for Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL) reduces relapse and toxicity and improves survival versus an imatinib-based approach, according to findings from the phase 2 Ph+ALL213 study.
Of 78 evaluable patients aged 15-64 years with newly diagnosed BCR/ABL1-positive ALL in the single-arm, multicenter study conducted by the Japanese Adult Leukemia Study Group (JALSG), all but one experienced complete remission (CR or CRi) after dasatinib induction (step 1), and 56% achieved molecular complete response (MCR) after intensive consolidation (IC; step 2), Isamu Sugiura, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The MCR rate increased to 66.2% after the first cycle of consolidation, which included high-dose methotrexate/cytarabine followed by 21 days of 100-mg dasatinib (C1), said Dr. Sugiura of the division of hematology and oncology, Toyohashi Municipal Hospital, Japan.
After all cycles of treatment, the MCR rates before and at 30 and 100 days after transplant were 75.9%, 92.7%, and 93.6%, respectively, he added.
The current standard of care of Ph+ALL is tyrosine kinase inhibitor (TKI)-based chemotherapy followed by alloHCT in the first CR, he said noting that deeper MCR at the time of transplant is associated with the best prognosis.
However, early therapy-related mortality, relapse, and non-relapse mortality remain problematic, he said.
JALSG previously reported results from the Ph+ALL202 and Ph+ALL208 studies, which successfully introduced the TKI imatinib into IC followed by alloHCT for newly diagnosed PH+ALL, establishing the standard of care in Japan, Dr. Sugiura said.
“As the next step, Ph+ALL213 was started to evaluate the introduction of dasatinib and two-step chemotherapy,” he said, explaining that 30%-40% of patients in the prior studies were unable to undergo alloHCT at the first CR because of older age, early relapse, or therapy-related death; benefits in Ph+ALL202, for example, were largely seen in patients younger than age 55 years.
Ph+ALL213 was designed to assess to ability of dasatinib to improve efficacy and reduce toxicity in those settings.
Patients with Eastern Cooperative Oncology Group performance status scores of 0-3 and sufficient organ function were enrolled and underwent step 1 (induction), which targeted hematologic complete response (HCR) by day 28 of dasatinib at a dose of 140 mg daily and day 14 of 60 mg/m2 of prednisone, followed by step 2 (IC), which targeted MCR by day 28 of 100-mg dasatinib in combination with CALGB BFM-like intensive chemotherapy, Dr. Sugiura said.
Consolidation included four cycles alternating between the C1 methotrexate/cytarabine/dasatinib regimen and a CHOP-like regimen using vincristine/cyclophosphamide/daunorubicin followed by 21 days of 100-mg dasatinib (C2). Maintenance therapy included 12 cycles of 24 days of 100 mg DA with vincristine/prednisone.
Patients who achieved HCR and had an appropriate donor proceeded to alloHCT after the first cycle of C1 (C1-1), and in those who were minimal residual disease (MRD)–positive just before transplantation, 100 mg dasatinib was given for 10 cycles after alloHCT, whereas MRD-negative patients underwent observation.
Toxicities associated with dasatinib included liver dysfunction in 11 patients (14.1%), and pneumonitis with severe allergic reaction in 1 patient, Dr. Sugiura said, adding that no therapy-related mortality was reported.
Overall, 74.4% of patients underwent transplant, which was significantly greater than the 59.6% who did so in the JALSG Ph+ALL202 trial. Other significant differences between the Ph+ALL213 and 202 trials included the rates of related donor transplants (29.3% vs. 50.8%) and use of reduced-intensity conditioning (31.0% vs. 10.2%), respectively, he said.
At a median follow-up of 48.1 months, 3-year event-free survival in the current trial was 66.2%, and overall survival (OS) was 80.5%, and in the 58 patients who underwent transplant at the first CR, the rates, respectively, were 74.1% and 84.5%. In those with MCR they were 79.5% and 90.9%.
Of note, the presence of additional cytogenetic abnormalities at presentation was associated with worse OS (P = .0346), and the effect was greatest when derivative 22 syndrome was present (P = .00174), Dr. Sugiura said.
MRD state at the time of transplant in first CR also was associated with outcomes; 3-year event-free survival was 79.5% in 44 MRD-negative patients, compared with 57.1% in 14 MRD-positive patients, and 3-year overall survival was 90.9% vs. 64.3%, respectively.
“Survival curves for MRD-positive patients were inferior to those for MRD-negative patients not because of hematological relapse, but because of transplant-related mortality caused by therapy-related complications and gastrointestinal acute [graft-versus-host] disease,” he said.
The findings demonstrate that dasatinib-based two-step induction was highly effective and safe as pretransplant therapy, he said, noting that transplant was “maximally used,” and although 16% of patients relapsed, both relapse- and non-relapse-related mortality were minimized, with rates of 8.6% and 10.3%, respectively, after transplant.
Longer observation and a larger study are required to confirm these findings, Dr. Sugiura said, noting that the phase 2 JALSG Ph+ALL219 study will look at the potential for further improving outcomes with the addition of the multitargeted TKI ponatinib in patients who are MRD-positive after IC.
This study was funded by the Ministry of Health, Labor and Welfare of Japan. Dr. Sugiura reported having no disclosures.
SOURCE: Sugiura I et al. ASH 2019. Abstract 743.
ORLANDO – A dasatinib-based two-step treatment regimen before allogeneic hematopoietic cell transplantation (alloHCT) for Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL) reduces relapse and toxicity and improves survival versus an imatinib-based approach, according to findings from the phase 2 Ph+ALL213 study.
Of 78 evaluable patients aged 15-64 years with newly diagnosed BCR/ABL1-positive ALL in the single-arm, multicenter study conducted by the Japanese Adult Leukemia Study Group (JALSG), all but one experienced complete remission (CR or CRi) after dasatinib induction (step 1), and 56% achieved molecular complete response (MCR) after intensive consolidation (IC; step 2), Isamu Sugiura, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The MCR rate increased to 66.2% after the first cycle of consolidation, which included high-dose methotrexate/cytarabine followed by 21 days of 100-mg dasatinib (C1), said Dr. Sugiura of the division of hematology and oncology, Toyohashi Municipal Hospital, Japan.
After all cycles of treatment, the MCR rates before and at 30 and 100 days after transplant were 75.9%, 92.7%, and 93.6%, respectively, he added.
The current standard of care of Ph+ALL is tyrosine kinase inhibitor (TKI)-based chemotherapy followed by alloHCT in the first CR, he said noting that deeper MCR at the time of transplant is associated with the best prognosis.
However, early therapy-related mortality, relapse, and non-relapse mortality remain problematic, he said.
JALSG previously reported results from the Ph+ALL202 and Ph+ALL208 studies, which successfully introduced the TKI imatinib into IC followed by alloHCT for newly diagnosed PH+ALL, establishing the standard of care in Japan, Dr. Sugiura said.
“As the next step, Ph+ALL213 was started to evaluate the introduction of dasatinib and two-step chemotherapy,” he said, explaining that 30%-40% of patients in the prior studies were unable to undergo alloHCT at the first CR because of older age, early relapse, or therapy-related death; benefits in Ph+ALL202, for example, were largely seen in patients younger than age 55 years.
Ph+ALL213 was designed to assess to ability of dasatinib to improve efficacy and reduce toxicity in those settings.
Patients with Eastern Cooperative Oncology Group performance status scores of 0-3 and sufficient organ function were enrolled and underwent step 1 (induction), which targeted hematologic complete response (HCR) by day 28 of dasatinib at a dose of 140 mg daily and day 14 of 60 mg/m2 of prednisone, followed by step 2 (IC), which targeted MCR by day 28 of 100-mg dasatinib in combination with CALGB BFM-like intensive chemotherapy, Dr. Sugiura said.
Consolidation included four cycles alternating between the C1 methotrexate/cytarabine/dasatinib regimen and a CHOP-like regimen using vincristine/cyclophosphamide/daunorubicin followed by 21 days of 100-mg dasatinib (C2). Maintenance therapy included 12 cycles of 24 days of 100 mg DA with vincristine/prednisone.
Patients who achieved HCR and had an appropriate donor proceeded to alloHCT after the first cycle of C1 (C1-1), and in those who were minimal residual disease (MRD)–positive just before transplantation, 100 mg dasatinib was given for 10 cycles after alloHCT, whereas MRD-negative patients underwent observation.
Toxicities associated with dasatinib included liver dysfunction in 11 patients (14.1%), and pneumonitis with severe allergic reaction in 1 patient, Dr. Sugiura said, adding that no therapy-related mortality was reported.
Overall, 74.4% of patients underwent transplant, which was significantly greater than the 59.6% who did so in the JALSG Ph+ALL202 trial. Other significant differences between the Ph+ALL213 and 202 trials included the rates of related donor transplants (29.3% vs. 50.8%) and use of reduced-intensity conditioning (31.0% vs. 10.2%), respectively, he said.
At a median follow-up of 48.1 months, 3-year event-free survival in the current trial was 66.2%, and overall survival (OS) was 80.5%, and in the 58 patients who underwent transplant at the first CR, the rates, respectively, were 74.1% and 84.5%. In those with MCR they were 79.5% and 90.9%.
Of note, the presence of additional cytogenetic abnormalities at presentation was associated with worse OS (P = .0346), and the effect was greatest when derivative 22 syndrome was present (P = .00174), Dr. Sugiura said.
MRD state at the time of transplant in first CR also was associated with outcomes; 3-year event-free survival was 79.5% in 44 MRD-negative patients, compared with 57.1% in 14 MRD-positive patients, and 3-year overall survival was 90.9% vs. 64.3%, respectively.
“Survival curves for MRD-positive patients were inferior to those for MRD-negative patients not because of hematological relapse, but because of transplant-related mortality caused by therapy-related complications and gastrointestinal acute [graft-versus-host] disease,” he said.
The findings demonstrate that dasatinib-based two-step induction was highly effective and safe as pretransplant therapy, he said, noting that transplant was “maximally used,” and although 16% of patients relapsed, both relapse- and non-relapse-related mortality were minimized, with rates of 8.6% and 10.3%, respectively, after transplant.
Longer observation and a larger study are required to confirm these findings, Dr. Sugiura said, noting that the phase 2 JALSG Ph+ALL219 study will look at the potential for further improving outcomes with the addition of the multitargeted TKI ponatinib in patients who are MRD-positive after IC.
This study was funded by the Ministry of Health, Labor and Welfare of Japan. Dr. Sugiura reported having no disclosures.
SOURCE: Sugiura I et al. ASH 2019. Abstract 743.
ORLANDO – A dasatinib-based two-step treatment regimen before allogeneic hematopoietic cell transplantation (alloHCT) for Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL) reduces relapse and toxicity and improves survival versus an imatinib-based approach, according to findings from the phase 2 Ph+ALL213 study.
Of 78 evaluable patients aged 15-64 years with newly diagnosed BCR/ABL1-positive ALL in the single-arm, multicenter study conducted by the Japanese Adult Leukemia Study Group (JALSG), all but one experienced complete remission (CR or CRi) after dasatinib induction (step 1), and 56% achieved molecular complete response (MCR) after intensive consolidation (IC; step 2), Isamu Sugiura, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The MCR rate increased to 66.2% after the first cycle of consolidation, which included high-dose methotrexate/cytarabine followed by 21 days of 100-mg dasatinib (C1), said Dr. Sugiura of the division of hematology and oncology, Toyohashi Municipal Hospital, Japan.
After all cycles of treatment, the MCR rates before and at 30 and 100 days after transplant were 75.9%, 92.7%, and 93.6%, respectively, he added.
The current standard of care of Ph+ALL is tyrosine kinase inhibitor (TKI)-based chemotherapy followed by alloHCT in the first CR, he said noting that deeper MCR at the time of transplant is associated with the best prognosis.
However, early therapy-related mortality, relapse, and non-relapse mortality remain problematic, he said.
JALSG previously reported results from the Ph+ALL202 and Ph+ALL208 studies, which successfully introduced the TKI imatinib into IC followed by alloHCT for newly diagnosed PH+ALL, establishing the standard of care in Japan, Dr. Sugiura said.
“As the next step, Ph+ALL213 was started to evaluate the introduction of dasatinib and two-step chemotherapy,” he said, explaining that 30%-40% of patients in the prior studies were unable to undergo alloHCT at the first CR because of older age, early relapse, or therapy-related death; benefits in Ph+ALL202, for example, were largely seen in patients younger than age 55 years.
Ph+ALL213 was designed to assess to ability of dasatinib to improve efficacy and reduce toxicity in those settings.
Patients with Eastern Cooperative Oncology Group performance status scores of 0-3 and sufficient organ function were enrolled and underwent step 1 (induction), which targeted hematologic complete response (HCR) by day 28 of dasatinib at a dose of 140 mg daily and day 14 of 60 mg/m2 of prednisone, followed by step 2 (IC), which targeted MCR by day 28 of 100-mg dasatinib in combination with CALGB BFM-like intensive chemotherapy, Dr. Sugiura said.
Consolidation included four cycles alternating between the C1 methotrexate/cytarabine/dasatinib regimen and a CHOP-like regimen using vincristine/cyclophosphamide/daunorubicin followed by 21 days of 100-mg dasatinib (C2). Maintenance therapy included 12 cycles of 24 days of 100 mg DA with vincristine/prednisone.
Patients who achieved HCR and had an appropriate donor proceeded to alloHCT after the first cycle of C1 (C1-1), and in those who were minimal residual disease (MRD)–positive just before transplantation, 100 mg dasatinib was given for 10 cycles after alloHCT, whereas MRD-negative patients underwent observation.
Toxicities associated with dasatinib included liver dysfunction in 11 patients (14.1%), and pneumonitis with severe allergic reaction in 1 patient, Dr. Sugiura said, adding that no therapy-related mortality was reported.
Overall, 74.4% of patients underwent transplant, which was significantly greater than the 59.6% who did so in the JALSG Ph+ALL202 trial. Other significant differences between the Ph+ALL213 and 202 trials included the rates of related donor transplants (29.3% vs. 50.8%) and use of reduced-intensity conditioning (31.0% vs. 10.2%), respectively, he said.
At a median follow-up of 48.1 months, 3-year event-free survival in the current trial was 66.2%, and overall survival (OS) was 80.5%, and in the 58 patients who underwent transplant at the first CR, the rates, respectively, were 74.1% and 84.5%. In those with MCR they were 79.5% and 90.9%.
Of note, the presence of additional cytogenetic abnormalities at presentation was associated with worse OS (P = .0346), and the effect was greatest when derivative 22 syndrome was present (P = .00174), Dr. Sugiura said.
MRD state at the time of transplant in first CR also was associated with outcomes; 3-year event-free survival was 79.5% in 44 MRD-negative patients, compared with 57.1% in 14 MRD-positive patients, and 3-year overall survival was 90.9% vs. 64.3%, respectively.
“Survival curves for MRD-positive patients were inferior to those for MRD-negative patients not because of hematological relapse, but because of transplant-related mortality caused by therapy-related complications and gastrointestinal acute [graft-versus-host] disease,” he said.
The findings demonstrate that dasatinib-based two-step induction was highly effective and safe as pretransplant therapy, he said, noting that transplant was “maximally used,” and although 16% of patients relapsed, both relapse- and non-relapse-related mortality were minimized, with rates of 8.6% and 10.3%, respectively, after transplant.
Longer observation and a larger study are required to confirm these findings, Dr. Sugiura said, noting that the phase 2 JALSG Ph+ALL219 study will look at the potential for further improving outcomes with the addition of the multitargeted TKI ponatinib in patients who are MRD-positive after IC.
This study was funded by the Ministry of Health, Labor and Welfare of Japan. Dr. Sugiura reported having no disclosures.
SOURCE: Sugiura I et al. ASH 2019. Abstract 743.
REPORTING FROM ASH 2019
Experts break down latest CAR T-cell advances in lymphoma
ORLANDO – There’s now mature data surrounding the use of chimeric antigen receptor (CAR) T-cell therapy in lymphoma, and the annual meeting of the American Society of Hematology brought forth additional information from real-world studies, insights about what is driving relapse, and promising data on mantle cell lymphoma.

The roundtable participants included Brian Hill, MD, of the Cleveland Clinic Taussig Cancer Center; Frederick L. Locke, MD, of the Moffit Cancer Center in Tampa, Fla.; and Peter Riedell, MD, of the University of Chicago.
Among the studies highlighted by the panel was the Transcend NHL 001 study (Abstract 241), which looked at third-line use of lisocabtagene maraleucel (liso-cel) in patients with diffuse large B-cell lymphoma, transformed follicular lymphoma, and other indolent non-Hodgkin lymphoma subtypes. More than 300 patients were enrolled, and liso-cel met all primary and secondary efficacy endpoints, with an overall response rate of more than 70%. The notable take-home point from the study was the safety profile, Dr. Riedell noted. Liso-cel was associated with a lower rate of cytokine release syndrome and neurologic toxicity, compared with the currently approved products.
Since patients in the study had a lower incidence and later onset of cytokine release syndrome, liso-cel could be a candidate for outpatient administration, Dr. Locke said. However, doing that would require “significant infrastructure” in hospitals and clinics to properly support patients, especially given that the treatment-related mortality on the study was similar to approved CAR T-cell products at about 3%. “You have to be ready to admit the patient to the hospital very rapidly, and you have to have the providers and the nurses who are vigilant when the patient is not in the hospital,” he said.
Another notable study presented at ASH examined the characteristics and outcomes of patients receiving bridging therapy while awaiting treatment with axicabtagene ciloleucel (Abstract 245). This real-world study adds interesting information to the field because, in some of the studies that were pivotal to the approval of CAR T-cell therapy, bridging therapy was not allowed, Dr. Locke said.
In this analysis, researchers found that the overall survival was worse among patients who received bridging. This finding suggests that patients who received bridging therapy had a different biology or that the therapy itself may have had an effect on the host or tumor microenvironment that affected the efficacy of the CAR T-cell therapy, the researchers reported.
The panel also highlighted the Zuma-2 study, which looked at KTE-X19, an anti-CD19 CAR T-cell therapy, among more than 70 patients with relapsed/refractory mantle cell lymphoma who had failed treatment with a Bruton’s tyrosine kinase inhibitor (Abstract 754). “This was, I thought, kind of a sleeper study at ASH,” said Dr. Hill, who was one of the authors of the study.
The overall response rate was 93% with about two-thirds of patients achieving a complete response. Researchers found that the response was consistent across subgroups, including Ki-67 and patients with prior use of steroids or bridging therapy. Dr. Locke, who was also a study author, said the results are a “game changer.”
“I’m very excited about it,” Dr. Riedell said, noting that these are patients without a lot of treatment options.
The panel also discussed other studies from ASH, including an analysis of tumor tissue samples from patients in the ZUMA-1 trial who had responded and subsequently relapsed (Abstract 203); a multicenter prospective analysis of circulating tumor DNA in diffuse large B-cell lymphoma patients who had relapsed after treatment with axicabtagene ciloleucel (Abstract 884); and the early use of corticosteroids to prevent toxicities in patients in cohort 4 of the ZUMA-1 trial (Abstract 243).
Dr. Hill reported consulting with Juno/Celgene/BMS and Novartis and research and consulting for Kite/Gilead. Dr. Locke reported consulting for Cellular Biomedicine Group and being a scientific adviser to Kite/Gilead, Novartis, Celgene/BMS, GammaDelta Therapeutics, Calibr, and Allogene. Dr. Riedell reported consulting for Bayer and Verastem, consulting for and research funding from Novartis and BMS/Celgene, and consulting for, research funding from, and speaking for Kite.
ORLANDO – There’s now mature data surrounding the use of chimeric antigen receptor (CAR) T-cell therapy in lymphoma, and the annual meeting of the American Society of Hematology brought forth additional information from real-world studies, insights about what is driving relapse, and promising data on mantle cell lymphoma.

The roundtable participants included Brian Hill, MD, of the Cleveland Clinic Taussig Cancer Center; Frederick L. Locke, MD, of the Moffit Cancer Center in Tampa, Fla.; and Peter Riedell, MD, of the University of Chicago.
Among the studies highlighted by the panel was the Transcend NHL 001 study (Abstract 241), which looked at third-line use of lisocabtagene maraleucel (liso-cel) in patients with diffuse large B-cell lymphoma, transformed follicular lymphoma, and other indolent non-Hodgkin lymphoma subtypes. More than 300 patients were enrolled, and liso-cel met all primary and secondary efficacy endpoints, with an overall response rate of more than 70%. The notable take-home point from the study was the safety profile, Dr. Riedell noted. Liso-cel was associated with a lower rate of cytokine release syndrome and neurologic toxicity, compared with the currently approved products.
Since patients in the study had a lower incidence and later onset of cytokine release syndrome, liso-cel could be a candidate for outpatient administration, Dr. Locke said. However, doing that would require “significant infrastructure” in hospitals and clinics to properly support patients, especially given that the treatment-related mortality on the study was similar to approved CAR T-cell products at about 3%. “You have to be ready to admit the patient to the hospital very rapidly, and you have to have the providers and the nurses who are vigilant when the patient is not in the hospital,” he said.
Another notable study presented at ASH examined the characteristics and outcomes of patients receiving bridging therapy while awaiting treatment with axicabtagene ciloleucel (Abstract 245). This real-world study adds interesting information to the field because, in some of the studies that were pivotal to the approval of CAR T-cell therapy, bridging therapy was not allowed, Dr. Locke said.
In this analysis, researchers found that the overall survival was worse among patients who received bridging. This finding suggests that patients who received bridging therapy had a different biology or that the therapy itself may have had an effect on the host or tumor microenvironment that affected the efficacy of the CAR T-cell therapy, the researchers reported.
The panel also highlighted the Zuma-2 study, which looked at KTE-X19, an anti-CD19 CAR T-cell therapy, among more than 70 patients with relapsed/refractory mantle cell lymphoma who had failed treatment with a Bruton’s tyrosine kinase inhibitor (Abstract 754). “This was, I thought, kind of a sleeper study at ASH,” said Dr. Hill, who was one of the authors of the study.
The overall response rate was 93% with about two-thirds of patients achieving a complete response. Researchers found that the response was consistent across subgroups, including Ki-67 and patients with prior use of steroids or bridging therapy. Dr. Locke, who was also a study author, said the results are a “game changer.”
“I’m very excited about it,” Dr. Riedell said, noting that these are patients without a lot of treatment options.
The panel also discussed other studies from ASH, including an analysis of tumor tissue samples from patients in the ZUMA-1 trial who had responded and subsequently relapsed (Abstract 203); a multicenter prospective analysis of circulating tumor DNA in diffuse large B-cell lymphoma patients who had relapsed after treatment with axicabtagene ciloleucel (Abstract 884); and the early use of corticosteroids to prevent toxicities in patients in cohort 4 of the ZUMA-1 trial (Abstract 243).
Dr. Hill reported consulting with Juno/Celgene/BMS and Novartis and research and consulting for Kite/Gilead. Dr. Locke reported consulting for Cellular Biomedicine Group and being a scientific adviser to Kite/Gilead, Novartis, Celgene/BMS, GammaDelta Therapeutics, Calibr, and Allogene. Dr. Riedell reported consulting for Bayer and Verastem, consulting for and research funding from Novartis and BMS/Celgene, and consulting for, research funding from, and speaking for Kite.
ORLANDO – There’s now mature data surrounding the use of chimeric antigen receptor (CAR) T-cell therapy in lymphoma, and the annual meeting of the American Society of Hematology brought forth additional information from real-world studies, insights about what is driving relapse, and promising data on mantle cell lymphoma.

The roundtable participants included Brian Hill, MD, of the Cleveland Clinic Taussig Cancer Center; Frederick L. Locke, MD, of the Moffit Cancer Center in Tampa, Fla.; and Peter Riedell, MD, of the University of Chicago.
Among the studies highlighted by the panel was the Transcend NHL 001 study (Abstract 241), which looked at third-line use of lisocabtagene maraleucel (liso-cel) in patients with diffuse large B-cell lymphoma, transformed follicular lymphoma, and other indolent non-Hodgkin lymphoma subtypes. More than 300 patients were enrolled, and liso-cel met all primary and secondary efficacy endpoints, with an overall response rate of more than 70%. The notable take-home point from the study was the safety profile, Dr. Riedell noted. Liso-cel was associated with a lower rate of cytokine release syndrome and neurologic toxicity, compared with the currently approved products.
Since patients in the study had a lower incidence and later onset of cytokine release syndrome, liso-cel could be a candidate for outpatient administration, Dr. Locke said. However, doing that would require “significant infrastructure” in hospitals and clinics to properly support patients, especially given that the treatment-related mortality on the study was similar to approved CAR T-cell products at about 3%. “You have to be ready to admit the patient to the hospital very rapidly, and you have to have the providers and the nurses who are vigilant when the patient is not in the hospital,” he said.
Another notable study presented at ASH examined the characteristics and outcomes of patients receiving bridging therapy while awaiting treatment with axicabtagene ciloleucel (Abstract 245). This real-world study adds interesting information to the field because, in some of the studies that were pivotal to the approval of CAR T-cell therapy, bridging therapy was not allowed, Dr. Locke said.
In this analysis, researchers found that the overall survival was worse among patients who received bridging. This finding suggests that patients who received bridging therapy had a different biology or that the therapy itself may have had an effect on the host or tumor microenvironment that affected the efficacy of the CAR T-cell therapy, the researchers reported.
The panel also highlighted the Zuma-2 study, which looked at KTE-X19, an anti-CD19 CAR T-cell therapy, among more than 70 patients with relapsed/refractory mantle cell lymphoma who had failed treatment with a Bruton’s tyrosine kinase inhibitor (Abstract 754). “This was, I thought, kind of a sleeper study at ASH,” said Dr. Hill, who was one of the authors of the study.
The overall response rate was 93% with about two-thirds of patients achieving a complete response. Researchers found that the response was consistent across subgroups, including Ki-67 and patients with prior use of steroids or bridging therapy. Dr. Locke, who was also a study author, said the results are a “game changer.”
“I’m very excited about it,” Dr. Riedell said, noting that these are patients without a lot of treatment options.
The panel also discussed other studies from ASH, including an analysis of tumor tissue samples from patients in the ZUMA-1 trial who had responded and subsequently relapsed (Abstract 203); a multicenter prospective analysis of circulating tumor DNA in diffuse large B-cell lymphoma patients who had relapsed after treatment with axicabtagene ciloleucel (Abstract 884); and the early use of corticosteroids to prevent toxicities in patients in cohort 4 of the ZUMA-1 trial (Abstract 243).
Dr. Hill reported consulting with Juno/Celgene/BMS and Novartis and research and consulting for Kite/Gilead. Dr. Locke reported consulting for Cellular Biomedicine Group and being a scientific adviser to Kite/Gilead, Novartis, Celgene/BMS, GammaDelta Therapeutics, Calibr, and Allogene. Dr. Riedell reported consulting for Bayer and Verastem, consulting for and research funding from Novartis and BMS/Celgene, and consulting for, research funding from, and speaking for Kite.
EXPERT ANALYSIS FROM ASH 2019
Sevuparin failed for acute VOC in sickle cell, but may have preventive potential
ORLANDO – Sevuparin, a novel nonanticoagulant heparinoid drug, showed no efficacy for acute vaso-occlusive crisis (VOC) in patients with sickle cell disease (SCD) in the randomized, controlled, phase 2 TVOC01 trial, but its promising safety and broad mechanism of action warrant further exploration in the prodromal VOC setting, according to investigators.
Time to VOC resolution – the primary study endpoint – was similar at about 168 hours in 71 hospitalized patients randomized to receive sevuparin and in 76 who received placebo (intention-to-treat hazard ratio, 0.89), Bart J. Biemond, MD, explained during a presentation of the findings at the annual meeting of the American Society of Hematology.
A per-protocol analysis based on the 69 and 75 patients dosed in the treatment and placebo arms, respectively, showed a similar result (HR, 0.81), said Dr. Biemond of the department of clinical hematology, Amsterdam UMC, Academic Medical Center, the Netherlands.
Secondary endpoints, including mean change in pain intensity from baseline on a visual analogue scale (VAS), duration of severest pain measured as time to achieve a 30% reduction in VAS score from baseline, and cumulative use of parenteral opioids, also did not differ between the treatment and placebo arms, he added.
Patients in the global, double-blind, multicenter trial were aged 12-50 years (median, 22 years) with any type of SCD. They were enrolled from 16 sites in 7 countries to receive a loading dose of 3 mg/kg of sevuparin and continuous 18 mg/kg per day infusions or placebo. Patients in both arms also received standard-of-care and parenteral opioid therapy.
The groups were generally balanced with respect to demographic and baseline characteristics, Dr. Biemond said, noting that the treatment was safe: No serious adverse events occurred, and any mild-to-moderate adverse events were transient.
The findings were disappointing given the lack of approved treatment options other than pain management for acute VOC in hospitalized patients with SCD, and they were somewhat surprising given that preclinical and clinical data in recent years have demonstrated that “you can actually prevent those crises by antiadhesive strategies,” he said.
“So we hypothesized that, if you perform such an antiadhesive strategy in a patient already having a crisis and admitted in the hospital, you may shorten their period of admission and perhaps also shorten the severity of their pain,” he said.
In fact, a single-center, randomized, controlled trial conducted by Qari et al. in 2007 (Thromb Haemost. 2007 Aug;98[2]:392-6) showed that full-dose tinzaparin reduced pain severity and duration of admission among sickle cell patients with acute VOC – perhaps because of the antiadhesive properties of heparin – but that study was never repeated, Dr. Biemond said, noting that those antiadhesive properties have been well documented in animal studies.
“Heparin is able to inhibit P-selectin, L-selectin, thrombospondin, fibronectin, and von Willebrand activity, which are all involved in vaso-occlusion in patients with sickle cell disease, and very likely also involved during a vaso-occlusive crisis,” he explained, adding that sevuparin, a low-molecular-weight heparin without functional antithrombin binding domain, seemed to be a good candidate for testing that hypothesis.
“It has no anticoagulant effects on factor Xa and IIa,” he said. “It retains, however, its antiadhesive and antiaggregation properties.”
Since it has no anticoagulation activity, it can be dosed at up to 20-fold the therapeutic dose of low-molecular-weight heparin to optimize the antiadhesive effects, he noted.
However, the data indicate that “antiadhesive therapies are clearly not effective in patients with vaso-occlusive crisis,” he said, noting that this was also affirmed by a similar 2019 study of the investigational panselectin inhibitor rivipansel, as reported in a Pfizer press release.
Intriguingly, the difference between the current study and the 2007 study by Qari et al. raises questions about whether anticoagulation, rather than antiadhesion, helped resolve VOC in that study, he said, noting that future studies should focus on whether that is the case.
As for the role of antiadhesive therapy, the mode of action of sevuparin and the current findings taken together suggest that future studies should also assess whether it can be used to prevent VOC.
“Perhaps sevuparin could be administered to patients in a prodromal phase – just before a real vaso-occlusive crisis appears – to prevent such a crisis from happening,” he said. “It would be interesting to use the drug that way.”
Dr. Biemond reported research funding from Sanquin and honoraria from Novartis and GBT.
SOURCE: Biemond B et al. ASH 2019, Abstract 614.
ORLANDO – Sevuparin, a novel nonanticoagulant heparinoid drug, showed no efficacy for acute vaso-occlusive crisis (VOC) in patients with sickle cell disease (SCD) in the randomized, controlled, phase 2 TVOC01 trial, but its promising safety and broad mechanism of action warrant further exploration in the prodromal VOC setting, according to investigators.
Time to VOC resolution – the primary study endpoint – was similar at about 168 hours in 71 hospitalized patients randomized to receive sevuparin and in 76 who received placebo (intention-to-treat hazard ratio, 0.89), Bart J. Biemond, MD, explained during a presentation of the findings at the annual meeting of the American Society of Hematology.
A per-protocol analysis based on the 69 and 75 patients dosed in the treatment and placebo arms, respectively, showed a similar result (HR, 0.81), said Dr. Biemond of the department of clinical hematology, Amsterdam UMC, Academic Medical Center, the Netherlands.
Secondary endpoints, including mean change in pain intensity from baseline on a visual analogue scale (VAS), duration of severest pain measured as time to achieve a 30% reduction in VAS score from baseline, and cumulative use of parenteral opioids, also did not differ between the treatment and placebo arms, he added.
Patients in the global, double-blind, multicenter trial were aged 12-50 years (median, 22 years) with any type of SCD. They were enrolled from 16 sites in 7 countries to receive a loading dose of 3 mg/kg of sevuparin and continuous 18 mg/kg per day infusions or placebo. Patients in both arms also received standard-of-care and parenteral opioid therapy.
The groups were generally balanced with respect to demographic and baseline characteristics, Dr. Biemond said, noting that the treatment was safe: No serious adverse events occurred, and any mild-to-moderate adverse events were transient.
The findings were disappointing given the lack of approved treatment options other than pain management for acute VOC in hospitalized patients with SCD, and they were somewhat surprising given that preclinical and clinical data in recent years have demonstrated that “you can actually prevent those crises by antiadhesive strategies,” he said.
“So we hypothesized that, if you perform such an antiadhesive strategy in a patient already having a crisis and admitted in the hospital, you may shorten their period of admission and perhaps also shorten the severity of their pain,” he said.
In fact, a single-center, randomized, controlled trial conducted by Qari et al. in 2007 (Thromb Haemost. 2007 Aug;98[2]:392-6) showed that full-dose tinzaparin reduced pain severity and duration of admission among sickle cell patients with acute VOC – perhaps because of the antiadhesive properties of heparin – but that study was never repeated, Dr. Biemond said, noting that those antiadhesive properties have been well documented in animal studies.
“Heparin is able to inhibit P-selectin, L-selectin, thrombospondin, fibronectin, and von Willebrand activity, which are all involved in vaso-occlusion in patients with sickle cell disease, and very likely also involved during a vaso-occlusive crisis,” he explained, adding that sevuparin, a low-molecular-weight heparin without functional antithrombin binding domain, seemed to be a good candidate for testing that hypothesis.
“It has no anticoagulant effects on factor Xa and IIa,” he said. “It retains, however, its antiadhesive and antiaggregation properties.”
Since it has no anticoagulation activity, it can be dosed at up to 20-fold the therapeutic dose of low-molecular-weight heparin to optimize the antiadhesive effects, he noted.
However, the data indicate that “antiadhesive therapies are clearly not effective in patients with vaso-occlusive crisis,” he said, noting that this was also affirmed by a similar 2019 study of the investigational panselectin inhibitor rivipansel, as reported in a Pfizer press release.
Intriguingly, the difference between the current study and the 2007 study by Qari et al. raises questions about whether anticoagulation, rather than antiadhesion, helped resolve VOC in that study, he said, noting that future studies should focus on whether that is the case.
As for the role of antiadhesive therapy, the mode of action of sevuparin and the current findings taken together suggest that future studies should also assess whether it can be used to prevent VOC.
“Perhaps sevuparin could be administered to patients in a prodromal phase – just before a real vaso-occlusive crisis appears – to prevent such a crisis from happening,” he said. “It would be interesting to use the drug that way.”
Dr. Biemond reported research funding from Sanquin and honoraria from Novartis and GBT.
SOURCE: Biemond B et al. ASH 2019, Abstract 614.
ORLANDO – Sevuparin, a novel nonanticoagulant heparinoid drug, showed no efficacy for acute vaso-occlusive crisis (VOC) in patients with sickle cell disease (SCD) in the randomized, controlled, phase 2 TVOC01 trial, but its promising safety and broad mechanism of action warrant further exploration in the prodromal VOC setting, according to investigators.
Time to VOC resolution – the primary study endpoint – was similar at about 168 hours in 71 hospitalized patients randomized to receive sevuparin and in 76 who received placebo (intention-to-treat hazard ratio, 0.89), Bart J. Biemond, MD, explained during a presentation of the findings at the annual meeting of the American Society of Hematology.
A per-protocol analysis based on the 69 and 75 patients dosed in the treatment and placebo arms, respectively, showed a similar result (HR, 0.81), said Dr. Biemond of the department of clinical hematology, Amsterdam UMC, Academic Medical Center, the Netherlands.
Secondary endpoints, including mean change in pain intensity from baseline on a visual analogue scale (VAS), duration of severest pain measured as time to achieve a 30% reduction in VAS score from baseline, and cumulative use of parenteral opioids, also did not differ between the treatment and placebo arms, he added.
Patients in the global, double-blind, multicenter trial were aged 12-50 years (median, 22 years) with any type of SCD. They were enrolled from 16 sites in 7 countries to receive a loading dose of 3 mg/kg of sevuparin and continuous 18 mg/kg per day infusions or placebo. Patients in both arms also received standard-of-care and parenteral opioid therapy.
The groups were generally balanced with respect to demographic and baseline characteristics, Dr. Biemond said, noting that the treatment was safe: No serious adverse events occurred, and any mild-to-moderate adverse events were transient.
The findings were disappointing given the lack of approved treatment options other than pain management for acute VOC in hospitalized patients with SCD, and they were somewhat surprising given that preclinical and clinical data in recent years have demonstrated that “you can actually prevent those crises by antiadhesive strategies,” he said.
“So we hypothesized that, if you perform such an antiadhesive strategy in a patient already having a crisis and admitted in the hospital, you may shorten their period of admission and perhaps also shorten the severity of their pain,” he said.
In fact, a single-center, randomized, controlled trial conducted by Qari et al. in 2007 (Thromb Haemost. 2007 Aug;98[2]:392-6) showed that full-dose tinzaparin reduced pain severity and duration of admission among sickle cell patients with acute VOC – perhaps because of the antiadhesive properties of heparin – but that study was never repeated, Dr. Biemond said, noting that those antiadhesive properties have been well documented in animal studies.
“Heparin is able to inhibit P-selectin, L-selectin, thrombospondin, fibronectin, and von Willebrand activity, which are all involved in vaso-occlusion in patients with sickle cell disease, and very likely also involved during a vaso-occlusive crisis,” he explained, adding that sevuparin, a low-molecular-weight heparin without functional antithrombin binding domain, seemed to be a good candidate for testing that hypothesis.
“It has no anticoagulant effects on factor Xa and IIa,” he said. “It retains, however, its antiadhesive and antiaggregation properties.”
Since it has no anticoagulation activity, it can be dosed at up to 20-fold the therapeutic dose of low-molecular-weight heparin to optimize the antiadhesive effects, he noted.
However, the data indicate that “antiadhesive therapies are clearly not effective in patients with vaso-occlusive crisis,” he said, noting that this was also affirmed by a similar 2019 study of the investigational panselectin inhibitor rivipansel, as reported in a Pfizer press release.
Intriguingly, the difference between the current study and the 2007 study by Qari et al. raises questions about whether anticoagulation, rather than antiadhesion, helped resolve VOC in that study, he said, noting that future studies should focus on whether that is the case.
As for the role of antiadhesive therapy, the mode of action of sevuparin and the current findings taken together suggest that future studies should also assess whether it can be used to prevent VOC.
“Perhaps sevuparin could be administered to patients in a prodromal phase – just before a real vaso-occlusive crisis appears – to prevent such a crisis from happening,” he said. “It would be interesting to use the drug that way.”
Dr. Biemond reported research funding from Sanquin and honoraria from Novartis and GBT.
SOURCE: Biemond B et al. ASH 2019, Abstract 614.
REPORTING FROM ASH 2019
Are providers asking about menstrual bleeding before/during anticoagulant therapy?
ORLANDO – A small study suggests health care providers may fail to ask patients about heavy menstrual bleeding before or during treatment with oral anticoagulants.
Researchers performed a chart review at a single center, which indicated that 60% of women were not asked about heavy menstrual bleeding before they were prescribed an oral anticoagulant.
Six months after the women started anticoagulant therapy, 29% required treatment for heavy menstrual bleeding. Charts for the remaining 71% of women contained no information about heavy menstrual bleeding.
“We were unable to distinguish between true absence of heavy menstrual bleeding and absence of reporting,” said Bethany T. Samuelson Bannow, MD, of Oregon Health & Science University, Portland.
Dr. Samuelson Bannow presented these findings at the annual meeting of the American Society of Hematology.
She explained that heavy menstrual bleeding is defined as more than 80 mL of blood loss per cycle. It affects 10%-15% of women in their lifetime, and anticoagulants increase the risk of heavy menstrual bleeding.
Studies have shown that heavy menstrual bleeding occurs in 22%-65% of women treated with vitamin K agonists and 20%-27% of women treated with rivaroxaban (Blood. 2017;130[24]:2603-9). However, many anticoagulant studies don’t include heavy menstrual bleeding as an outcome.
To gain more insight, Dr. Samuelson Bannow and colleagues conducted a chart review. Their study included 236 women of reproductive age treated at Oregon Health & Science University between Jan. 1, 2012, and Dec. 31, 2018.
The patients’ median age was 37 years (range, 18-50 years). Most patients (67%) were receiving an oral anticoagulant for venous thromboembolism. The rest were on anticoagulant therapy for arterial thrombosis (6%), atrial fibrillation (6%), a mechanical valve (1%), or “other” reasons (20%).
Dr. Samuelson Bannow said the other group was “almost exclusively women who were receiving prophylaxis” postoperatively or for travel. Most women in this group were receiving rivaroxaban.
Rivaroxaban was the most commonly prescribed anticoagulant in the entire cohort (41%), followed by warfarin (34%) and apixaban (25%).
At the time of anticoagulant prescription, 12% of women reported a history of heavy menstrual bleeding, and 28% did not. For most patients – 60% – there was no discussion of menstrual history documented.
Six months after starting oral anticoagulant therapy, 29% of patients required treatment for heavy menstrual bleeding. For 71% of patients, there was no documentation on the treatment of heavy menstrual bleeding.
Treatment for heavy menstrual bleeding was required in 33% of patients on rivaroxaban, 24% of those on apixaban, and 29% of those on warfarin, a significant difference (P less than .001).
“Rates of heavy menstrual bleeding … are higher in rivaroxaban users,” Dr. Samuelson Bannow said. “This is not the first study to demonstrate this. However, [the rate of heavy menstrual bleeding in this study] is still a lot lower than we would expect based on past levels with warfarin. This tells us we’re probably missing a lot of heavy menstrual bleeding. That’s not too surprising considering how few providers are actually asking about the menses.”
Dr. Samuelson Bannow and colleagues disclosed no conflicts of interest.
SOURCE: Samuelson Bannow BT et al. ASH 2019, Abstract 60.
ORLANDO – A small study suggests health care providers may fail to ask patients about heavy menstrual bleeding before or during treatment with oral anticoagulants.
Researchers performed a chart review at a single center, which indicated that 60% of women were not asked about heavy menstrual bleeding before they were prescribed an oral anticoagulant.
Six months after the women started anticoagulant therapy, 29% required treatment for heavy menstrual bleeding. Charts for the remaining 71% of women contained no information about heavy menstrual bleeding.
“We were unable to distinguish between true absence of heavy menstrual bleeding and absence of reporting,” said Bethany T. Samuelson Bannow, MD, of Oregon Health & Science University, Portland.
Dr. Samuelson Bannow presented these findings at the annual meeting of the American Society of Hematology.
She explained that heavy menstrual bleeding is defined as more than 80 mL of blood loss per cycle. It affects 10%-15% of women in their lifetime, and anticoagulants increase the risk of heavy menstrual bleeding.
Studies have shown that heavy menstrual bleeding occurs in 22%-65% of women treated with vitamin K agonists and 20%-27% of women treated with rivaroxaban (Blood. 2017;130[24]:2603-9). However, many anticoagulant studies don’t include heavy menstrual bleeding as an outcome.
To gain more insight, Dr. Samuelson Bannow and colleagues conducted a chart review. Their study included 236 women of reproductive age treated at Oregon Health & Science University between Jan. 1, 2012, and Dec. 31, 2018.
The patients’ median age was 37 years (range, 18-50 years). Most patients (67%) were receiving an oral anticoagulant for venous thromboembolism. The rest were on anticoagulant therapy for arterial thrombosis (6%), atrial fibrillation (6%), a mechanical valve (1%), or “other” reasons (20%).
Dr. Samuelson Bannow said the other group was “almost exclusively women who were receiving prophylaxis” postoperatively or for travel. Most women in this group were receiving rivaroxaban.
Rivaroxaban was the most commonly prescribed anticoagulant in the entire cohort (41%), followed by warfarin (34%) and apixaban (25%).
At the time of anticoagulant prescription, 12% of women reported a history of heavy menstrual bleeding, and 28% did not. For most patients – 60% – there was no discussion of menstrual history documented.
Six months after starting oral anticoagulant therapy, 29% of patients required treatment for heavy menstrual bleeding. For 71% of patients, there was no documentation on the treatment of heavy menstrual bleeding.
Treatment for heavy menstrual bleeding was required in 33% of patients on rivaroxaban, 24% of those on apixaban, and 29% of those on warfarin, a significant difference (P less than .001).
“Rates of heavy menstrual bleeding … are higher in rivaroxaban users,” Dr. Samuelson Bannow said. “This is not the first study to demonstrate this. However, [the rate of heavy menstrual bleeding in this study] is still a lot lower than we would expect based on past levels with warfarin. This tells us we’re probably missing a lot of heavy menstrual bleeding. That’s not too surprising considering how few providers are actually asking about the menses.”
Dr. Samuelson Bannow and colleagues disclosed no conflicts of interest.
SOURCE: Samuelson Bannow BT et al. ASH 2019, Abstract 60.
ORLANDO – A small study suggests health care providers may fail to ask patients about heavy menstrual bleeding before or during treatment with oral anticoagulants.
Researchers performed a chart review at a single center, which indicated that 60% of women were not asked about heavy menstrual bleeding before they were prescribed an oral anticoagulant.
Six months after the women started anticoagulant therapy, 29% required treatment for heavy menstrual bleeding. Charts for the remaining 71% of women contained no information about heavy menstrual bleeding.
“We were unable to distinguish between true absence of heavy menstrual bleeding and absence of reporting,” said Bethany T. Samuelson Bannow, MD, of Oregon Health & Science University, Portland.
Dr. Samuelson Bannow presented these findings at the annual meeting of the American Society of Hematology.
She explained that heavy menstrual bleeding is defined as more than 80 mL of blood loss per cycle. It affects 10%-15% of women in their lifetime, and anticoagulants increase the risk of heavy menstrual bleeding.
Studies have shown that heavy menstrual bleeding occurs in 22%-65% of women treated with vitamin K agonists and 20%-27% of women treated with rivaroxaban (Blood. 2017;130[24]:2603-9). However, many anticoagulant studies don’t include heavy menstrual bleeding as an outcome.
To gain more insight, Dr. Samuelson Bannow and colleagues conducted a chart review. Their study included 236 women of reproductive age treated at Oregon Health & Science University between Jan. 1, 2012, and Dec. 31, 2018.
The patients’ median age was 37 years (range, 18-50 years). Most patients (67%) were receiving an oral anticoagulant for venous thromboembolism. The rest were on anticoagulant therapy for arterial thrombosis (6%), atrial fibrillation (6%), a mechanical valve (1%), or “other” reasons (20%).
Dr. Samuelson Bannow said the other group was “almost exclusively women who were receiving prophylaxis” postoperatively or for travel. Most women in this group were receiving rivaroxaban.
Rivaroxaban was the most commonly prescribed anticoagulant in the entire cohort (41%), followed by warfarin (34%) and apixaban (25%).
At the time of anticoagulant prescription, 12% of women reported a history of heavy menstrual bleeding, and 28% did not. For most patients – 60% – there was no discussion of menstrual history documented.
Six months after starting oral anticoagulant therapy, 29% of patients required treatment for heavy menstrual bleeding. For 71% of patients, there was no documentation on the treatment of heavy menstrual bleeding.
Treatment for heavy menstrual bleeding was required in 33% of patients on rivaroxaban, 24% of those on apixaban, and 29% of those on warfarin, a significant difference (P less than .001).
“Rates of heavy menstrual bleeding … are higher in rivaroxaban users,” Dr. Samuelson Bannow said. “This is not the first study to demonstrate this. However, [the rate of heavy menstrual bleeding in this study] is still a lot lower than we would expect based on past levels with warfarin. This tells us we’re probably missing a lot of heavy menstrual bleeding. That’s not too surprising considering how few providers are actually asking about the menses.”
Dr. Samuelson Bannow and colleagues disclosed no conflicts of interest.
SOURCE: Samuelson Bannow BT et al. ASH 2019, Abstract 60.
REPORTING FROM ASH 2019
UKALL14: Rituximab improves EFS in B-ALL, but four doses not enough
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
ORLANDO – Adding rituximab to standard induction chemotherapy in adults with precursor B-cell acute lymphoblastic leukemia (B-ALL) appears to improve event-free survival, but four doses are insufficient, according to the first analysis from the randomized, phase 3 UKALL14 trial.
The findings also suggest that the significant event-free survival (EFS) benefit of adding 16-18 doses of rituximab in B-ALL patients, as demonstrated in “the recent and very important” GRAALL-2005/R study, may be generalizable to B-precursor ALL patients regardless of Philadelphia (Ph) chromosome status or CD20-positive expression level, Adele K. Fielding, MBBS, PhD, reported at the annual meeting of the American Society of Hematology.
Unlike GRAALL-2005/R (NCT00327678), which included only patients with greater than 20% of ALL blasts expressing CD20 and with Ph-negative ALL, UKALL14 (NCT01085617) included B-ALL patients regardless of Ph chromosome status or CD20 expression level, explained Dr. Fielding of the Cancer Institute, University College London.
Overall, EFS rates among patients in the UKALL14 study at a median follow-up of 40.5 months were 41.9% in 288 patients randomized to receive standard-of-care chemotherapy (SOC), and 48.7% among 289 randomized to receive SOC plus rituximab, but the difference was not statistically significant (hazard ratio, 0.88; P = .28), she said.
“Likewise there was a nonsignificant improvement in 3-year event-free survival and in median event-free survival in the rituximab arms, but these differences did not meet our predetermined criteria,” she added.
Similarly, the overall survival findings showed slight, but non–statistically significant improvement in the rituximab arms (HR, 0.9; P = .39). The 3-year and median overall survival outcomes appeared to favor rituximab, but “this was not the magnitude of benefit that we were seeking in our study,” she said.
However, while a preplanned subgroup analysis by cytogenetic and other risk groups, as well as by cell surface CD20 expression, did not reveal any significant interactions for EFS, they did show that the percentage of blasts expressing CD20 was a strong independent poor prognostic factor.
A cutoff of 11.6%, compared with the 20% typically used, was found to be ideal based on the Youden Index, which determines the best balance between sensitivity and specificity.
“Interestingly, in addition to this, we did not find any impact of CD20 expression on response to rituximab,” Dr. Fielding noted.
Further, outcomes analyses by post–induction treatment assignment showed that, in patients who received myeloablative allogeneic stem cell transplant, “there was a large and statistically significant benefit to [adding rituximab], she said.
Landmark analysis showed an EFS hazard ratio of 0.48 at the time of transplant (P = .037), she said, noting that the SOC and SOC plus rituximab arms were well matched among this subset of patients.
The difference appeared to relate to relapse risk (HR, .38), but on an intention-to-treat analysis including all patients under age 40 years, the difference was “no longer quite so pronounced.”
“We do not understand the biological basis for this finding,” Dr. Fielding said, noting that it wasn’t explained by differences in graft-versus-host disease or infection. “This difference was not apparent in patients who received or were intended to receive reduced-intensity allogeneic conditioning.”
A multivariable analysis did not show a significant treatment effect, but did show “the same trend toward a better outcome in the rituximab arm,” she added.
UKALL14 subjects were adults aged 25-65 years with de novo ALL, regardless of Ph status or cell surface CD20 expression, who were recruited from 70 centers in the United Kingdom between December 2010 and July 2017. Those randomized to standard of care received a standard four-drug induction after a steroid prephase – with or without four doses of rituximab.
After a second induction, patients underwent risk assessment; low-risk patients were treated on the SOC arm and received high-dose methotrexate and additional pegylated asparaginase followed by four cycles of consolidation therapy. This was followed by 2 years of maintenance treatment.
High-risk patients with a sibling or fully matched unrelated donor available underwent allogeneic stem cell transplant, with those aged 40 years and younger receiving myeloablative conditioning and those over 40 years receiving reduced-intensity conditioning.
Most patients in the SOC plus rituximab arm received all four doses of rituximab, and the treatment arms were well-balanced with respect to risk characteristics, Dr. Fielding said, adding that no differences were noted in adverse events or mortality between the arms.
There is strong rationale for studying rituximab in ALL, she noted. For example, rituximab is safe to add to chemotherapy, and it has potential relevance at any level of CD20 expression, she said, explaining the basis for the study. Indeed, the findings support its use in this setting.
“Rituximab benefits patients with ALL,” she said. “But in our hands, four doses is insufficient to realize the full benefit.”
Dr. Fielding is a consultant for Amgen, Novartis, Pfizer, and Incyte.
SOURCE: Marks D et al. ASH 2019, Abstract 739.
REPORTING FROM ASH 2019
Promising early efficacy of venetoclax/navitoclax in r/r acute lymphoblastic leukemia
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
ORLANDO – A combination of venetoclax (Venclexta) and the experimental BCL-2 inhibitor navitoclax showed good activity and acceptable safety in both children and adults with relapsed or refractory acute lymphoblastic leukemia or lymphoblastic lymphoma, investigators in a phase 1 trial reported.
The overall rate of combined complete response (CR), CR with incomplete marrow recovery (CRi) or incomplete platelet recovery (CRp) was 49% among 45 patients: 24 with acute lymphoblastic leukemia of B-cell lineage (B-ALL), 18 with T-cell lineage ALL (T-ALL), and 3 with lymphoblastic lymphoma, reported Norman J. Lacayo, MD, from Stanford (Calif.) University.
“Venetoclax, navitoclax, and chemotherapy is well tolerated with few discontinuations for dose reductions due to adverse events in patients with relapsed/refractory ALL or lymphoblastic lymphoma. The preliminary efficacy was promising in this heavily pretreated population of patients, including pediatric patients and patients with prior stem cell transplantation of CAR [chimeric antigen receptor] T-cell therapy,” he said at the annual meeting of the American Society of Hematology.
Venetoclax is a highly selective inhibitor of the B-cell lymphoma 2 (BCL-2) pathway. Navitoclax inhibits BCL-2, the BCL–extra large (BCL-XL) transmembrane molecule, and the apoptotic protein BCL-W, but was associated with dose-limiting toxicities when used at standard doses in monotherapy, he noted.
To see whether adding venetoclax to low-dose navitoclax could be safe and have synergistic activity against BCL-2, Dr. Lacayo and colleagues are conducting a phase 1, open-label, dose-escalation study of patients aged 4 years and older with relapsed/refractory ALL or lymphoblastic lymphoma.
Patients receive the weight-adjusted equivalent of 200 mg venetoclax on day 1, and 400 mg equivalent daily thereafter. Beginning on day 3, patients receive oral navitoclax daily at doses of 25, 50, or 100 mg for patients weighing 45 kg or more, or 25 or 50 mg for patients weighing from 20 to less than 45 kg.
Patients can also receive two cycles of chemotherapy with asparaginase, vincristine, and dexamethasone, with additional cycles allowed at the investigators’ discretion.
The patients reported on at ASH 2019 had received a median of 4 prior lines of therapy (range, 1-10).
After a median time on study of 8 months, preliminary efficacy – a secondary endpoint of this phase 1 trial – was promising, Dr. Lacayo said. The CR rate was 25% among patients with B-ALL, 11% in patients with T-ALL, and 67% (two of three patients) with lymphoblastic lymphoma. The respective CRi rates were 13%, 17%, and 0%, and respective CRp rates were 17%, 11%, and 0%.
In addition, 3 of 24 patients (13%) with B-ALL had a partial response, as did 1 patient with lymphoblastic lymphoma.
The median time to first response was about 1.1 months. The median duration of response was 9.1 months for patients with B-ALL, 4.2 months for patients with T-ALL, and had not been reached among patients with lymphoblastic leukemia.
The median overall survival was 9.7 months for patients with B-ALL, 6.8 months for those with T-ALL, and not reached for those with lymphoblastic leukemia.
In all, 6 of 24 patients with B-ALL, 3 of 18 with T-ALL, and 2 of 3 with lymphoblastic leukemia survived long enough to proceed to stem cell transplantation or CAR T-cell therapy.
Analysis of the combination’s safety, the primary endpoint, showed that 58% of patients had grade 3-4 adverse events (AEs) related to venetoclax, and 42% had grade 3-4 AEs related to navitoclax. Four patients had to discontinue the combination because of treatment-related AEs.
Dose-limiting toxicities, which occurred in seven patients, included delayed count recovery, drug-induced liver injury, intestinal ischemia, and increase in serum bilirubin.
One patient died from an intestinal ischemic event deemed to be related to the combination, and seven other patients had fatal adverse events considered not related to the study drugs. The causes of death included sepsis, septic shock, cardiac arrest, and neurotoxicity.
The investigators are enrolling an expansion cohort to see whether a 21-day dosing schedule of venetoclax with 50 mg navitoclax, or 25 mg for patients under 45 kg, could improve count recovery time.
The study was funded by AbbVie. Dr. Lacayo reported having no conflict of interests to disclose. Several coauthors are AbbVie employees.
SOURCE: Lacayo NJ et al. ASH 2019, Abstract 285.
REPORTING FROM ASH 2019
REGN1979 shows good activity in pretreated aggressive B-NHL
ORLANDO – A novel bispecific antibody directed against CD20 and CD3 was associated in a phase 1 trial with a high overall response rate among patients with relapsed or refractory B-cell non-Hodgkin lymphomas in early clinical trials, including patients with diffuse large B-cell lymphoma (DLBCL) that had progressed following chimeric antigen receptor (CAR) T-cell therapy.
Among 22 patients previously treated for relapsed/refractory follicular lymphoma of grade 1-3a, there were 21 responses (95%), including 17 complete responses (CR) and 4 partial responses (PR), with the remaining patient having stable disease at 12 weeks of follow-up, reported Rajat Bannerji, MD, PhD, from the Rutgers Cancer Institute of New Jersey in New Brunswick.
“We had activity that was fairly robust in this heavily pretreated population with follicular lymphoma, large-cell patients who had not received CAR T and large-cell patients who had received CAR T, mantle cell, and marginal zone [lymphoma],” he said at the annual meeting of the American Society of Hematology.
REGN1979 is an anti-CD20 and anti-CD3 bispecific IgG4 antibody. It is designed to cross-link and activate CD3-expressing T cells on contact with CD20-positive B cells to kill CD20-positive tumor cells independent of T-cell receptor recognition.
The antibody is administered via an escalating dose schedule consisting of initial, intermediate, and step-up doses.
In addition to the follicular lymphoma response rates noted before, patients with heavily pretreated DLBCL who received the antibody at a dose of 80 mg or higher had an overall response rate of 57.9% (11 patients) including 42.1% CR (8 patients), and 15.8% PR (3 patients). Two patients had stable disease at the 12-week assessment, three had disease progression, and three were not available for assessment.
Among seven patients with DLBCL treated at 80 mg or above who had not received CAR T therapy, five had a CR, one had stable disease, and one had disease progression. Of 12 patients with prior CAR T exposure, 3 had complete responses, 3 had partial responses, 1 had stable disease, 2 had progressive disease, and 3 were not available for assessment.
Among six patients with mantle cell lymphoma and six with marginal zone lymphoma treated across all disease levels, the ORR in each cohort was 67%, with two of six patients in each cohort having a complete response, and two having a partial response.
The safety analysis of all 110 patients enrolled showed that no patients experience a dose-limiting toxicity during the escalation phase, and no maximum tolerated doses were identified.
The most common treatment-related adverse events (AEs) were pyrexia in 88 patients, cytokine release syndrome in 65, chills in 56, fatigue in 40, and anemia in 39.
The most common grade 3-4 AEs were anemia in 24, and hypophosphatemia, lymphopenia, and neutropenia in 21 patients each.
Neurologic AEs were transient and did not require treatment discontinuation, and there were no grade 4 neurologic AEs or deaths from neurologic side effects.
Six patients discontinued the study drug because of treatment-related AEs that included cytomegalovirus infection, grade 3 hemolysis, fatigue, pneumonia, and toxoplasmosis.
A total of 15 patients died during the study, 10 of which were caused by progressive disease, with other deaths caused by gastric perforation, cardiac arrest, lung infection, pneumonia, and 1 from fungal pneumonia 7 months after treatment discontinuation. In addition, after the data cutoff, one patient with mantle cell lymphoma blastoid variant with bone-marrow involvement and bulky disease who was enrolled in an expansion cohort died from tumor lysis syndrome.
The dose-escalation portion of the trial has been completed and expansion cohorts are being enrolled. In addition, REGN1979 is being investigated in a phase 2 global multiarm trial.
The study is supported by Regeneron Pharmaceuticals. Dr. Bannerji reported research funding, travel support, and consulting fees from Regeneron and others.
SOURCE: Bannerji R et al. ASH 2019, Abstract 762.
ORLANDO – A novel bispecific antibody directed against CD20 and CD3 was associated in a phase 1 trial with a high overall response rate among patients with relapsed or refractory B-cell non-Hodgkin lymphomas in early clinical trials, including patients with diffuse large B-cell lymphoma (DLBCL) that had progressed following chimeric antigen receptor (CAR) T-cell therapy.
Among 22 patients previously treated for relapsed/refractory follicular lymphoma of grade 1-3a, there were 21 responses (95%), including 17 complete responses (CR) and 4 partial responses (PR), with the remaining patient having stable disease at 12 weeks of follow-up, reported Rajat Bannerji, MD, PhD, from the Rutgers Cancer Institute of New Jersey in New Brunswick.
“We had activity that was fairly robust in this heavily pretreated population with follicular lymphoma, large-cell patients who had not received CAR T and large-cell patients who had received CAR T, mantle cell, and marginal zone [lymphoma],” he said at the annual meeting of the American Society of Hematology.
REGN1979 is an anti-CD20 and anti-CD3 bispecific IgG4 antibody. It is designed to cross-link and activate CD3-expressing T cells on contact with CD20-positive B cells to kill CD20-positive tumor cells independent of T-cell receptor recognition.
The antibody is administered via an escalating dose schedule consisting of initial, intermediate, and step-up doses.
In addition to the follicular lymphoma response rates noted before, patients with heavily pretreated DLBCL who received the antibody at a dose of 80 mg or higher had an overall response rate of 57.9% (11 patients) including 42.1% CR (8 patients), and 15.8% PR (3 patients). Two patients had stable disease at the 12-week assessment, three had disease progression, and three were not available for assessment.
Among seven patients with DLBCL treated at 80 mg or above who had not received CAR T therapy, five had a CR, one had stable disease, and one had disease progression. Of 12 patients with prior CAR T exposure, 3 had complete responses, 3 had partial responses, 1 had stable disease, 2 had progressive disease, and 3 were not available for assessment.
Among six patients with mantle cell lymphoma and six with marginal zone lymphoma treated across all disease levels, the ORR in each cohort was 67%, with two of six patients in each cohort having a complete response, and two having a partial response.
The safety analysis of all 110 patients enrolled showed that no patients experience a dose-limiting toxicity during the escalation phase, and no maximum tolerated doses were identified.
The most common treatment-related adverse events (AEs) were pyrexia in 88 patients, cytokine release syndrome in 65, chills in 56, fatigue in 40, and anemia in 39.
The most common grade 3-4 AEs were anemia in 24, and hypophosphatemia, lymphopenia, and neutropenia in 21 patients each.
Neurologic AEs were transient and did not require treatment discontinuation, and there were no grade 4 neurologic AEs or deaths from neurologic side effects.
Six patients discontinued the study drug because of treatment-related AEs that included cytomegalovirus infection, grade 3 hemolysis, fatigue, pneumonia, and toxoplasmosis.
A total of 15 patients died during the study, 10 of which were caused by progressive disease, with other deaths caused by gastric perforation, cardiac arrest, lung infection, pneumonia, and 1 from fungal pneumonia 7 months after treatment discontinuation. In addition, after the data cutoff, one patient with mantle cell lymphoma blastoid variant with bone-marrow involvement and bulky disease who was enrolled in an expansion cohort died from tumor lysis syndrome.
The dose-escalation portion of the trial has been completed and expansion cohorts are being enrolled. In addition, REGN1979 is being investigated in a phase 2 global multiarm trial.
The study is supported by Regeneron Pharmaceuticals. Dr. Bannerji reported research funding, travel support, and consulting fees from Regeneron and others.
SOURCE: Bannerji R et al. ASH 2019, Abstract 762.
ORLANDO – A novel bispecific antibody directed against CD20 and CD3 was associated in a phase 1 trial with a high overall response rate among patients with relapsed or refractory B-cell non-Hodgkin lymphomas in early clinical trials, including patients with diffuse large B-cell lymphoma (DLBCL) that had progressed following chimeric antigen receptor (CAR) T-cell therapy.
Among 22 patients previously treated for relapsed/refractory follicular lymphoma of grade 1-3a, there were 21 responses (95%), including 17 complete responses (CR) and 4 partial responses (PR), with the remaining patient having stable disease at 12 weeks of follow-up, reported Rajat Bannerji, MD, PhD, from the Rutgers Cancer Institute of New Jersey in New Brunswick.
“We had activity that was fairly robust in this heavily pretreated population with follicular lymphoma, large-cell patients who had not received CAR T and large-cell patients who had received CAR T, mantle cell, and marginal zone [lymphoma],” he said at the annual meeting of the American Society of Hematology.
REGN1979 is an anti-CD20 and anti-CD3 bispecific IgG4 antibody. It is designed to cross-link and activate CD3-expressing T cells on contact with CD20-positive B cells to kill CD20-positive tumor cells independent of T-cell receptor recognition.
The antibody is administered via an escalating dose schedule consisting of initial, intermediate, and step-up doses.
In addition to the follicular lymphoma response rates noted before, patients with heavily pretreated DLBCL who received the antibody at a dose of 80 mg or higher had an overall response rate of 57.9% (11 patients) including 42.1% CR (8 patients), and 15.8% PR (3 patients). Two patients had stable disease at the 12-week assessment, three had disease progression, and three were not available for assessment.
Among seven patients with DLBCL treated at 80 mg or above who had not received CAR T therapy, five had a CR, one had stable disease, and one had disease progression. Of 12 patients with prior CAR T exposure, 3 had complete responses, 3 had partial responses, 1 had stable disease, 2 had progressive disease, and 3 were not available for assessment.
Among six patients with mantle cell lymphoma and six with marginal zone lymphoma treated across all disease levels, the ORR in each cohort was 67%, with two of six patients in each cohort having a complete response, and two having a partial response.
The safety analysis of all 110 patients enrolled showed that no patients experience a dose-limiting toxicity during the escalation phase, and no maximum tolerated doses were identified.
The most common treatment-related adverse events (AEs) were pyrexia in 88 patients, cytokine release syndrome in 65, chills in 56, fatigue in 40, and anemia in 39.
The most common grade 3-4 AEs were anemia in 24, and hypophosphatemia, lymphopenia, and neutropenia in 21 patients each.
Neurologic AEs were transient and did not require treatment discontinuation, and there were no grade 4 neurologic AEs or deaths from neurologic side effects.
Six patients discontinued the study drug because of treatment-related AEs that included cytomegalovirus infection, grade 3 hemolysis, fatigue, pneumonia, and toxoplasmosis.
A total of 15 patients died during the study, 10 of which were caused by progressive disease, with other deaths caused by gastric perforation, cardiac arrest, lung infection, pneumonia, and 1 from fungal pneumonia 7 months after treatment discontinuation. In addition, after the data cutoff, one patient with mantle cell lymphoma blastoid variant with bone-marrow involvement and bulky disease who was enrolled in an expansion cohort died from tumor lysis syndrome.
The dose-escalation portion of the trial has been completed and expansion cohorts are being enrolled. In addition, REGN1979 is being investigated in a phase 2 global multiarm trial.
The study is supported by Regeneron Pharmaceuticals. Dr. Bannerji reported research funding, travel support, and consulting fees from Regeneron and others.
SOURCE: Bannerji R et al. ASH 2019, Abstract 762.
REPORTING FROM ASH 2019
Chemo-free induction-consolidation protocol for Ph+ ALL improved survival
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
ORLANDO – A front-line chemotherapy-free induction-consolidation protocol that combines dasatinib and blinatumomab for the treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) resulted in high survival and molecular response rates in the phase 2 D-ALBA trial.
At a median follow-up of 14.3 months, 61 of 63 patients enrolled in the multicenter trial had completed induction with the second-generation tyrosine kinase inhibitor (TKI) dasatinib, 60 had received the first cycle of treatment with the bispecific monoclonal antibody blinatumomab, and 56, 45, 36, and 25 had received second, third, fourth, and fifth cycles of blinatumomab, respectively, Sabina Chiaretti, MD, PhD, reported at the annual meeting of the American Society of Hematology.
The molecular response rate at the end of induction on day 85 was 29%, said Dr. Chiaretti of the department of translational and precision medicine, Sapienza University, Rome.
“Even more importantly, at the primary endpoint [the end of the second cycle of blinatumomab], 60% of patients were molecular responders,” she said.
Of note, the molecular response rate continued to increase with additional blinatumomab cycles; the rate was 79% after cycle 4, she said.
The overall survival (OS) and disease-free survival (DFS) rates also were “very exciting and promising” at 92.5% and 89.7%, respectively, she added.
DFS did not differ significantly based on molecular response at day 85 (100% vs. 87.4% in those with vs. without a molecular response; P = .154), but patients with p190 fusion protein had slightly worse DFS, compared with those who had p210 or both p190 and p210 fusion protein (83.5% vs. 100%; P = .48).
Study participants included adult Ph+ ALL patients with a median age of 54.5 years (range of 24.1-81.7 years) who were enrolled between May 2017 and January 2019; 54% were women and the median white blood cell count was 42 x109/L.
The percentage of study subjects with the p190, p210, and both p190/p210 fusion proteins was 65.1%, 27%, and 7.9% respectively, Dr. Chiaretti said.
Treatment included dasatinib at a dose of 140 mg/day as induction for 85 days along with steroids, which were started 7 days prior to induction and continued for a total of 31 days. Those who had a complete hematologic response (CHR) after induction received postinduction consolidation treatment with blinatumomab at a flat dose of 28 mcg/day for at least 2 cycles, and up to 3 additional cycles were allowed at physician discretion based on molecular response.
During the course of the study, 156 adverse events occurred, including 50 serious adverse events. The latter most often involved infections, including 6 cytomegalovirus infections and 6 cases of prolonged fever; one of those cases was likely related to blinatumomab.
Two patients died, including an 80-year-old woman who died during induction, and a patient who was in CHR. Six relapses occurred, including one that involved a major protocol violation; three were extramedullary.
Additional analyses in this study showed that the most frequent copy number aberration was, as expected based on the available literature, IKZF1 deletion, which was present in 25 of 46 available samples (54%). Of those, 11 (23.9%) were found to have the IKZF1-plus signature, defined as IKZF1 and/or PAX5 and/or CDKN2A/B deletions, she said.
Further, ABL1 mutational analysis conducted in 15 patients with evidence of MRD increase showed that 8 were wild type and 7 were mutated – with 6 of the 7 represented by the gatekeeper mutation T315I, and one by an E255K mutation. All but 1 mutation occurred in p190 cases prior to the start of blinatumomab.
Of note, and in line with prior findings, blinatumomab was effective for reducing or eradicating the MRD levels in these difficult-to-treat patients, Dr. Chiaretti said.
An analysis of the immunologic compartment carried out in 12 patients who completed all 5 cycles of blinatumomab showed a significant increase in the rate of CD8+ T cells (29% vs. 19.8% before the start of blinatumomab; P = .04) and a significant reduction in the rate of Tregs (3.7% vs. 11% before blinatumomab; P = .02), she added.
The findings of this study to date – with some patients having more than 2 years of follow-up – are notable given the high rates of molecular response and survival, Dr. Chiaretti said.
Outcomes in patients with Ph+ ALL were generally poor before the introduction of TKIs, but “the scenario completely changed,” she explained.
“In general, all TKI-based treatments – with or without chemotherapy – have led to overall survival rates in the range of 50% ... which means that we still need to improve our clinical management,” she said. “Another finding that became clear is the fact that patients who achieve MRD-negative status have a significantly better outcome than those who do not.”
The D-ALBA trial was designed with the aim of increasing the rate of MRD negativity in newly diagnosed patients using dasatinib and blinatumomab, and the results demonstrate that this chemotherapy-free induction/consolidation approach is feasible in the front-line setting for adult Ph+ ALL patients, she said, adding that “it is strongly effective in inducing high rates of MRD negativity, and it results in much better survival rates.”
The findings with respect to IKZF1-plus cases and ABL1 mutations underscore the need for further work, she said.
“We still have to face some challenging cases,” she explained. “This study, as others before, really proves that IKZF1-plus cases are very difficult to treat; they require intensification and probably alternative strategies.”
Dr. Chiaretti reported membership on a board of directors or advisory committee for Pfizer, Incyte, Amgen, and Shire.
SOURCE: Chiaretti S et al. ASH 2019, Abstract 740.
REPORTING FROM ASH 2019