User login
Imaging Combo May Diagnose Gastric Cancer Without Biopsy
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
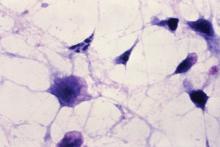
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: Magnifying NBI improves the diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions. The diagnostic accuracy of white light endoscopy alone was 65%, whereas that of magnifying NBI alone was 90%, a statistically significant difference (P less than .001).
Data Source: A multicenter, prospective, randomized, controlled trial of 362 patients with small depressed gastric lesions.
Disclosures: The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
Imaging Combo May Diagnose Gastric Cancer Without Biopsy
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: Magnifying NBI improves the diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions. The diagnostic accuracy of white light endoscopy alone was 65%, whereas that of magnifying NBI alone was 90%, a statistically significant difference (P less than .001).
Data Source: A multicenter, prospective, randomized, controlled trial of 362 patients with small depressed gastric lesions.
Disclosures: The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
Imaging Combo May Diagnose Gastric Cancer Without Biopsy
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
CHICAGO – The combination of white light endoscopy and magnifying narrow-band imaging shows promise for achieving accurate diagnosis of early gastric cancer, based on a prospective, randomized, controlled trial conducted in Japan.
"Magnifying narrow-band imaging improved [the] diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions," said Dr. Noriya Uedo, the principal investigator. "Adding magnifying narrow-band imaging to white light endoscopy could make accurate diagnosis of early gastric cancer [possible] without biopsy."
Currently, a diagnosis is made primarily via biopsy, said Dr. Uedo at the annual Digestive Disease Week.
Narrow-band imaging (NBI) is a novel optical technology for examining the surface structure and vascular architecture in the superficial mucosa. "Using magnifying endoscopy, it enables us to evaluate detailed morphological features of both epithelium and vasculature corresponding to histology," he said.
This study was designed to compare the real-time diagnostic performance of conventional white light endoscopy vs. magnifying NBI for gastric lesions no larger than 1 cm.
The trial included patients with a history of endoscopic treatment of early gastric cancer who were at high risk for developing recurrent gastric cancer. The study’s primary objective was to contrast the diagnostic accuracy of the two modalities.
On enrollment, patients were screened with white light endoscopy, and those who were found to have a previously undiagnosed small depressed lesion were randomized to either the white light group or the magnifying NBI group. In the white light group, after the endoscopic finding was documented, the lesion was then evaluated with magnifying NBI.
Between June 2008 and May 2010, 1,365 patients were enrolled, and 362 were found to have small depressed lesions. These patients were randomized to the white light endoscopy group or the magnifying narrow-band imaging group. There were 20 patients with gastric carcinoma in each group.
The diagnostic accuracy of white light endoscopy was 65% (114 of 176), whereas that of magnifying NBI was 90% (160 of 177), and this difference was statistically significant (P less than .001). Sensitivity was also higher in the magnifying NBI group at 60% (12 of 20) vs. 40% (8 of 20), but this difference did not reach statistical significance. Specificity was significantly higher in the magnifying NBI group at 94% (148 of 157), compared with the white light endoscopy group at 68% (106 of 156; P less than .001).
The time required to make a diagnosis with magnifying NBI was about 30 seconds longer than with white light endoscopy. "The difference would be acceptable in a clinical setting, instead of taking a biopsy, I think," said Dr. Uedo of the department of gastrointestinal oncology, Osaka (Japan) Medical Center for Cancer and Cardiovascular Diseases.
The diagnostic performance of magnifying NBI following white light imaging, compared with white light imaging alone, was significantly better in terms of accuracy, sensitivity, and specificity (P less than .001 in each case).
Dr. Uedo said that the specificity of white light endoscopy was not very high, and the number of false-positive lesions was large. "So, the number of biopsies is also large," he said. Only 40% of carcinomas were correctly diagnosed based on their endoscopic appearance. However, he said, the number of false-positive lesions in the magnifying NBI group was small, because of the higher specificity, and in turn the number of biopsies was lower.
As for the combination of the two modalities, he said that it "shows extremely excellent performance for differentiation of carcinoma from [a] benign depressed lesion."
Gastric cancer is the second leading cause of cancer death worldwide, and the earlier the diagnosis, the better the patient’s prognosis.
The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: Magnifying NBI improves the diagnostic performance of white light endoscopy for discriminating gastric cancer from benign small depressed lesions. The diagnostic accuracy of white light endoscopy alone was 65%, whereas that of magnifying NBI alone was 90%, a statistically significant difference (P less than .001).
Data Source: A multicenter, prospective, randomized, controlled trial of 362 patients with small depressed gastric lesions.
Disclosures: The study was funded by a grant-in-aid for cancer research from the Ministry of Health, Labor, and Welfare of Japan. Dr. Uedo does not have any relevant financial or other relationship with any manufacturer or provider of commercial products or services discussed during the presentation.
Link Between PPIs and C. difficile Inconsistent
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: In an adjusted Cox proportional hazard model, the association between proton pump inhibitor use and C. difficile infection was significant for patients on PPIs for 3 months, but less than 1 year, (hazard ratio, 1.94), but not for those on PPIs for at least 1 year (HR, 1.22).
Data Source: Longitudinal hospital cohort study of 61,834 patients treated at Seoul (South Korea) National University Hospital.
Disclosures: Dr. Hong and his colleagues reported no conflicts of interest.
Link Between PPIs and C. difficile Inconsistent
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Link Between PPIs and C. difficile Inconsistent
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: In an adjusted Cox proportional hazard model, the association between proton pump inhibitor use and C. difficile infection was significant for patients on PPIs for 3 months, but less than 1 year, (hazard ratio, 1.94), but not for those on PPIs for at least 1 year (HR, 1.22).
Data Source: Longitudinal hospital cohort study of 61,834 patients treated at Seoul (South Korea) National University Hospital.
Disclosures: Dr. Hong and his colleagues reported no conflicts of interest.
Adalimumab Appears Safe for Inducing Remission in Pediatric Crohn's
CHICAGO – Adalimumab induced and maintained clinical remission in children with moderate to severe Crohn’s disease and the treatment was not associated with any new safety signals in a double-blind, phase III, randomized trial.
The effect was most apparent in patients who were infliximab naive, Dr. Jeffrey S. Hyams said at the annual Digestive Disease Week.
Adalimumab (Humira), a human monoclonal antibody to tumor necrosis factor (TNF)–alfa, is indicated for the treatment of a variety of conditions including Crohn’s disease in adults and juvenile idiopathic arthritis, but it is not approved for juvenile Crohn’s disease.
The study involved 188 patients, aged 6-17 years, with moderate to severe Crohn’s disease that had lasted for at least 12 weeks, despite concurrent treatment with oral corticosteroids for at least 2 weeks and/or immunomodulators for at least 8 weeks. Roughly 45% of patients had used the chimeric monoclonal antibody to TNF, infliximab (Remicade).
All study patients received 4 weeks of open-label adalimumab induction therapy and were stratified based on response at week 4 and prior infliximab use to high- or low-dose maintenance adalimumab. High-dose adalimumab was 40 mg every other week for patients weighing 40 kg or more and 20 mg every other week if less than 40 kg. Low-dose adalimumab was 20 mg every other week for patients weighing 40 kg or more and 10 mg every other week if less than 40 kg. Dose escalation was allowed for flare or non-response beginning at week 12.
At week 26, 39% of the high-dose patients and 28% of low-dose patients met the study’s primary end point of clinical remission, defined as a Pediatric Crohn’s Disease Activity Index of 10 or less, said Dr. Hyams, director of the gastroenterology department at Connecticut Children’s Medical Center in Hartford. In addition, more high-dose patients than low-dose patients achieved clinical remission at week 52 (33% vs. 23%). The difference between groups was not statistically significant at week 26 or week 52.
A clinical response, defined as a decrease in Pediatric Crohn’s Disease Activity Index of at least 15 points from baseline, was observed in more high-dose than low-dose patients at week 26 (59% vs. 48%) and week 52, with the difference reaching statistical significance only at week 52 (42% vs. 28%; P = .03), he said.
When the data were broken down according to prior infliximab use, remission rates among infliximab-experienced patients were similar between the high- and low-dose adalimumab arms at week 26 (17% vs. 20%) and week 52 (19% vs. 17%).
Among infliximab-naive patients, however, clinical remission rates were significantly greater at week 26 in the high-dose vs. low-dose group (57% vs. 35%, P = .026), especially among week-4 responders (63% for high-dose group vs. 38% for low-dose group, P = .016). In all, 82% of the 188 patients responded to induction at week 4. Remission rates among infliximab-naive patients were statistically similar at week 52 (45% vs. 28%, P = .065).
Dr. Hyams said there were no "obvious safety signals" among patients who received at least one maintenance dose of adalimumab. Serious adverse events were reported in 19 (20%) of the 95 low-dose patients and 22 (24%) of the 93 high-dose patients. Notably, serious infections were reported in only 3 low-dose (3.2%) and 5 high-dose (5.4%) patients. No malignancies were observed.
Adalimumab carries a boxed warning for an increased risk of serious infections leading to hospitalization or death, particularly tuberculosis. In August 2009, the Food and Drug Administration also required that boxed warnings be added to the TNF-blocker class of drugs because of an increased risk of lymphoma and other malignancies in children and adolescents.
When asked during a discussion of the study about the effect of adalimumab on fistulas, Dr. Hyams said that 15%-20% of patients had active fistulas,and a beneficial response to therapy occurred in about 50% of the low-dose patients and about 80% of the high-dose patients.
Another attendee asked if prior treatment with immunomodulators affected response, and Dr. Hyams said it did not. If the patient experienced a clinical response, corticosteroid therapy was tapered after week 4 and could be increased to the baseline dose for flare or nonresponse. Immunomodulator therapy could be discontinued at or after week 26 and could not be reinstated.
The study was sponsored by Abbott Laboratories and an Abbott employee prepared the first draft and assisted in the production of the slides. Dr. Hyams disclosed consulting and advisory committee/review panel participation and grant/research support from Abbott. Five of the 13 coauthors are Abbott employees and five others have financial relationships with Abbott.
Humira,
CHICAGO – Adalimumab induced and maintained clinical remission in children with moderate to severe Crohn’s disease and the treatment was not associated with any new safety signals in a double-blind, phase III, randomized trial.
The effect was most apparent in patients who were infliximab naive, Dr. Jeffrey S. Hyams said at the annual Digestive Disease Week.
Adalimumab (Humira), a human monoclonal antibody to tumor necrosis factor (TNF)–alfa, is indicated for the treatment of a variety of conditions including Crohn’s disease in adults and juvenile idiopathic arthritis, but it is not approved for juvenile Crohn’s disease.
The study involved 188 patients, aged 6-17 years, with moderate to severe Crohn’s disease that had lasted for at least 12 weeks, despite concurrent treatment with oral corticosteroids for at least 2 weeks and/or immunomodulators for at least 8 weeks. Roughly 45% of patients had used the chimeric monoclonal antibody to TNF, infliximab (Remicade).
All study patients received 4 weeks of open-label adalimumab induction therapy and were stratified based on response at week 4 and prior infliximab use to high- or low-dose maintenance adalimumab. High-dose adalimumab was 40 mg every other week for patients weighing 40 kg or more and 20 mg every other week if less than 40 kg. Low-dose adalimumab was 20 mg every other week for patients weighing 40 kg or more and 10 mg every other week if less than 40 kg. Dose escalation was allowed for flare or non-response beginning at week 12.
At week 26, 39% of the high-dose patients and 28% of low-dose patients met the study’s primary end point of clinical remission, defined as a Pediatric Crohn’s Disease Activity Index of 10 or less, said Dr. Hyams, director of the gastroenterology department at Connecticut Children’s Medical Center in Hartford. In addition, more high-dose patients than low-dose patients achieved clinical remission at week 52 (33% vs. 23%). The difference between groups was not statistically significant at week 26 or week 52.
A clinical response, defined as a decrease in Pediatric Crohn’s Disease Activity Index of at least 15 points from baseline, was observed in more high-dose than low-dose patients at week 26 (59% vs. 48%) and week 52, with the difference reaching statistical significance only at week 52 (42% vs. 28%; P = .03), he said.
When the data were broken down according to prior infliximab use, remission rates among infliximab-experienced patients were similar between the high- and low-dose adalimumab arms at week 26 (17% vs. 20%) and week 52 (19% vs. 17%).
Among infliximab-naive patients, however, clinical remission rates were significantly greater at week 26 in the high-dose vs. low-dose group (57% vs. 35%, P = .026), especially among week-4 responders (63% for high-dose group vs. 38% for low-dose group, P = .016). In all, 82% of the 188 patients responded to induction at week 4. Remission rates among infliximab-naive patients were statistically similar at week 52 (45% vs. 28%, P = .065).
Dr. Hyams said there were no "obvious safety signals" among patients who received at least one maintenance dose of adalimumab. Serious adverse events were reported in 19 (20%) of the 95 low-dose patients and 22 (24%) of the 93 high-dose patients. Notably, serious infections were reported in only 3 low-dose (3.2%) and 5 high-dose (5.4%) patients. No malignancies were observed.
Adalimumab carries a boxed warning for an increased risk of serious infections leading to hospitalization or death, particularly tuberculosis. In August 2009, the Food and Drug Administration also required that boxed warnings be added to the TNF-blocker class of drugs because of an increased risk of lymphoma and other malignancies in children and adolescents.
When asked during a discussion of the study about the effect of adalimumab on fistulas, Dr. Hyams said that 15%-20% of patients had active fistulas,and a beneficial response to therapy occurred in about 50% of the low-dose patients and about 80% of the high-dose patients.
Another attendee asked if prior treatment with immunomodulators affected response, and Dr. Hyams said it did not. If the patient experienced a clinical response, corticosteroid therapy was tapered after week 4 and could be increased to the baseline dose for flare or nonresponse. Immunomodulator therapy could be discontinued at or after week 26 and could not be reinstated.
The study was sponsored by Abbott Laboratories and an Abbott employee prepared the first draft and assisted in the production of the slides. Dr. Hyams disclosed consulting and advisory committee/review panel participation and grant/research support from Abbott. Five of the 13 coauthors are Abbott employees and five others have financial relationships with Abbott.
CHICAGO – Adalimumab induced and maintained clinical remission in children with moderate to severe Crohn’s disease and the treatment was not associated with any new safety signals in a double-blind, phase III, randomized trial.
The effect was most apparent in patients who were infliximab naive, Dr. Jeffrey S. Hyams said at the annual Digestive Disease Week.
Adalimumab (Humira), a human monoclonal antibody to tumor necrosis factor (TNF)–alfa, is indicated for the treatment of a variety of conditions including Crohn’s disease in adults and juvenile idiopathic arthritis, but it is not approved for juvenile Crohn’s disease.
The study involved 188 patients, aged 6-17 years, with moderate to severe Crohn’s disease that had lasted for at least 12 weeks, despite concurrent treatment with oral corticosteroids for at least 2 weeks and/or immunomodulators for at least 8 weeks. Roughly 45% of patients had used the chimeric monoclonal antibody to TNF, infliximab (Remicade).
All study patients received 4 weeks of open-label adalimumab induction therapy and were stratified based on response at week 4 and prior infliximab use to high- or low-dose maintenance adalimumab. High-dose adalimumab was 40 mg every other week for patients weighing 40 kg or more and 20 mg every other week if less than 40 kg. Low-dose adalimumab was 20 mg every other week for patients weighing 40 kg or more and 10 mg every other week if less than 40 kg. Dose escalation was allowed for flare or non-response beginning at week 12.
At week 26, 39% of the high-dose patients and 28% of low-dose patients met the study’s primary end point of clinical remission, defined as a Pediatric Crohn’s Disease Activity Index of 10 or less, said Dr. Hyams, director of the gastroenterology department at Connecticut Children’s Medical Center in Hartford. In addition, more high-dose patients than low-dose patients achieved clinical remission at week 52 (33% vs. 23%). The difference between groups was not statistically significant at week 26 or week 52.
A clinical response, defined as a decrease in Pediatric Crohn’s Disease Activity Index of at least 15 points from baseline, was observed in more high-dose than low-dose patients at week 26 (59% vs. 48%) and week 52, with the difference reaching statistical significance only at week 52 (42% vs. 28%; P = .03), he said.
When the data were broken down according to prior infliximab use, remission rates among infliximab-experienced patients were similar between the high- and low-dose adalimumab arms at week 26 (17% vs. 20%) and week 52 (19% vs. 17%).
Among infliximab-naive patients, however, clinical remission rates were significantly greater at week 26 in the high-dose vs. low-dose group (57% vs. 35%, P = .026), especially among week-4 responders (63% for high-dose group vs. 38% for low-dose group, P = .016). In all, 82% of the 188 patients responded to induction at week 4. Remission rates among infliximab-naive patients were statistically similar at week 52 (45% vs. 28%, P = .065).
Dr. Hyams said there were no "obvious safety signals" among patients who received at least one maintenance dose of adalimumab. Serious adverse events were reported in 19 (20%) of the 95 low-dose patients and 22 (24%) of the 93 high-dose patients. Notably, serious infections were reported in only 3 low-dose (3.2%) and 5 high-dose (5.4%) patients. No malignancies were observed.
Adalimumab carries a boxed warning for an increased risk of serious infections leading to hospitalization or death, particularly tuberculosis. In August 2009, the Food and Drug Administration also required that boxed warnings be added to the TNF-blocker class of drugs because of an increased risk of lymphoma and other malignancies in children and adolescents.
When asked during a discussion of the study about the effect of adalimumab on fistulas, Dr. Hyams said that 15%-20% of patients had active fistulas,and a beneficial response to therapy occurred in about 50% of the low-dose patients and about 80% of the high-dose patients.
Another attendee asked if prior treatment with immunomodulators affected response, and Dr. Hyams said it did not. If the patient experienced a clinical response, corticosteroid therapy was tapered after week 4 and could be increased to the baseline dose for flare or nonresponse. Immunomodulator therapy could be discontinued at or after week 26 and could not be reinstated.
The study was sponsored by Abbott Laboratories and an Abbott employee prepared the first draft and assisted in the production of the slides. Dr. Hyams disclosed consulting and advisory committee/review panel participation and grant/research support from Abbott. Five of the 13 coauthors are Abbott employees and five others have financial relationships with Abbott.
Humira,
Humira,
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: At week 26, 39% of the high-dose adalimumab patients and 28% of the low-dose patients met the study’s primary end point of clinical remission.
Data Source: Phase III, multicenter, double-blind, randomized study of 188 pediatric patients with moderate to severe Crohn’s disease.
Disclosures: The study was sponsored by Abbott Laboratories, and an Abbott employee prepared the first draft and assisted in the production of the slides. Dr. Hyams disclosed consulting and advisory committee/review panel participation and grant/research support from Abbott. Five of the 13 coauthors are Abbott employees and five others have financial relationships with Abbott.
Continued Aspirin Use Does Not Impede Ulcer Healing
CHICAGO – Continued use of aspirin does not impair the healing of aspirin-related peptic ulcers under powerful proton pump inhibitor therapy, a randomized study in 160 patients suggests.
The ulcer healing rate, according to an intention-to-treat analysis, was 85.2% for patients receiving esomeprazole (Nexium) alone and 84.8% for those receiving esomeprazole plus aspirin. The per-protocol analysis showed nearly identical healing rates at 83.1% and 82.1%, Dr. Ping-I Hsu reported at the annual Digestive Disease Week.
The findings are noteworthy because patients are sometimes switched from aspirin to clopidogrel (Plavix) as an alternative treatment for aspirin-related peptic ulcers. There are no specific guidelines for the use of gastroprotective agents like proton pump inhibitors (PPIs) and clopidogrel. However, in a highly controversial move, the Food and Drug Administration discouraged concomitant use of clopidogrel and PPIs, especially omeprazole (Prilosec), because of a potential drug interaction.
Dr. Hsu pointed out that clopidogrel is far more expensive than aspirin, and that an earlier study showed that clopidogrel plus omeprazole had a similar ulcer healing rate as aspirin plus omeprazole (Aliment. Pharmacol. Ther. 2004;19:359-65).
"We therefore suggest that continuing aspirin use plus a powerful PPI is the best initial treatment of aspirin-related peptic ulcers," said Dr. Hsu, with the division of gastroenterology, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan.
The trial randomized 160 patients who were on low-dose aspirin and had a 3 mm or more peptic ulcer to esomeprazole 40 mg/day alone or with aspirin 100 mg/day for 8 weeks. Patients with Helicobacter pylori infection were treated with 10-day, standard triple therapy.
Exclusion criteria included serious medical illness or acute gastrointestinal bleeding, cardiovascular events within 6 months, history of partial gastrectomy, concomitant use of clopidogrel or anticoagulant and long-term use of NSAIDs.
Ten patients in the esomeprazole group and 12 in the combination group were excluded because of poor compliance or refusal of follow-up endoscopy, leaving 71 esomeprazole and 67 combination patients in the per-protocol analysis.
At baseline, the 81 esomeprazole patients and 79 esomeprazole plus aspirin patients were similar with respect to NSAID use (17% vs. 11%), prior peptic ulcer bleeding (12% vs. 14%), H. pylori infection (47% vs. 37%), and rates of underlying diseases such as diabetes mellitus (27% vs. 33%), hypertension (67% vs. 58%), coronary artery disease (52% vs. 57%), and cerebrovascular accident (10% vs. 15%). Their mean age was 69 years.
At week 8, Lanza scores decreased from 4 at baseline to 1.27 in each group, Dr. Hsu said.
Dyspepsia symptom scores decreased in the esomeprazole group from 1.78 to 0.50 and from 1.59 to 0.5 in the combination group. No patient in either group experienced ulcer bleeding or perforation.
Cardiovascular outcomes also were similar with or without continuous aspirin use. Only one case of unstable angina occurred in the combination group, and no patients experienced an acute MI, ischemic stroke or died, he said.
Independent risk factors predicting ulcer healing failure were diabetes mellitus (odds ratio, 3.2), use of steroids (OR, 12.1) and persistent H. pylori infection (OR, 20.2), Dr. Hsu said. The healing rate of ulcers with H. pylori infection was 25% vs. 84% without infection.
"Eradicating H. pylori is important for the healing of aspirin-related peptic ulcers," he said.
Dr. Hsu disclosed no conflicts of interest.
CHICAGO – Continued use of aspirin does not impair the healing of aspirin-related peptic ulcers under powerful proton pump inhibitor therapy, a randomized study in 160 patients suggests.
The ulcer healing rate, according to an intention-to-treat analysis, was 85.2% for patients receiving esomeprazole (Nexium) alone and 84.8% for those receiving esomeprazole plus aspirin. The per-protocol analysis showed nearly identical healing rates at 83.1% and 82.1%, Dr. Ping-I Hsu reported at the annual Digestive Disease Week.
The findings are noteworthy because patients are sometimes switched from aspirin to clopidogrel (Plavix) as an alternative treatment for aspirin-related peptic ulcers. There are no specific guidelines for the use of gastroprotective agents like proton pump inhibitors (PPIs) and clopidogrel. However, in a highly controversial move, the Food and Drug Administration discouraged concomitant use of clopidogrel and PPIs, especially omeprazole (Prilosec), because of a potential drug interaction.
Dr. Hsu pointed out that clopidogrel is far more expensive than aspirin, and that an earlier study showed that clopidogrel plus omeprazole had a similar ulcer healing rate as aspirin plus omeprazole (Aliment. Pharmacol. Ther. 2004;19:359-65).
"We therefore suggest that continuing aspirin use plus a powerful PPI is the best initial treatment of aspirin-related peptic ulcers," said Dr. Hsu, with the division of gastroenterology, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan.
The trial randomized 160 patients who were on low-dose aspirin and had a 3 mm or more peptic ulcer to esomeprazole 40 mg/day alone or with aspirin 100 mg/day for 8 weeks. Patients with Helicobacter pylori infection were treated with 10-day, standard triple therapy.
Exclusion criteria included serious medical illness or acute gastrointestinal bleeding, cardiovascular events within 6 months, history of partial gastrectomy, concomitant use of clopidogrel or anticoagulant and long-term use of NSAIDs.
Ten patients in the esomeprazole group and 12 in the combination group were excluded because of poor compliance or refusal of follow-up endoscopy, leaving 71 esomeprazole and 67 combination patients in the per-protocol analysis.
At baseline, the 81 esomeprazole patients and 79 esomeprazole plus aspirin patients were similar with respect to NSAID use (17% vs. 11%), prior peptic ulcer bleeding (12% vs. 14%), H. pylori infection (47% vs. 37%), and rates of underlying diseases such as diabetes mellitus (27% vs. 33%), hypertension (67% vs. 58%), coronary artery disease (52% vs. 57%), and cerebrovascular accident (10% vs. 15%). Their mean age was 69 years.
At week 8, Lanza scores decreased from 4 at baseline to 1.27 in each group, Dr. Hsu said.
Dyspepsia symptom scores decreased in the esomeprazole group from 1.78 to 0.50 and from 1.59 to 0.5 in the combination group. No patient in either group experienced ulcer bleeding or perforation.
Cardiovascular outcomes also were similar with or without continuous aspirin use. Only one case of unstable angina occurred in the combination group, and no patients experienced an acute MI, ischemic stroke or died, he said.
Independent risk factors predicting ulcer healing failure were diabetes mellitus (odds ratio, 3.2), use of steroids (OR, 12.1) and persistent H. pylori infection (OR, 20.2), Dr. Hsu said. The healing rate of ulcers with H. pylori infection was 25% vs. 84% without infection.
"Eradicating H. pylori is important for the healing of aspirin-related peptic ulcers," he said.
Dr. Hsu disclosed no conflicts of interest.
CHICAGO – Continued use of aspirin does not impair the healing of aspirin-related peptic ulcers under powerful proton pump inhibitor therapy, a randomized study in 160 patients suggests.
The ulcer healing rate, according to an intention-to-treat analysis, was 85.2% for patients receiving esomeprazole (Nexium) alone and 84.8% for those receiving esomeprazole plus aspirin. The per-protocol analysis showed nearly identical healing rates at 83.1% and 82.1%, Dr. Ping-I Hsu reported at the annual Digestive Disease Week.
The findings are noteworthy because patients are sometimes switched from aspirin to clopidogrel (Plavix) as an alternative treatment for aspirin-related peptic ulcers. There are no specific guidelines for the use of gastroprotective agents like proton pump inhibitors (PPIs) and clopidogrel. However, in a highly controversial move, the Food and Drug Administration discouraged concomitant use of clopidogrel and PPIs, especially omeprazole (Prilosec), because of a potential drug interaction.
Dr. Hsu pointed out that clopidogrel is far more expensive than aspirin, and that an earlier study showed that clopidogrel plus omeprazole had a similar ulcer healing rate as aspirin plus omeprazole (Aliment. Pharmacol. Ther. 2004;19:359-65).
"We therefore suggest that continuing aspirin use plus a powerful PPI is the best initial treatment of aspirin-related peptic ulcers," said Dr. Hsu, with the division of gastroenterology, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan.
The trial randomized 160 patients who were on low-dose aspirin and had a 3 mm or more peptic ulcer to esomeprazole 40 mg/day alone or with aspirin 100 mg/day for 8 weeks. Patients with Helicobacter pylori infection were treated with 10-day, standard triple therapy.
Exclusion criteria included serious medical illness or acute gastrointestinal bleeding, cardiovascular events within 6 months, history of partial gastrectomy, concomitant use of clopidogrel or anticoagulant and long-term use of NSAIDs.
Ten patients in the esomeprazole group and 12 in the combination group were excluded because of poor compliance or refusal of follow-up endoscopy, leaving 71 esomeprazole and 67 combination patients in the per-protocol analysis.
At baseline, the 81 esomeprazole patients and 79 esomeprazole plus aspirin patients were similar with respect to NSAID use (17% vs. 11%), prior peptic ulcer bleeding (12% vs. 14%), H. pylori infection (47% vs. 37%), and rates of underlying diseases such as diabetes mellitus (27% vs. 33%), hypertension (67% vs. 58%), coronary artery disease (52% vs. 57%), and cerebrovascular accident (10% vs. 15%). Their mean age was 69 years.
At week 8, Lanza scores decreased from 4 at baseline to 1.27 in each group, Dr. Hsu said.
Dyspepsia symptom scores decreased in the esomeprazole group from 1.78 to 0.50 and from 1.59 to 0.5 in the combination group. No patient in either group experienced ulcer bleeding or perforation.
Cardiovascular outcomes also were similar with or without continuous aspirin use. Only one case of unstable angina occurred in the combination group, and no patients experienced an acute MI, ischemic stroke or died, he said.
Independent risk factors predicting ulcer healing failure were diabetes mellitus (odds ratio, 3.2), use of steroids (OR, 12.1) and persistent H. pylori infection (OR, 20.2), Dr. Hsu said. The healing rate of ulcers with H. pylori infection was 25% vs. 84% without infection.
"Eradicating H. pylori is important for the healing of aspirin-related peptic ulcers," he said.
Dr. Hsu disclosed no conflicts of interest.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: The ulcer healing rate by intention-to-treat analysis was 85.2% with esomeprazole alone and 84.8% with esomeprazole plus aspirin.
Data Source: Randomized study of 160 patients with aspirin-related peptic ulcers.
Disclosures: Dr. Hsu disclosed no conflicts of interest.
Continued Aspirin Use Does Not Impede Ulcer Healing
CHICAGO – Continued use of aspirin does not impair the healing of aspirin-related peptic ulcers under powerful proton pump inhibitor therapy, a randomized study in 160 patients suggests.
The ulcer healing rate, according to an intention-to-treat analysis, was 85.2% for patients receiving esomeprazole (Nexium) alone and 84.8% for those receiving esomeprazole plus aspirin. The per-protocol analysis showed nearly identical healing rates at 83.1% and 82.1%, Dr. Ping-I Hsu reported at the annual Digestive Disease Week.
The findings are noteworthy because patients are sometimes switched from aspirin to clopidogrel (Plavix) as an alternative treatment for aspirin-related peptic ulcers. There are no specific guidelines for the use of gastroprotective agents like proton pump inhibitors (PPIs) and clopidogrel. However, in a highly controversial move, the Food and Drug Administration discouraged concomitant use of clopidogrel and PPIs, especially omeprazole (Prilosec), because of a potential drug interaction.
Dr. Hsu pointed out that clopidogrel is far more expensive than aspirin, and that an earlier study showed that clopidogrel plus omeprazole had a similar ulcer healing rate as aspirin plus omeprazole (Aliment. Pharmacol. Ther. 2004;19:359-65).
"We therefore suggest that continuing aspirin use plus a powerful PPI is the best initial treatment of aspirin-related peptic ulcers," said Dr. Hsu, with the division of gastroenterology, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan.
The trial randomized 160 patients who were on low-dose aspirin and had a 3 mm or more peptic ulcer to esomeprazole 40 mg/day alone or with aspirin 100 mg/day for 8 weeks. Patients with Helicobacter pylori infection were treated with 10-day, standard triple therapy.
Exclusion criteria included serious medical illness or acute gastrointestinal bleeding, cardiovascular events within 6 months, history of partial gastrectomy, concomitant use of clopidogrel or anticoagulant and long-term use of NSAIDs.
Ten patients in the esomeprazole group and 12 in the combination group were excluded because of poor compliance or refusal of follow-up endoscopy, leaving 71 esomeprazole and 67 combination patients in the per-protocol analysis.
At baseline, the 81 esomeprazole patients and 79 esomeprazole plus aspirin patients were similar with respect to NSAID use (17% vs. 11%), prior peptic ulcer bleeding (12% vs. 14%), H. pylori infection (47% vs. 37%), and rates of underlying diseases such as diabetes mellitus (27% vs. 33%), hypertension (67% vs. 58%), coronary artery disease (52% vs. 57%), and cerebrovascular accident (10% vs. 15%). Their mean age was 69 years.
At week 8, Lanza scores decreased from 4 at baseline to 1.27 in each group, Dr. Hsu said.
Dyspepsia symptom scores decreased in the esomeprazole group from 1.78 to 0.50 and from 1.59 to 0.5 in the combination group. No patient in either group experienced ulcer bleeding or perforation.
Cardiovascular outcomes also were similar with or without continuous aspirin use. Only one case of unstable angina occurred in the combination group, and no patients experienced an acute MI, ischemic stroke or died, he said.
Independent risk factors predicting ulcer healing failure were diabetes mellitus (odds ratio, 3.2), use of steroids (OR, 12.1) and persistent H. pylori infection (OR, 20.2), Dr. Hsu said. The healing rate of ulcers with H. pylori infection was 25% vs. 84% without infection.
"Eradicating H. pylori is important for the healing of aspirin-related peptic ulcers," he said.
Dr. Hsu disclosed no conflicts of interest.
CHICAGO – Continued use of aspirin does not impair the healing of aspirin-related peptic ulcers under powerful proton pump inhibitor therapy, a randomized study in 160 patients suggests.
The ulcer healing rate, according to an intention-to-treat analysis, was 85.2% for patients receiving esomeprazole (Nexium) alone and 84.8% for those receiving esomeprazole plus aspirin. The per-protocol analysis showed nearly identical healing rates at 83.1% and 82.1%, Dr. Ping-I Hsu reported at the annual Digestive Disease Week.
The findings are noteworthy because patients are sometimes switched from aspirin to clopidogrel (Plavix) as an alternative treatment for aspirin-related peptic ulcers. There are no specific guidelines for the use of gastroprotective agents like proton pump inhibitors (PPIs) and clopidogrel. However, in a highly controversial move, the Food and Drug Administration discouraged concomitant use of clopidogrel and PPIs, especially omeprazole (Prilosec), because of a potential drug interaction.
Dr. Hsu pointed out that clopidogrel is far more expensive than aspirin, and that an earlier study showed that clopidogrel plus omeprazole had a similar ulcer healing rate as aspirin plus omeprazole (Aliment. Pharmacol. Ther. 2004;19:359-65).
"We therefore suggest that continuing aspirin use plus a powerful PPI is the best initial treatment of aspirin-related peptic ulcers," said Dr. Hsu, with the division of gastroenterology, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan.
The trial randomized 160 patients who were on low-dose aspirin and had a 3 mm or more peptic ulcer to esomeprazole 40 mg/day alone or with aspirin 100 mg/day for 8 weeks. Patients with Helicobacter pylori infection were treated with 10-day, standard triple therapy.
Exclusion criteria included serious medical illness or acute gastrointestinal bleeding, cardiovascular events within 6 months, history of partial gastrectomy, concomitant use of clopidogrel or anticoagulant and long-term use of NSAIDs.
Ten patients in the esomeprazole group and 12 in the combination group were excluded because of poor compliance or refusal of follow-up endoscopy, leaving 71 esomeprazole and 67 combination patients in the per-protocol analysis.
At baseline, the 81 esomeprazole patients and 79 esomeprazole plus aspirin patients were similar with respect to NSAID use (17% vs. 11%), prior peptic ulcer bleeding (12% vs. 14%), H. pylori infection (47% vs. 37%), and rates of underlying diseases such as diabetes mellitus (27% vs. 33%), hypertension (67% vs. 58%), coronary artery disease (52% vs. 57%), and cerebrovascular accident (10% vs. 15%). Their mean age was 69 years.
At week 8, Lanza scores decreased from 4 at baseline to 1.27 in each group, Dr. Hsu said.
Dyspepsia symptom scores decreased in the esomeprazole group from 1.78 to 0.50 and from 1.59 to 0.5 in the combination group. No patient in either group experienced ulcer bleeding or perforation.
Cardiovascular outcomes also were similar with or without continuous aspirin use. Only one case of unstable angina occurred in the combination group, and no patients experienced an acute MI, ischemic stroke or died, he said.
Independent risk factors predicting ulcer healing failure were diabetes mellitus (odds ratio, 3.2), use of steroids (OR, 12.1) and persistent H. pylori infection (OR, 20.2), Dr. Hsu said. The healing rate of ulcers with H. pylori infection was 25% vs. 84% without infection.
"Eradicating H. pylori is important for the healing of aspirin-related peptic ulcers," he said.
Dr. Hsu disclosed no conflicts of interest.
CHICAGO – Continued use of aspirin does not impair the healing of aspirin-related peptic ulcers under powerful proton pump inhibitor therapy, a randomized study in 160 patients suggests.
The ulcer healing rate, according to an intention-to-treat analysis, was 85.2% for patients receiving esomeprazole (Nexium) alone and 84.8% for those receiving esomeprazole plus aspirin. The per-protocol analysis showed nearly identical healing rates at 83.1% and 82.1%, Dr. Ping-I Hsu reported at the annual Digestive Disease Week.
The findings are noteworthy because patients are sometimes switched from aspirin to clopidogrel (Plavix) as an alternative treatment for aspirin-related peptic ulcers. There are no specific guidelines for the use of gastroprotective agents like proton pump inhibitors (PPIs) and clopidogrel. However, in a highly controversial move, the Food and Drug Administration discouraged concomitant use of clopidogrel and PPIs, especially omeprazole (Prilosec), because of a potential drug interaction.
Dr. Hsu pointed out that clopidogrel is far more expensive than aspirin, and that an earlier study showed that clopidogrel plus omeprazole had a similar ulcer healing rate as aspirin plus omeprazole (Aliment. Pharmacol. Ther. 2004;19:359-65).
"We therefore suggest that continuing aspirin use plus a powerful PPI is the best initial treatment of aspirin-related peptic ulcers," said Dr. Hsu, with the division of gastroenterology, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan.
The trial randomized 160 patients who were on low-dose aspirin and had a 3 mm or more peptic ulcer to esomeprazole 40 mg/day alone or with aspirin 100 mg/day for 8 weeks. Patients with Helicobacter pylori infection were treated with 10-day, standard triple therapy.
Exclusion criteria included serious medical illness or acute gastrointestinal bleeding, cardiovascular events within 6 months, history of partial gastrectomy, concomitant use of clopidogrel or anticoagulant and long-term use of NSAIDs.
Ten patients in the esomeprazole group and 12 in the combination group were excluded because of poor compliance or refusal of follow-up endoscopy, leaving 71 esomeprazole and 67 combination patients in the per-protocol analysis.
At baseline, the 81 esomeprazole patients and 79 esomeprazole plus aspirin patients were similar with respect to NSAID use (17% vs. 11%), prior peptic ulcer bleeding (12% vs. 14%), H. pylori infection (47% vs. 37%), and rates of underlying diseases such as diabetes mellitus (27% vs. 33%), hypertension (67% vs. 58%), coronary artery disease (52% vs. 57%), and cerebrovascular accident (10% vs. 15%). Their mean age was 69 years.
At week 8, Lanza scores decreased from 4 at baseline to 1.27 in each group, Dr. Hsu said.
Dyspepsia symptom scores decreased in the esomeprazole group from 1.78 to 0.50 and from 1.59 to 0.5 in the combination group. No patient in either group experienced ulcer bleeding or perforation.
Cardiovascular outcomes also were similar with or without continuous aspirin use. Only one case of unstable angina occurred in the combination group, and no patients experienced an acute MI, ischemic stroke or died, he said.
Independent risk factors predicting ulcer healing failure were diabetes mellitus (odds ratio, 3.2), use of steroids (OR, 12.1) and persistent H. pylori infection (OR, 20.2), Dr. Hsu said. The healing rate of ulcers with H. pylori infection was 25% vs. 84% without infection.
"Eradicating H. pylori is important for the healing of aspirin-related peptic ulcers," he said.
Dr. Hsu disclosed no conflicts of interest.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: The ulcer healing rate by intention-to-treat analysis was 85.2% with esomeprazole alone and 84.8% with esomeprazole plus aspirin.
Data Source: Randomized study of 160 patients with aspirin-related peptic ulcers.
Disclosures: Dr. Hsu disclosed no conflicts of interest.
Cyclosporine No Better Than Infliximab for Ulcerative Colitis
CHICAGO – A randomized, multicenter open-label trial found that cyclosporine was not more effective than infliximab in patients with acute, severe ulcerative colitis refractory to intravenous steroids, according to Dr. David Laharie.
Acute severe ulcerative colitis (UC) occurs in about 25% of patients with UC, and while intravenous corticosteroids are the primary therapy, 40% of patients are refractory to them. After steroid failure, only two medical options are available to avoid colectomy: cyclosporine and infliximab.
"However, there has been no randomized clinical trial comparing the two," said Dr. Laharie of Centre Hospitalier Universitaire in Bordeaux, France. He presented the findings of a multicenter, randomized open-label study comparing cyclosporine with infliximab in severe acute UC refractory to intravenous steroids. This study found cyclosporine to be no more effective than infliximab in this population, he said at the annual Digestive Disease Week.
Patients with steroid-refractory acute severe UC were randomized to cyclosporine (55 patients) or infliximab (56 patients). The researchers sought to determine whether treatment failure was less frequent with cyclosporine than with infliximab.
Adults were randomized if they were having a severe acute flare of UC (Lichtiger score greater than 10) and were refractory to intravenous steroid therapy (greater than or equal to 0.8 mg/kg per day of methylprednisone or equivalent) for at least 5 days. They had to be naive to the two treatment drugs and could not be under treatment with azathioprine/6-mercaptopurine unless therapy had been initiated fewer than 4 weeks before randomization.
The two groups were treated for up to 98 days, and the trial’s primary end point was treatment failure, defined as an absence of early clinical response, relapse after day 7, colectomy, absence of remission off steroids at the trial’s end, a severe adverse event, or death. Secondary end points included the Lichtiger score from day 0 to day 7, the percentage of patients showing clinical response at day 7, endoscopic response and colectomy at day 98, and the number of severe adverse events.
Approximately half the patients in both groups were female, with a median age of approximately 37 years, and had UC for at least 1 year. More than 90% of patients in both groups were naive to azathioprine. Lichtiger scores in both groups were 11 and over, and Mayo scores ranged from less than or equal to 0 to 12.
For the primary end point of treatment failure, 60% failed in the cyclosporine arm versus 54% in the infliximab arm, a nonsignificant difference.
The response rate at day 7 was 85.4% in the cyclosporine arm versus 85.7% in the infliximab arm, also not a significant difference. Response was defined as a Lichtiger score less than 10, and a decrease of at least 3 points compared with baseline.
The Lichtiger score from day 0 to day 6 showed that the median time to clinical response was 4 days (interquartile range [IQR], 3-6) with infliximab, versus 5 days (IQR, 4-7) for cyclosporine, a significant difference (P = .046).
At day 98, signs of mucosal healing were found in 52% of patients in the cyclosporine group and 53% of patients in the infliximab group. Healing was defined as having a Mayo endoscopic subscore of 0-1.
The colectomy rates were 18% in the cyclosporine arm and 21% in the infliximab arm. Severe adverse events affected 15% (8 patients) in the cyclosporine group and 25% (14 patients) in the infliximab group. Three patients developed cytomegalovirus colitis and two developed septicemia.
"In acute severe ulcerative colitis refractory to intravenous steroids, cyclosporine was not more effective than infliximab," said Dr. Laharie. "The short-term response was achieved with both drugs in more than 80% of patients within 1 week. Three-month colectomy rates were similar (18% with cyclosporine versus 21% with infliximab). And in this severe population, both drugs were well tolerated," he said.
Dr. Laharie disclosed financial relationships with Schering-Plough and Abbott Laboratories (royalty, speaking, and teaching), and with Norgine (consulting fee and board membership). The study received support from the Association François Aupetit, the Société Nationale Française de Gastro-Entérologie, and the International Organization for the Study of Inflammatory Bowel Disease, and was sponsored by Groupe d’Etude Thérapeutique des Affections Inflammatoires du Tube Digestif.
CHICAGO – A randomized, multicenter open-label trial found that cyclosporine was not more effective than infliximab in patients with acute, severe ulcerative colitis refractory to intravenous steroids, according to Dr. David Laharie.
Acute severe ulcerative colitis (UC) occurs in about 25% of patients with UC, and while intravenous corticosteroids are the primary therapy, 40% of patients are refractory to them. After steroid failure, only two medical options are available to avoid colectomy: cyclosporine and infliximab.
"However, there has been no randomized clinical trial comparing the two," said Dr. Laharie of Centre Hospitalier Universitaire in Bordeaux, France. He presented the findings of a multicenter, randomized open-label study comparing cyclosporine with infliximab in severe acute UC refractory to intravenous steroids. This study found cyclosporine to be no more effective than infliximab in this population, he said at the annual Digestive Disease Week.
Patients with steroid-refractory acute severe UC were randomized to cyclosporine (55 patients) or infliximab (56 patients). The researchers sought to determine whether treatment failure was less frequent with cyclosporine than with infliximab.
Adults were randomized if they were having a severe acute flare of UC (Lichtiger score greater than 10) and were refractory to intravenous steroid therapy (greater than or equal to 0.8 mg/kg per day of methylprednisone or equivalent) for at least 5 days. They had to be naive to the two treatment drugs and could not be under treatment with azathioprine/6-mercaptopurine unless therapy had been initiated fewer than 4 weeks before randomization.
The two groups were treated for up to 98 days, and the trial’s primary end point was treatment failure, defined as an absence of early clinical response, relapse after day 7, colectomy, absence of remission off steroids at the trial’s end, a severe adverse event, or death. Secondary end points included the Lichtiger score from day 0 to day 7, the percentage of patients showing clinical response at day 7, endoscopic response and colectomy at day 98, and the number of severe adverse events.
Approximately half the patients in both groups were female, with a median age of approximately 37 years, and had UC for at least 1 year. More than 90% of patients in both groups were naive to azathioprine. Lichtiger scores in both groups were 11 and over, and Mayo scores ranged from less than or equal to 0 to 12.
For the primary end point of treatment failure, 60% failed in the cyclosporine arm versus 54% in the infliximab arm, a nonsignificant difference.
The response rate at day 7 was 85.4% in the cyclosporine arm versus 85.7% in the infliximab arm, also not a significant difference. Response was defined as a Lichtiger score less than 10, and a decrease of at least 3 points compared with baseline.
The Lichtiger score from day 0 to day 6 showed that the median time to clinical response was 4 days (interquartile range [IQR], 3-6) with infliximab, versus 5 days (IQR, 4-7) for cyclosporine, a significant difference (P = .046).
At day 98, signs of mucosal healing were found in 52% of patients in the cyclosporine group and 53% of patients in the infliximab group. Healing was defined as having a Mayo endoscopic subscore of 0-1.
The colectomy rates were 18% in the cyclosporine arm and 21% in the infliximab arm. Severe adverse events affected 15% (8 patients) in the cyclosporine group and 25% (14 patients) in the infliximab group. Three patients developed cytomegalovirus colitis and two developed septicemia.
"In acute severe ulcerative colitis refractory to intravenous steroids, cyclosporine was not more effective than infliximab," said Dr. Laharie. "The short-term response was achieved with both drugs in more than 80% of patients within 1 week. Three-month colectomy rates were similar (18% with cyclosporine versus 21% with infliximab). And in this severe population, both drugs were well tolerated," he said.
Dr. Laharie disclosed financial relationships with Schering-Plough and Abbott Laboratories (royalty, speaking, and teaching), and with Norgine (consulting fee and board membership). The study received support from the Association François Aupetit, the Société Nationale Française de Gastro-Entérologie, and the International Organization for the Study of Inflammatory Bowel Disease, and was sponsored by Groupe d’Etude Thérapeutique des Affections Inflammatoires du Tube Digestif.
CHICAGO – A randomized, multicenter open-label trial found that cyclosporine was not more effective than infliximab in patients with acute, severe ulcerative colitis refractory to intravenous steroids, according to Dr. David Laharie.
Acute severe ulcerative colitis (UC) occurs in about 25% of patients with UC, and while intravenous corticosteroids are the primary therapy, 40% of patients are refractory to them. After steroid failure, only two medical options are available to avoid colectomy: cyclosporine and infliximab.
"However, there has been no randomized clinical trial comparing the two," said Dr. Laharie of Centre Hospitalier Universitaire in Bordeaux, France. He presented the findings of a multicenter, randomized open-label study comparing cyclosporine with infliximab in severe acute UC refractory to intravenous steroids. This study found cyclosporine to be no more effective than infliximab in this population, he said at the annual Digestive Disease Week.
Patients with steroid-refractory acute severe UC were randomized to cyclosporine (55 patients) or infliximab (56 patients). The researchers sought to determine whether treatment failure was less frequent with cyclosporine than with infliximab.
Adults were randomized if they were having a severe acute flare of UC (Lichtiger score greater than 10) and were refractory to intravenous steroid therapy (greater than or equal to 0.8 mg/kg per day of methylprednisone or equivalent) for at least 5 days. They had to be naive to the two treatment drugs and could not be under treatment with azathioprine/6-mercaptopurine unless therapy had been initiated fewer than 4 weeks before randomization.
The two groups were treated for up to 98 days, and the trial’s primary end point was treatment failure, defined as an absence of early clinical response, relapse after day 7, colectomy, absence of remission off steroids at the trial’s end, a severe adverse event, or death. Secondary end points included the Lichtiger score from day 0 to day 7, the percentage of patients showing clinical response at day 7, endoscopic response and colectomy at day 98, and the number of severe adverse events.
Approximately half the patients in both groups were female, with a median age of approximately 37 years, and had UC for at least 1 year. More than 90% of patients in both groups were naive to azathioprine. Lichtiger scores in both groups were 11 and over, and Mayo scores ranged from less than or equal to 0 to 12.
For the primary end point of treatment failure, 60% failed in the cyclosporine arm versus 54% in the infliximab arm, a nonsignificant difference.
The response rate at day 7 was 85.4% in the cyclosporine arm versus 85.7% in the infliximab arm, also not a significant difference. Response was defined as a Lichtiger score less than 10, and a decrease of at least 3 points compared with baseline.
The Lichtiger score from day 0 to day 6 showed that the median time to clinical response was 4 days (interquartile range [IQR], 3-6) with infliximab, versus 5 days (IQR, 4-7) for cyclosporine, a significant difference (P = .046).
At day 98, signs of mucosal healing were found in 52% of patients in the cyclosporine group and 53% of patients in the infliximab group. Healing was defined as having a Mayo endoscopic subscore of 0-1.
The colectomy rates were 18% in the cyclosporine arm and 21% in the infliximab arm. Severe adverse events affected 15% (8 patients) in the cyclosporine group and 25% (14 patients) in the infliximab group. Three patients developed cytomegalovirus colitis and two developed septicemia.
"In acute severe ulcerative colitis refractory to intravenous steroids, cyclosporine was not more effective than infliximab," said Dr. Laharie. "The short-term response was achieved with both drugs in more than 80% of patients within 1 week. Three-month colectomy rates were similar (18% with cyclosporine versus 21% with infliximab). And in this severe population, both drugs were well tolerated," he said.
Dr. Laharie disclosed financial relationships with Schering-Plough and Abbott Laboratories (royalty, speaking, and teaching), and with Norgine (consulting fee and board membership). The study received support from the Association François Aupetit, the Société Nationale Française de Gastro-Entérologie, and the International Organization for the Study of Inflammatory Bowel Disease, and was sponsored by Groupe d’Etude Thérapeutique des Affections Inflammatoires du Tube Digestif.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: In the treatment of acute severe ulcerative colitis refractory to intravenous steroids, cyclosporine was not more effective than infliximab: More than 80% of patients in both treatment arms responded to therapy within 1 week, and the 3-month colectomy rates were similar (18% with cyclosporine vs. 21% with infliximab).
Data Source: Multicenter, randomized, open-label study of 111 patients treated with either cyclosporine or infliximab.
Disclosures: Dr. Laharie disclosed financial relationships with Schering-Plough and Abbott Laboratories (royalty, speaking, and teaching), and with Norgine (consulting fee and board membership). The study received support from the Association François Aupetit, the Société Nationale Française de Gastro-Entérologie, and the International Organization for the Study of Inflammatory Bowel Disease, and was sponsored by Groupe d’Etude Thérapeutique des Affections Inflammatoires du Tube Digestif.