User login
ORLANDO – Overall cancer death rates are dropping dramatically, but pancreatic cancer mortality remains high.
“By 2020 we expect [pancreatic cancer] to be the second most common cause of cancer-related death, exceeded only by lung cancer, and if lung cancer deaths continue to fall – which we expect that they will – it will be the most common cause of cancer-related death,” Margaret A. Tempero, MD, said at the annual conference of the National Comprehensive Cancer Network.
Further, as the population ages there will be an increasing number of patients presenting with pancreatic cancer, said Dr. Tempero of the University of California, San Francisco.
Currently, 80% of pancreatic cancer patients are diagnosed with disease that is not amenable to resection, and 80% of those who have resection and adjuvant therapy experience relapse. The overall survival rate is only about 9%.
“This is really, really an aggressive malignancy,” Dr. Tempero said, noting that the survival among those with metastases who do not receive treatment is only about 3 months.
There are no early symptoms that direct attention to the pancreas. Additionally, some patients experience very early invasion and metastases; in fact, up to two-thirds of patients with lesions only 1 cm in size will already have lymph node metastasis, she said.
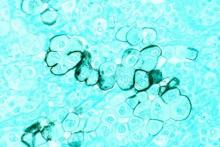
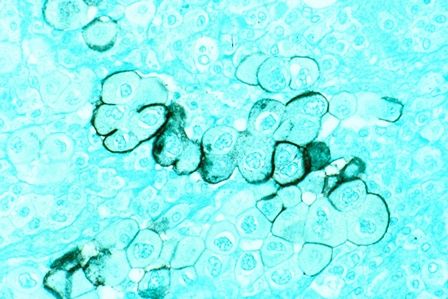
The disease tends to be chemoresistant, although this may be changing with treatment advances, but it is characterized by “a lot of desmoplastic stroma, so there’s a lot of microenvironment that’s perturbed around the malignancy,” making it difficult for drugs to permeate the stroma.
“That’s something we’re actively working on – ways that we can actually change the stroma so that we can get more drug into the cancer,” she said.
Another challenge is the disease’s “habit of elaborating a lot of cytokines that disable the person with the disease,” which can lead to frailty that makes it difficult to deliver potentially effective therapies that are well tolerated in patients with other types of cancer, she noted.
An important question is whether pancreatic cancer is diagnosed too late or metastasizes too early, and there is evidence to support both possibilities.
“Either way ... we need to work on better treatment,” she said.
Resectable/borderline resectable disease
One noteworthy recent advance for patients with resectable/borderline resectable disease is the addition of capecitabine to gemcitabine for adjuvant therapy. In the ESPAC 4 study published in March in the Lancet, the combination of gemcitabine and capecitabine showed a clear benefit over gemcitabine alone.
“So that has now entered [the NCCN] guidelines as an important option for adjuvant therapy,” said Dr. Tempero, chair of the NCCN pancreatic cancer guidelines panel.
Ongoing trials are also looking at the FOLFIRINOX (irinotecan plus 5-fluorouracil plus leucovorin plus oxaliplatin) and gemcitabine/nanoparticle albumin-bound paclitaxel (nab-P) regimens in the adjuvant setting. These have previously shown some efficacy in the metastatic setting.
“So we really wanted to get these therapies into the adjuvant setting as soon as we could,” she said.
In the ACCORD trial, FOLFIRINOX is being compared with gemcitabine in the postoperative adjuvant setting, and the APACT trial comparing gemcitabine/nab-P to gemcitabine monotherapy completed accrual last year.
“I’m pretty sure that we’ll have enough events on the APACT study by the end of this year, and hopefully we can present that data in the spring. I’m hoping it will be a positive trial for us,” she said.
Neoadjuvant therapy – a successful strategy used in many other malignancies – is also being looked at for pancreatic cancer.
A pilot study (A021101) completed last year suggested that chemotherapy (FOLFIRINOX for 2 months) and chemoradiation (capecitabine and radiation at 50.4 Gy) followed by surgical resection and adjuvant chemotherapy (gemcitabine for 2 months) provided some benefit in patients with borderline resectable pancreatic cancer. This trial led to another ongoing study (S1505) in which patients with borderline resectable disease will be treated with 4 months of FOLFIRINOX prior to resection, followed by chemoradiation and surgery or FOLFIRINOX and surgery, and patients with resectable disease will undergo resection followed by FOLFIRINOX and surgery or gemcitabine/nab-P and surgery.
“The goal is not to compare the two regimens; the goal is to identify the benchmarks that we get with these regimens. In other words, if you’re going to give FOLFIRINOX, what pathologic complete response rate can you expect? What will your R1 resection rate be? With gemcitabine and nab-paclitaxel, the same thing, because if you want to continue to build on these regimens in the neoadjuvant setting you need to know what you’re likely to get so you can make clinical trial assumptions when you add new drugs.
“Once we have these benchmarking data we can really sail in the neoadjuvant setting. It’s a great window-of-opportunity setting for new drugs, because you’re getting serial tissue,” Dr. Tempero said, explaining that in addition to resection of tissue, there is opportunity to get biopsies ahead of time and look at the effects of the drug.
Locally advanced disease
For locally advanced disease, studies have failed to show a benefit of adding radiation after chemotherapy, but radiation oncologists who argue that, “when your therapy gets better, my therapy gets better,” have a valid point, Dr. Tempero said.
For that reason, the Radiation Therapy Oncology group launched a trial to look at gemcitabine/nab-P with and without radiation, but had difficulty with enrollment due to resistance among some physicians who are opposed to radiation in this setting .
“So I don’t know that we will ever answer this question in locally advanced disease. What I can say ... is, in my mind, in locally advanced disease, the most important component is the chemotherapy,” she said.
Metastatic disease
When it comes to trials involving pancreatic cancer patients with metastatic disease, it is important to understand – and to convey to policymakers – that the goal is not only to provide better care in these patients who are at the end of their life, but also to identify strategies that can be used in the adjuvant and neoadjuvant settings, as this is part of the “overall mission of helping patients to feel better and live longer and be cured,” Dr. Tempero said.
One regimen currently used in the metastatic setting is FOLFIRINOX, which was shown in the Prodige 4-ACCORD 11 trial to be superior to gemcitabine monotherapy for survival (hazard ratio, 0.57).
“This is the first time we ever saw a hazard ratio below 0.6 in this disease,” she said, adding that for some patients this means “they can get tremendous benefit, they can come off chemotherapy and have a chemotherapy holiday,” she said.
That said, it’s a tough regimen, she added, explaining that it has dominating toxicities of myelosuppression, diarrhea, and neuropathy that can be irreversible.
Frail patients may not be able to tolerate the regimen, but modifications to the regimen may help. For example, the 5-fluorourasil bolus is often omitted, and doses are sometimes reduced. Chemotherapy holidays can also be of benefit.
Another regimen for the metastatic setting involves the use of nab-P plus gemcitabine, which was shown in a phase III trial to improve survival (HR for death, 0.72).
The results aren’t quite as dramatic as those seen with FOLFIRINOX, but the regimen is slightly easier to manage, Dr. Tempero said, adding: “It’s still not a walk in the park.”
Myelosuppression, arthralgias, and neuropathy still occur, she explained.
Gemcitabine/capecitabine, which has been shown to improve progression-free survival, can also be used, and may be preferable in elderly patients who aren’t fit enough for the other regimens, she said.
“When I select treatment, I really sit down with the patient, and I look at their comorbidities and let them review the toxicities. They decide,” she said, explaining that she provides recommendations based on their concerns and input. “We do have a conversation and we talk about the goals of treatment, we talk about the toxicities.”
Future efforts for metastatic disease should build upon both FOLFIRINOX and gemcitabine/nab-P, she said.
However, because of the difficulty with administering FOLFIRINOX, only two of the 54 open phase I-III trials ongoing in the United States for metastatic disease incorporate the regimen.
Other treatment options include gemcitabine/cisplatin, GTX (gemcitabine/docetaxel/capecitabine), and gemcitabine/erlotinib. The former remains in the NCCN guidelines, primarily for those with hereditary forms of pancreatic cancer, and in particular for those in the DNA repair pathway (BRCA patients, for example).
“We actually have trials now focusing on just BRCA-related pancreatic cancer,” she said, noting that these patients are “exquisitely sensitive to cisplatin and don’t need a harsh regimen like FOLFIRINOX to get the same benefit.
GTX is a very active regimen, although it has never been compared with gemcitabine monotherapy in a randomized trial. However, because of its clear activity it remains in the NCCN guidelines as an option.
Gemcitabine/erlotinib also remains in the guidelines because of a tiny trial that showed a small benefit, but it is not a preferred combination, she said.
Future therapies
Efforts going forward are focusing on finding drugs that inactivate activated RAS, which is “a really big driver” in many cancers, as well as on addressing the microenvironment (such as the desmoplastic stroma that may help encourage invasion of metastases and/or impede drug delivery to the cancer), Dr. Tempero said.
“So there is a lot of interest right now in various forms of immunotherapy or in stromal remodeling so we can see what impact that has on the progression of this disease,” she said, noting that new agents in registration trials include ibrutinib, laparib, PEGPH20, and insulinlike growth factor 1 (IGF-1) inhibitors, and those in planning stages include chemokine (C-C motif) receptor 2 (CCR2) inhibitors and palbociclib.
“And I think we have opportunities in the maintenance setting and in the neoadjuvant setting to do window-of-opportunity trials where we can test new concepts, where we can get pharmacodynamic and biologic data to understand what these new agents are doing,” she said.
Collaborative effort to identify patients at risk
Population-level screening strategies for pancreatic cancer aren’t feasible because of the relatively low incidence of the disease, but efforts are underway to identify and screen high-risk groups.
“We actually have some tests that you could screen with, but they’re not perfect, and with a disease that occurs at the rate that [pancreatic cancer] does, you can’t screen the whole population, because you will find false positives, and you will cause unnecessary procedures more than you’ll find the cancer, Dr. Tempero said during a meeting with press at the NCCN annual conference.
Instead, it is important to identify and screen only those at high risk, she added.
Such a group might include patients with new-onset diabetes who experience weight loss.
New-onset diabetes can be caused by pancreatic cancer, and weight loss with diabetes is unexpected and should raise a red flag, Dr. Temepero explained, adding that an education gap among community physicians means these patients are sometimes cheered for the weight loss instead – and then they end up in the pancreatic disease clinic with metastatic disease 2 years later.
In an effort to better define and characterize this and other high-risk groups, the National Institute for Diabetes and Digestive and Kidney Diseases and the National Cancer Institute are working together to fund a network of institutions that will develop high-risk cohorts and begin deploying screening strategies. The effort is partly in response to the Recalcitrant Cancer Act passed in 2012 to “force more attention on funding pancreatic cancer research through the branches of the NIH,” she explained.
In this particular high-risk group, the institutions will look at the character of diabetes and the clinical correlates with pancreatic cancer.
“Once we hone in on these, we can use those – what we hope are – early-detection biomarkers, and if those are positive, then we would ask the patient to have a CT scan to look for pancreatic cancer,” she said.
Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.
ORLANDO – Overall cancer death rates are dropping dramatically, but pancreatic cancer mortality remains high.
“By 2020 we expect [pancreatic cancer] to be the second most common cause of cancer-related death, exceeded only by lung cancer, and if lung cancer deaths continue to fall – which we expect that they will – it will be the most common cause of cancer-related death,” Margaret A. Tempero, MD, said at the annual conference of the National Comprehensive Cancer Network.
Further, as the population ages there will be an increasing number of patients presenting with pancreatic cancer, said Dr. Tempero of the University of California, San Francisco.
Currently, 80% of pancreatic cancer patients are diagnosed with disease that is not amenable to resection, and 80% of those who have resection and adjuvant therapy experience relapse. The overall survival rate is only about 9%.
“This is really, really an aggressive malignancy,” Dr. Tempero said, noting that the survival among those with metastases who do not receive treatment is only about 3 months.
There are no early symptoms that direct attention to the pancreas. Additionally, some patients experience very early invasion and metastases; in fact, up to two-thirds of patients with lesions only 1 cm in size will already have lymph node metastasis, she said.
The disease tends to be chemoresistant, although this may be changing with treatment advances, but it is characterized by “a lot of desmoplastic stroma, so there’s a lot of microenvironment that’s perturbed around the malignancy,” making it difficult for drugs to permeate the stroma.
“That’s something we’re actively working on – ways that we can actually change the stroma so that we can get more drug into the cancer,” she said.
Another challenge is the disease’s “habit of elaborating a lot of cytokines that disable the person with the disease,” which can lead to frailty that makes it difficult to deliver potentially effective therapies that are well tolerated in patients with other types of cancer, she noted.
An important question is whether pancreatic cancer is diagnosed too late or metastasizes too early, and there is evidence to support both possibilities.
“Either way ... we need to work on better treatment,” she said.
Resectable/borderline resectable disease
One noteworthy recent advance for patients with resectable/borderline resectable disease is the addition of capecitabine to gemcitabine for adjuvant therapy. In the ESPAC 4 study published in March in the Lancet, the combination of gemcitabine and capecitabine showed a clear benefit over gemcitabine alone.
“So that has now entered [the NCCN] guidelines as an important option for adjuvant therapy,” said Dr. Tempero, chair of the NCCN pancreatic cancer guidelines panel.
Ongoing trials are also looking at the FOLFIRINOX (irinotecan plus 5-fluorouracil plus leucovorin plus oxaliplatin) and gemcitabine/nanoparticle albumin-bound paclitaxel (nab-P) regimens in the adjuvant setting. These have previously shown some efficacy in the metastatic setting.
“So we really wanted to get these therapies into the adjuvant setting as soon as we could,” she said.
In the ACCORD trial, FOLFIRINOX is being compared with gemcitabine in the postoperative adjuvant setting, and the APACT trial comparing gemcitabine/nab-P to gemcitabine monotherapy completed accrual last year.
“I’m pretty sure that we’ll have enough events on the APACT study by the end of this year, and hopefully we can present that data in the spring. I’m hoping it will be a positive trial for us,” she said.
Neoadjuvant therapy – a successful strategy used in many other malignancies – is also being looked at for pancreatic cancer.
A pilot study (A021101) completed last year suggested that chemotherapy (FOLFIRINOX for 2 months) and chemoradiation (capecitabine and radiation at 50.4 Gy) followed by surgical resection and adjuvant chemotherapy (gemcitabine for 2 months) provided some benefit in patients with borderline resectable pancreatic cancer. This trial led to another ongoing study (S1505) in which patients with borderline resectable disease will be treated with 4 months of FOLFIRINOX prior to resection, followed by chemoradiation and surgery or FOLFIRINOX and surgery, and patients with resectable disease will undergo resection followed by FOLFIRINOX and surgery or gemcitabine/nab-P and surgery.
“The goal is not to compare the two regimens; the goal is to identify the benchmarks that we get with these regimens. In other words, if you’re going to give FOLFIRINOX, what pathologic complete response rate can you expect? What will your R1 resection rate be? With gemcitabine and nab-paclitaxel, the same thing, because if you want to continue to build on these regimens in the neoadjuvant setting you need to know what you’re likely to get so you can make clinical trial assumptions when you add new drugs.
“Once we have these benchmarking data we can really sail in the neoadjuvant setting. It’s a great window-of-opportunity setting for new drugs, because you’re getting serial tissue,” Dr. Tempero said, explaining that in addition to resection of tissue, there is opportunity to get biopsies ahead of time and look at the effects of the drug.
Locally advanced disease
For locally advanced disease, studies have failed to show a benefit of adding radiation after chemotherapy, but radiation oncologists who argue that, “when your therapy gets better, my therapy gets better,” have a valid point, Dr. Tempero said.
For that reason, the Radiation Therapy Oncology group launched a trial to look at gemcitabine/nab-P with and without radiation, but had difficulty with enrollment due to resistance among some physicians who are opposed to radiation in this setting .
“So I don’t know that we will ever answer this question in locally advanced disease. What I can say ... is, in my mind, in locally advanced disease, the most important component is the chemotherapy,” she said.
Metastatic disease
When it comes to trials involving pancreatic cancer patients with metastatic disease, it is important to understand – and to convey to policymakers – that the goal is not only to provide better care in these patients who are at the end of their life, but also to identify strategies that can be used in the adjuvant and neoadjuvant settings, as this is part of the “overall mission of helping patients to feel better and live longer and be cured,” Dr. Tempero said.
One regimen currently used in the metastatic setting is FOLFIRINOX, which was shown in the Prodige 4-ACCORD 11 trial to be superior to gemcitabine monotherapy for survival (hazard ratio, 0.57).
“This is the first time we ever saw a hazard ratio below 0.6 in this disease,” she said, adding that for some patients this means “they can get tremendous benefit, they can come off chemotherapy and have a chemotherapy holiday,” she said.
That said, it’s a tough regimen, she added, explaining that it has dominating toxicities of myelosuppression, diarrhea, and neuropathy that can be irreversible.
Frail patients may not be able to tolerate the regimen, but modifications to the regimen may help. For example, the 5-fluorourasil bolus is often omitted, and doses are sometimes reduced. Chemotherapy holidays can also be of benefit.
Another regimen for the metastatic setting involves the use of nab-P plus gemcitabine, which was shown in a phase III trial to improve survival (HR for death, 0.72).
The results aren’t quite as dramatic as those seen with FOLFIRINOX, but the regimen is slightly easier to manage, Dr. Tempero said, adding: “It’s still not a walk in the park.”
Myelosuppression, arthralgias, and neuropathy still occur, she explained.
Gemcitabine/capecitabine, which has been shown to improve progression-free survival, can also be used, and may be preferable in elderly patients who aren’t fit enough for the other regimens, she said.
“When I select treatment, I really sit down with the patient, and I look at their comorbidities and let them review the toxicities. They decide,” she said, explaining that she provides recommendations based on their concerns and input. “We do have a conversation and we talk about the goals of treatment, we talk about the toxicities.”
Future efforts for metastatic disease should build upon both FOLFIRINOX and gemcitabine/nab-P, she said.
However, because of the difficulty with administering FOLFIRINOX, only two of the 54 open phase I-III trials ongoing in the United States for metastatic disease incorporate the regimen.
Other treatment options include gemcitabine/cisplatin, GTX (gemcitabine/docetaxel/capecitabine), and gemcitabine/erlotinib. The former remains in the NCCN guidelines, primarily for those with hereditary forms of pancreatic cancer, and in particular for those in the DNA repair pathway (BRCA patients, for example).
“We actually have trials now focusing on just BRCA-related pancreatic cancer,” she said, noting that these patients are “exquisitely sensitive to cisplatin and don’t need a harsh regimen like FOLFIRINOX to get the same benefit.
GTX is a very active regimen, although it has never been compared with gemcitabine monotherapy in a randomized trial. However, because of its clear activity it remains in the NCCN guidelines as an option.
Gemcitabine/erlotinib also remains in the guidelines because of a tiny trial that showed a small benefit, but it is not a preferred combination, she said.
Future therapies
Efforts going forward are focusing on finding drugs that inactivate activated RAS, which is “a really big driver” in many cancers, as well as on addressing the microenvironment (such as the desmoplastic stroma that may help encourage invasion of metastases and/or impede drug delivery to the cancer), Dr. Tempero said.
“So there is a lot of interest right now in various forms of immunotherapy or in stromal remodeling so we can see what impact that has on the progression of this disease,” she said, noting that new agents in registration trials include ibrutinib, laparib, PEGPH20, and insulinlike growth factor 1 (IGF-1) inhibitors, and those in planning stages include chemokine (C-C motif) receptor 2 (CCR2) inhibitors and palbociclib.
“And I think we have opportunities in the maintenance setting and in the neoadjuvant setting to do window-of-opportunity trials where we can test new concepts, where we can get pharmacodynamic and biologic data to understand what these new agents are doing,” she said.
Collaborative effort to identify patients at risk
Population-level screening strategies for pancreatic cancer aren’t feasible because of the relatively low incidence of the disease, but efforts are underway to identify and screen high-risk groups.
“We actually have some tests that you could screen with, but they’re not perfect, and with a disease that occurs at the rate that [pancreatic cancer] does, you can’t screen the whole population, because you will find false positives, and you will cause unnecessary procedures more than you’ll find the cancer, Dr. Tempero said during a meeting with press at the NCCN annual conference.
Instead, it is important to identify and screen only those at high risk, she added.
Such a group might include patients with new-onset diabetes who experience weight loss.
New-onset diabetes can be caused by pancreatic cancer, and weight loss with diabetes is unexpected and should raise a red flag, Dr. Temepero explained, adding that an education gap among community physicians means these patients are sometimes cheered for the weight loss instead – and then they end up in the pancreatic disease clinic with metastatic disease 2 years later.
In an effort to better define and characterize this and other high-risk groups, the National Institute for Diabetes and Digestive and Kidney Diseases and the National Cancer Institute are working together to fund a network of institutions that will develop high-risk cohorts and begin deploying screening strategies. The effort is partly in response to the Recalcitrant Cancer Act passed in 2012 to “force more attention on funding pancreatic cancer research through the branches of the NIH,” she explained.
In this particular high-risk group, the institutions will look at the character of diabetes and the clinical correlates with pancreatic cancer.
“Once we hone in on these, we can use those – what we hope are – early-detection biomarkers, and if those are positive, then we would ask the patient to have a CT scan to look for pancreatic cancer,” she said.
Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.
ORLANDO – Overall cancer death rates are dropping dramatically, but pancreatic cancer mortality remains high.
“By 2020 we expect [pancreatic cancer] to be the second most common cause of cancer-related death, exceeded only by lung cancer, and if lung cancer deaths continue to fall – which we expect that they will – it will be the most common cause of cancer-related death,” Margaret A. Tempero, MD, said at the annual conference of the National Comprehensive Cancer Network.
Further, as the population ages there will be an increasing number of patients presenting with pancreatic cancer, said Dr. Tempero of the University of California, San Francisco.
Currently, 80% of pancreatic cancer patients are diagnosed with disease that is not amenable to resection, and 80% of those who have resection and adjuvant therapy experience relapse. The overall survival rate is only about 9%.
“This is really, really an aggressive malignancy,” Dr. Tempero said, noting that the survival among those with metastases who do not receive treatment is only about 3 months.
There are no early symptoms that direct attention to the pancreas. Additionally, some patients experience very early invasion and metastases; in fact, up to two-thirds of patients with lesions only 1 cm in size will already have lymph node metastasis, she said.
The disease tends to be chemoresistant, although this may be changing with treatment advances, but it is characterized by “a lot of desmoplastic stroma, so there’s a lot of microenvironment that’s perturbed around the malignancy,” making it difficult for drugs to permeate the stroma.
“That’s something we’re actively working on – ways that we can actually change the stroma so that we can get more drug into the cancer,” she said.
Another challenge is the disease’s “habit of elaborating a lot of cytokines that disable the person with the disease,” which can lead to frailty that makes it difficult to deliver potentially effective therapies that are well tolerated in patients with other types of cancer, she noted.
An important question is whether pancreatic cancer is diagnosed too late or metastasizes too early, and there is evidence to support both possibilities.
“Either way ... we need to work on better treatment,” she said.
Resectable/borderline resectable disease
One noteworthy recent advance for patients with resectable/borderline resectable disease is the addition of capecitabine to gemcitabine for adjuvant therapy. In the ESPAC 4 study published in March in the Lancet, the combination of gemcitabine and capecitabine showed a clear benefit over gemcitabine alone.
“So that has now entered [the NCCN] guidelines as an important option for adjuvant therapy,” said Dr. Tempero, chair of the NCCN pancreatic cancer guidelines panel.
Ongoing trials are also looking at the FOLFIRINOX (irinotecan plus 5-fluorouracil plus leucovorin plus oxaliplatin) and gemcitabine/nanoparticle albumin-bound paclitaxel (nab-P) regimens in the adjuvant setting. These have previously shown some efficacy in the metastatic setting.
“So we really wanted to get these therapies into the adjuvant setting as soon as we could,” she said.
In the ACCORD trial, FOLFIRINOX is being compared with gemcitabine in the postoperative adjuvant setting, and the APACT trial comparing gemcitabine/nab-P to gemcitabine monotherapy completed accrual last year.
“I’m pretty sure that we’ll have enough events on the APACT study by the end of this year, and hopefully we can present that data in the spring. I’m hoping it will be a positive trial for us,” she said.
Neoadjuvant therapy – a successful strategy used in many other malignancies – is also being looked at for pancreatic cancer.
A pilot study (A021101) completed last year suggested that chemotherapy (FOLFIRINOX for 2 months) and chemoradiation (capecitabine and radiation at 50.4 Gy) followed by surgical resection and adjuvant chemotherapy (gemcitabine for 2 months) provided some benefit in patients with borderline resectable pancreatic cancer. This trial led to another ongoing study (S1505) in which patients with borderline resectable disease will be treated with 4 months of FOLFIRINOX prior to resection, followed by chemoradiation and surgery or FOLFIRINOX and surgery, and patients with resectable disease will undergo resection followed by FOLFIRINOX and surgery or gemcitabine/nab-P and surgery.
“The goal is not to compare the two regimens; the goal is to identify the benchmarks that we get with these regimens. In other words, if you’re going to give FOLFIRINOX, what pathologic complete response rate can you expect? What will your R1 resection rate be? With gemcitabine and nab-paclitaxel, the same thing, because if you want to continue to build on these regimens in the neoadjuvant setting you need to know what you’re likely to get so you can make clinical trial assumptions when you add new drugs.
“Once we have these benchmarking data we can really sail in the neoadjuvant setting. It’s a great window-of-opportunity setting for new drugs, because you’re getting serial tissue,” Dr. Tempero said, explaining that in addition to resection of tissue, there is opportunity to get biopsies ahead of time and look at the effects of the drug.
Locally advanced disease
For locally advanced disease, studies have failed to show a benefit of adding radiation after chemotherapy, but radiation oncologists who argue that, “when your therapy gets better, my therapy gets better,” have a valid point, Dr. Tempero said.
For that reason, the Radiation Therapy Oncology group launched a trial to look at gemcitabine/nab-P with and without radiation, but had difficulty with enrollment due to resistance among some physicians who are opposed to radiation in this setting .
“So I don’t know that we will ever answer this question in locally advanced disease. What I can say ... is, in my mind, in locally advanced disease, the most important component is the chemotherapy,” she said.
Metastatic disease
When it comes to trials involving pancreatic cancer patients with metastatic disease, it is important to understand – and to convey to policymakers – that the goal is not only to provide better care in these patients who are at the end of their life, but also to identify strategies that can be used in the adjuvant and neoadjuvant settings, as this is part of the “overall mission of helping patients to feel better and live longer and be cured,” Dr. Tempero said.
One regimen currently used in the metastatic setting is FOLFIRINOX, which was shown in the Prodige 4-ACCORD 11 trial to be superior to gemcitabine monotherapy for survival (hazard ratio, 0.57).
“This is the first time we ever saw a hazard ratio below 0.6 in this disease,” she said, adding that for some patients this means “they can get tremendous benefit, they can come off chemotherapy and have a chemotherapy holiday,” she said.
That said, it’s a tough regimen, she added, explaining that it has dominating toxicities of myelosuppression, diarrhea, and neuropathy that can be irreversible.
Frail patients may not be able to tolerate the regimen, but modifications to the regimen may help. For example, the 5-fluorourasil bolus is often omitted, and doses are sometimes reduced. Chemotherapy holidays can also be of benefit.
Another regimen for the metastatic setting involves the use of nab-P plus gemcitabine, which was shown in a phase III trial to improve survival (HR for death, 0.72).
The results aren’t quite as dramatic as those seen with FOLFIRINOX, but the regimen is slightly easier to manage, Dr. Tempero said, adding: “It’s still not a walk in the park.”
Myelosuppression, arthralgias, and neuropathy still occur, she explained.
Gemcitabine/capecitabine, which has been shown to improve progression-free survival, can also be used, and may be preferable in elderly patients who aren’t fit enough for the other regimens, she said.
“When I select treatment, I really sit down with the patient, and I look at their comorbidities and let them review the toxicities. They decide,” she said, explaining that she provides recommendations based on their concerns and input. “We do have a conversation and we talk about the goals of treatment, we talk about the toxicities.”
Future efforts for metastatic disease should build upon both FOLFIRINOX and gemcitabine/nab-P, she said.
However, because of the difficulty with administering FOLFIRINOX, only two of the 54 open phase I-III trials ongoing in the United States for metastatic disease incorporate the regimen.
Other treatment options include gemcitabine/cisplatin, GTX (gemcitabine/docetaxel/capecitabine), and gemcitabine/erlotinib. The former remains in the NCCN guidelines, primarily for those with hereditary forms of pancreatic cancer, and in particular for those in the DNA repair pathway (BRCA patients, for example).
“We actually have trials now focusing on just BRCA-related pancreatic cancer,” she said, noting that these patients are “exquisitely sensitive to cisplatin and don’t need a harsh regimen like FOLFIRINOX to get the same benefit.
GTX is a very active regimen, although it has never been compared with gemcitabine monotherapy in a randomized trial. However, because of its clear activity it remains in the NCCN guidelines as an option.
Gemcitabine/erlotinib also remains in the guidelines because of a tiny trial that showed a small benefit, but it is not a preferred combination, she said.
Future therapies
Efforts going forward are focusing on finding drugs that inactivate activated RAS, which is “a really big driver” in many cancers, as well as on addressing the microenvironment (such as the desmoplastic stroma that may help encourage invasion of metastases and/or impede drug delivery to the cancer), Dr. Tempero said.
“So there is a lot of interest right now in various forms of immunotherapy or in stromal remodeling so we can see what impact that has on the progression of this disease,” she said, noting that new agents in registration trials include ibrutinib, laparib, PEGPH20, and insulinlike growth factor 1 (IGF-1) inhibitors, and those in planning stages include chemokine (C-C motif) receptor 2 (CCR2) inhibitors and palbociclib.
“And I think we have opportunities in the maintenance setting and in the neoadjuvant setting to do window-of-opportunity trials where we can test new concepts, where we can get pharmacodynamic and biologic data to understand what these new agents are doing,” she said.
Collaborative effort to identify patients at risk
Population-level screening strategies for pancreatic cancer aren’t feasible because of the relatively low incidence of the disease, but efforts are underway to identify and screen high-risk groups.
“We actually have some tests that you could screen with, but they’re not perfect, and with a disease that occurs at the rate that [pancreatic cancer] does, you can’t screen the whole population, because you will find false positives, and you will cause unnecessary procedures more than you’ll find the cancer, Dr. Tempero said during a meeting with press at the NCCN annual conference.
Instead, it is important to identify and screen only those at high risk, she added.
Such a group might include patients with new-onset diabetes who experience weight loss.
New-onset diabetes can be caused by pancreatic cancer, and weight loss with diabetes is unexpected and should raise a red flag, Dr. Temepero explained, adding that an education gap among community physicians means these patients are sometimes cheered for the weight loss instead – and then they end up in the pancreatic disease clinic with metastatic disease 2 years later.
In an effort to better define and characterize this and other high-risk groups, the National Institute for Diabetes and Digestive and Kidney Diseases and the National Cancer Institute are working together to fund a network of institutions that will develop high-risk cohorts and begin deploying screening strategies. The effort is partly in response to the Recalcitrant Cancer Act passed in 2012 to “force more attention on funding pancreatic cancer research through the branches of the NIH,” she explained.
In this particular high-risk group, the institutions will look at the character of diabetes and the clinical correlates with pancreatic cancer.
“Once we hone in on these, we can use those – what we hope are – early-detection biomarkers, and if those are positive, then we would ask the patient to have a CT scan to look for pancreatic cancer,” she said.
Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.
AT THE NCCN ANNUAL CONFERENCE
Key clinical point:
Disclosures: Dr. Tempero reported serving as a scientific advisor and/or receiving grant/research support, consulting fees, and/or honoraria from Celgene Corporation, Champion Oncology, Cornerstone Pharmaceuticals, Eli Lilly, EMD Serono, Gilead Sciences, Halozyme Therapeutics, MCS Biotech Resources, NeoHealth, Novocure, Opsona Therapeutics, Pfizer, Portola Pharmaceuticals, and Threshold Pharmaceuticals.