User login
Idiopathic myointimal hyperplasia of the mesenteric veins
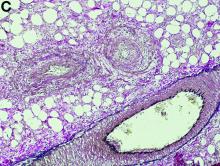
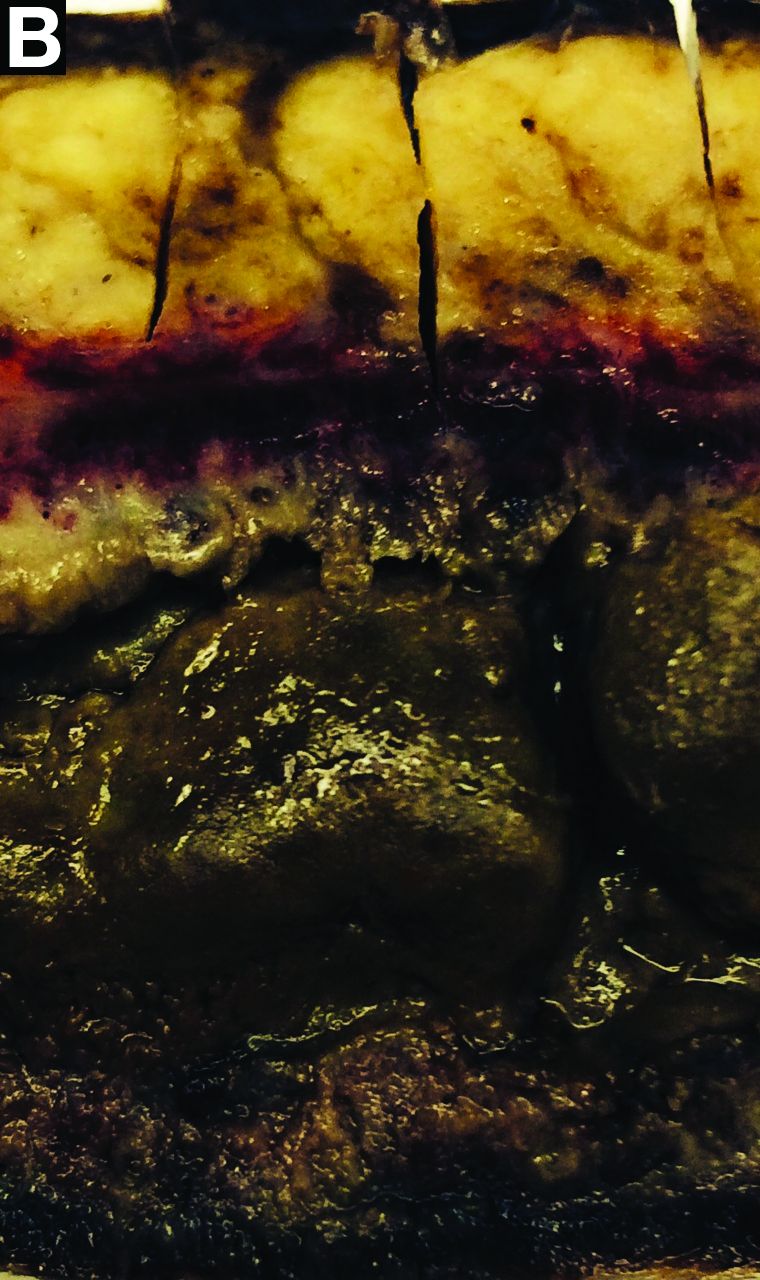
Gross examination of the rectosigmoid colon resected from this patient demonstrated transmural fibrosis. The mucosa was necrotic and hemorrhagic with a granular and cobblestone pattern (Figure B). Histopathologic examination of the mucosa revealed veins with myointimal hyperplasia with sparing of arterial vasculature (Figure C; stain: elastin; original magnification, ×10). The combined findings via endoscopy and histopathology confirmed the diagnosis of idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV).
IMHMV is a rare cause of proctosigmoiditis first described in a case series of 4 patients in 1991 by Genta and Haggitt.1 Owing to its clinical presentation of lower quadrant abdominal pain, diarrhea, hematochezia, and mucous in the stools, the diagnosis is often mistaken for inflammatory bowel disease. However, the endoscopic and pathologic findings of IHMVH resemble ischemic colitis. IMHMV is refractory to medical treatment and its definitive diagnosis and curative management involves surgical resection of the involved segment (often the rectosigmoid colon). The precise pathophysiology of IMHMV is unclear. Histopathologic analysis of veins in the involved segment of colon can demonstrate changes similar to those of failed saphenous grafts from coronary artery bypass.2 Myointimal hyperplasia of the mesenteric veins occurs (best identified with elastin stain on histopathology) with near total occlusion of the venous lumen and without any associated inflammatory infiltrate or arterial involvement.3
After colectomy, our patient’s abdominal symptoms resolved and follow-up colonoscopy at 6 months did not reveal recurrence of IMHMV, at which time, the patient underwent take-down of his colostomy. In the year after colostomy take-down, the patient showed no clinical or endoscopic signs of colitis while off of all medical therapies. Here, we present the first case of a successful take-down of a curative colostomy for an IMHMV patient, a treatment course not described previously in the literature. Prompt diagnosis and timely surgical intervention may allow for avoidance of permanent colostomy in patients with IMHMV.
References
1. Genta R.M., Haggitt, R.C. Idiopathic myointimal hyperplasia of mesenteric veins. Gastroenterology. 1991;101:533-9.
2. Abu-Alfa A.K., Ayer U., West A.B. Mucosal biopsy findings and venous abnormalities in idiopathic myointimal hyperplasia of the mesenteric veins. Am J Surg Pathol. 1996;20:1271-8.
3. Chiang C.K., Lee C.L., Huang C.S., et al. A rare cause of ischemic proctosigmoiditis: Idiopathic myointimal hyperplasia of mesenteric veins. Endoscopy. 2012;44:54-5.
Idiopathic myointimal hyperplasia of the mesenteric veins
Gross examination of the rectosigmoid colon resected from this patient demonstrated transmural fibrosis. The mucosa was necrotic and hemorrhagic with a granular and cobblestone pattern (Figure B). Histopathologic examination of the mucosa revealed veins with myointimal hyperplasia with sparing of arterial vasculature (Figure C; stain: elastin; original magnification, ×10). The combined findings via endoscopy and histopathology confirmed the diagnosis of idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV).
IMHMV is a rare cause of proctosigmoiditis first described in a case series of 4 patients in 1991 by Genta and Haggitt.1 Owing to its clinical presentation of lower quadrant abdominal pain, diarrhea, hematochezia, and mucous in the stools, the diagnosis is often mistaken for inflammatory bowel disease. However, the endoscopic and pathologic findings of IHMVH resemble ischemic colitis. IMHMV is refractory to medical treatment and its definitive diagnosis and curative management involves surgical resection of the involved segment (often the rectosigmoid colon). The precise pathophysiology of IMHMV is unclear. Histopathologic analysis of veins in the involved segment of colon can demonstrate changes similar to those of failed saphenous grafts from coronary artery bypass.2 Myointimal hyperplasia of the mesenteric veins occurs (best identified with elastin stain on histopathology) with near total occlusion of the venous lumen and without any associated inflammatory infiltrate or arterial involvement.3
After colectomy, our patient’s abdominal symptoms resolved and follow-up colonoscopy at 6 months did not reveal recurrence of IMHMV, at which time, the patient underwent take-down of his colostomy. In the year after colostomy take-down, the patient showed no clinical or endoscopic signs of colitis while off of all medical therapies. Here, we present the first case of a successful take-down of a curative colostomy for an IMHMV patient, a treatment course not described previously in the literature. Prompt diagnosis and timely surgical intervention may allow for avoidance of permanent colostomy in patients with IMHMV.
References
1. Genta R.M., Haggitt, R.C. Idiopathic myointimal hyperplasia of mesenteric veins. Gastroenterology. 1991;101:533-9.
2. Abu-Alfa A.K., Ayer U., West A.B. Mucosal biopsy findings and venous abnormalities in idiopathic myointimal hyperplasia of the mesenteric veins. Am J Surg Pathol. 1996;20:1271-8.
3. Chiang C.K., Lee C.L., Huang C.S., et al. A rare cause of ischemic proctosigmoiditis: Idiopathic myointimal hyperplasia of mesenteric veins. Endoscopy. 2012;44:54-5.
Idiopathic myointimal hyperplasia of the mesenteric veins
Gross examination of the rectosigmoid colon resected from this patient demonstrated transmural fibrosis. The mucosa was necrotic and hemorrhagic with a granular and cobblestone pattern (Figure B). Histopathologic examination of the mucosa revealed veins with myointimal hyperplasia with sparing of arterial vasculature (Figure C; stain: elastin; original magnification, ×10). The combined findings via endoscopy and histopathology confirmed the diagnosis of idiopathic myointimal hyperplasia of the mesenteric veins (IMHMV).
IMHMV is a rare cause of proctosigmoiditis first described in a case series of 4 patients in 1991 by Genta and Haggitt.1 Owing to its clinical presentation of lower quadrant abdominal pain, diarrhea, hematochezia, and mucous in the stools, the diagnosis is often mistaken for inflammatory bowel disease. However, the endoscopic and pathologic findings of IHMVH resemble ischemic colitis. IMHMV is refractory to medical treatment and its definitive diagnosis and curative management involves surgical resection of the involved segment (often the rectosigmoid colon). The precise pathophysiology of IMHMV is unclear. Histopathologic analysis of veins in the involved segment of colon can demonstrate changes similar to those of failed saphenous grafts from coronary artery bypass.2 Myointimal hyperplasia of the mesenteric veins occurs (best identified with elastin stain on histopathology) with near total occlusion of the venous lumen and without any associated inflammatory infiltrate or arterial involvement.3
After colectomy, our patient’s abdominal symptoms resolved and follow-up colonoscopy at 6 months did not reveal recurrence of IMHMV, at which time, the patient underwent take-down of his colostomy. In the year after colostomy take-down, the patient showed no clinical or endoscopic signs of colitis while off of all medical therapies. Here, we present the first case of a successful take-down of a curative colostomy for an IMHMV patient, a treatment course not described previously in the literature. Prompt diagnosis and timely surgical intervention may allow for avoidance of permanent colostomy in patients with IMHMV.
References
1. Genta R.M., Haggitt, R.C. Idiopathic myointimal hyperplasia of mesenteric veins. Gastroenterology. 1991;101:533-9.
2. Abu-Alfa A.K., Ayer U., West A.B. Mucosal biopsy findings and venous abnormalities in idiopathic myointimal hyperplasia of the mesenteric veins. Am J Surg Pathol. 1996;20:1271-8.
3. Chiang C.K., Lee C.L., Huang C.S., et al. A rare cause of ischemic proctosigmoiditis: Idiopathic myointimal hyperplasia of mesenteric veins. Endoscopy. 2012;44:54-5.