User login
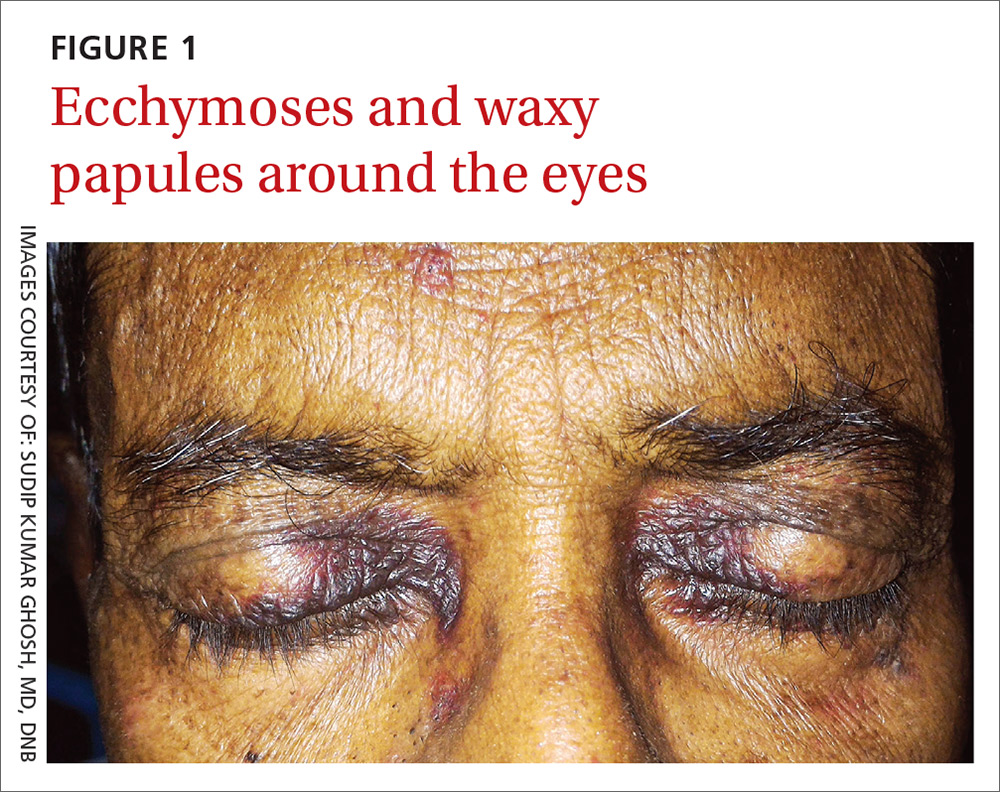
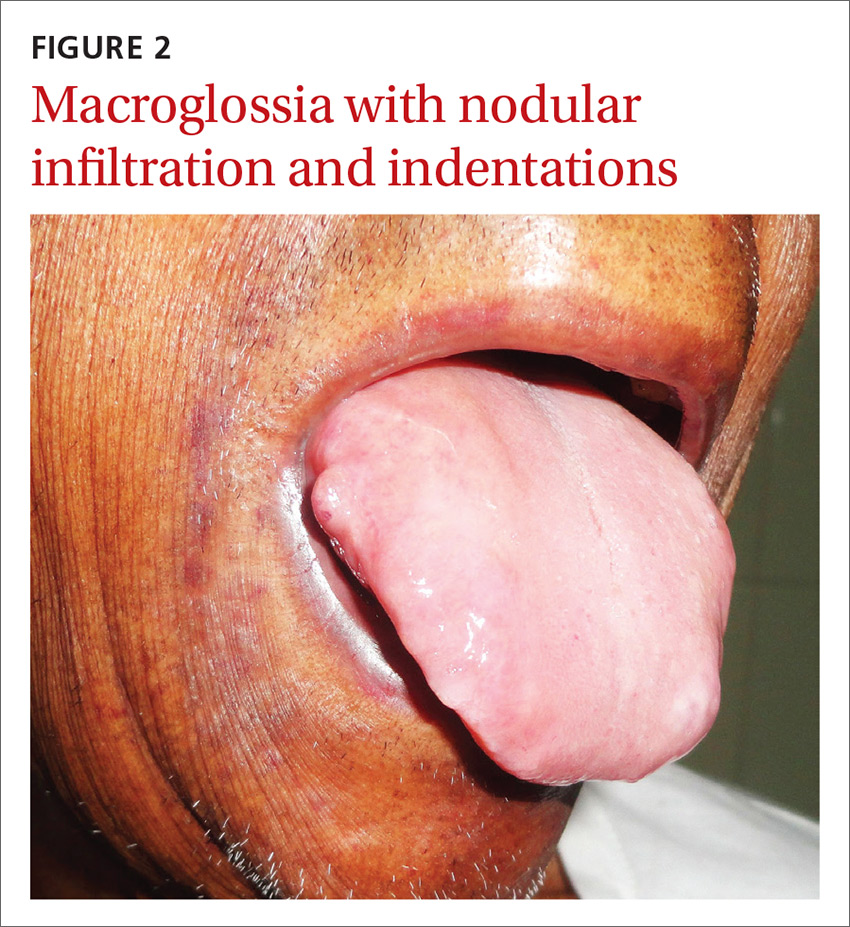
A 54-year-old man presented at our facility with a 3-month history of exertional breathlessness and purple blotches around his eyes. Examination revealed bilateral periorbital and perioral ecchymosis, purpuric spots along his waist, and waxy papules on his eyelids (FIGURE 1). In addition, the patient had macroglossia with nodular infiltration and irregular indentations at the lateral margin of his tongue (FIGURE 2).
The patient also had a raised jugular venous pressure and prominent atrial and ventricular waves. Further examination revealed a fourth heart sound over the left ventricular apex, as well as bilateral basal rales. All other systems were normal except for mild hepatomegaly.
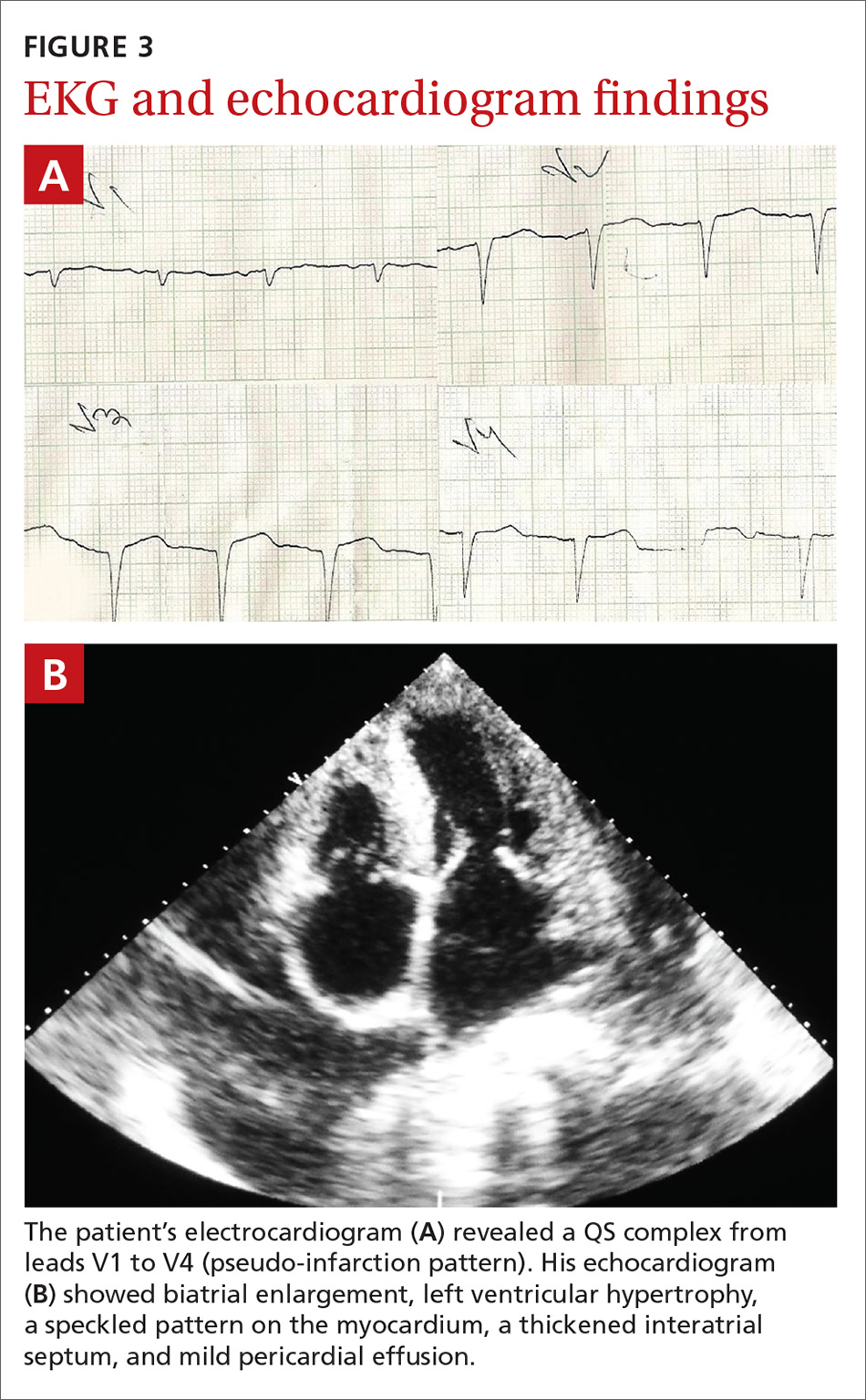
Routine hematologic and biochemical lab work was unremarkable. X-rays of the spine and skull were normal, but a chest x-ray showed mild cardiomegaly. An electrocardiogram (EKG) showed a QS complex from leads V1 to V4 (a pseudo-infarction pattern; FIGURE 3A). An echocardiogram showed biatrial enlargement, left ventricular hypertrophy with a left ventricular ejection fraction of 48%, a speckled pattern on the myocardium, a thickened interatrial septum, and mild pericardial effusion (FIGURE 3B).
A color Doppler revealed mild mitral and tricuspid regurgitation with a restrictive pattern of mitral valve flow. Serum protein electrophoresis was normal.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Primary systemic amyloidosis
A diagnosis of primary systemic amyloidosis was confirmed with histopathologic examination of the abdominal fat pad using Congo red stain. Clinical, imaging, and laboratory features supported this diagnosis.
Primary systemic amyloidosis (also known as light-chain amyloidosis) is the most common type of systemic amyloidosis, affecting an estimated 5 to 12 million people per year.1,2 It occurs when there is a buildup of the abnormal protein amyloid. Organs that may be affected include the heart, kidneys, skin, nerves, and liver. There are no clear environmental, racial, or genetic risk factors for this condition.
With primary systemic amyloidosis, the ecchymosis present around the eyes may also appear elsewhere on the body (pinch purpura). Other symptoms may include macroglossia; sensory and autonomic neuropathy; and concomitant renal, cardiac, and hepatic involvement. In elderly patients with these symptoms, myeloma-associated systemic amyloidosis should be ruled out.2 Histopathologic examination of the abdominal fat pad or rectum is usually diagnostic.
Systemic amyloidosis and the heart
In patients with symptoms of congestive heart failure, a finding of thick heart walls on echocardiogram may indicate cardiac amyloidosis, particularly if there is no other underlying heart disease that could explain such findings. An even stronger indicator is the additional finding of low-voltage complexes on EKG.3
Periorbital ecchymosis can be a sign of many conditions
Bilateral periorbital ecchymosis, also known as “raccoon eyes,” was an important clinical clue to the diagnosis in our patient, but multiple conditions should be considered when raccoon eyes are present.
Basal skull fracture occurs with a history of trauma. Clinical and radiologic signs of injuries can usually be found in other areas of the body.6
Periorbital cellulitis presents with unilateral erythematous periorbital swelling. A rapid increase in the patient’s temperature and swelling of tissue may occur. Movement of the extraocular muscles and visual acuity are usually normal.7
Blood dyscrasias usually involve a history of external bleeding.7 A thorough laboratory evaluation, including a complete blood count, platelet function tests, and a blood coagulation profile, is usually sufficient to exclude these cases.
A variety of treatment options
Clinicians have used angiotensin-converting enzyme inhibitors, long-acting nitrates, vasodilators, and diuretics to treat cardiac amyloidosis with varying results. For patients with atrial fibrillation (AF), ibutilide and amiodarone are useful antiarrhythmic drugs.3,8 In addition, experts recommend anticoagulation therapy with warfarin, dabigatran, or rivaroxaban for patients with AF because of the high risk of stroke.3,8 Symptomatic bradycardia and high-grade conduction-system disease usually require pacemaker implantation.
A guarded prognosis. The prognosis for patients with primary systemic amyloidosis is usually poor. Cardiac failure and renal failure are the major causes of death. The median survival time is 13 months, and only 5% of patients survive longer than 10 years.4,5
Our patient was prescribed furosemide 40 mg/d, ramipril 1.25 mg/d, and spironolactone 25 mg/d. Within a couple weeks, his symptoms improved. However, 3 months after being diagnosed, the patient succumbed to heart failure.
CORRESPONDENCE
Sudip Kumar Ghosh, MD, DNB, Department of Dermatology, Venereology, and Leprosy, R. G. Kar Medical College, 1, Khudiram Bose Sarani, Kolkata, West Bengal 700004, India; dr_skghosh@yahoo.co.in.
1. Gertz MA. The classification and typing of amyloid deposits. Am J Clin Pathol. 2004;121:787-789.
2. Sanchorawala V. Light-chain (AL) amyloidosis: diagnosis and treatment. Clin J Am Soc Nephrol. 2006;1:1331-1341.
3. Quarta CC, Kruger JL, Falk RH. Cardiac amyloidosis. Circulation. 2012;126:e178-e182.
4. Kyle RA, Gertz MA, Greipp PR, et al. A trial of three regimens for primary amyloidosis: colchicine alone, melphalan and prednisone, and melphalan, prednisone, and colchicine. N Engl J Med. 1997;336:1202-1207.
5. Kyle RA, Gertz MA, Greipp PR, et al. Long-term survival (10 years or more) in 30 patients with primary amyloidosis. Blood. 1999;93:1062-1066.
6. Somasundaram A, Laxton AW, Perrin RG. The clinical features of periorbital ecchymosis in a series of trauma patients. Injury. 2014;45:203-205.
7. Ghosh SK, Dutta A, Basu M. Raccoon eyes in a case of metastatic neuroblastoma. Indian J Dermatol Venereol Leprol. 2012;78:740-741.
8. Hassan W, Al-Sergani H, Mourad W, et al. Amyloid heart disease. New frontiers and insights in pathophysiology, diagnosis, and management. Tex Heart Inst J. 2005;32:178-184.
A 54-year-old man presented at our facility with a 3-month history of exertional breathlessness and purple blotches around his eyes. Examination revealed bilateral periorbital and perioral ecchymosis, purpuric spots along his waist, and waxy papules on his eyelids (FIGURE 1). In addition, the patient had macroglossia with nodular infiltration and irregular indentations at the lateral margin of his tongue (FIGURE 2).
The patient also had a raised jugular venous pressure and prominent atrial and ventricular waves. Further examination revealed a fourth heart sound over the left ventricular apex, as well as bilateral basal rales. All other systems were normal except for mild hepatomegaly.
Routine hematologic and biochemical lab work was unremarkable. X-rays of the spine and skull were normal, but a chest x-ray showed mild cardiomegaly. An electrocardiogram (EKG) showed a QS complex from leads V1 to V4 (a pseudo-infarction pattern; FIGURE 3A). An echocardiogram showed biatrial enlargement, left ventricular hypertrophy with a left ventricular ejection fraction of 48%, a speckled pattern on the myocardium, a thickened interatrial septum, and mild pericardial effusion (FIGURE 3B).
A color Doppler revealed mild mitral and tricuspid regurgitation with a restrictive pattern of mitral valve flow. Serum protein electrophoresis was normal.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Primary systemic amyloidosis
A diagnosis of primary systemic amyloidosis was confirmed with histopathologic examination of the abdominal fat pad using Congo red stain. Clinical, imaging, and laboratory features supported this diagnosis.
Primary systemic amyloidosis (also known as light-chain amyloidosis) is the most common type of systemic amyloidosis, affecting an estimated 5 to 12 million people per year.1,2 It occurs when there is a buildup of the abnormal protein amyloid. Organs that may be affected include the heart, kidneys, skin, nerves, and liver. There are no clear environmental, racial, or genetic risk factors for this condition.
With primary systemic amyloidosis, the ecchymosis present around the eyes may also appear elsewhere on the body (pinch purpura). Other symptoms may include macroglossia; sensory and autonomic neuropathy; and concomitant renal, cardiac, and hepatic involvement. In elderly patients with these symptoms, myeloma-associated systemic amyloidosis should be ruled out.2 Histopathologic examination of the abdominal fat pad or rectum is usually diagnostic.
Systemic amyloidosis and the heart
In patients with symptoms of congestive heart failure, a finding of thick heart walls on echocardiogram may indicate cardiac amyloidosis, particularly if there is no other underlying heart disease that could explain such findings. An even stronger indicator is the additional finding of low-voltage complexes on EKG.3
Periorbital ecchymosis can be a sign of many conditions
Bilateral periorbital ecchymosis, also known as “raccoon eyes,” was an important clinical clue to the diagnosis in our patient, but multiple conditions should be considered when raccoon eyes are present.
Basal skull fracture occurs with a history of trauma. Clinical and radiologic signs of injuries can usually be found in other areas of the body.6
Periorbital cellulitis presents with unilateral erythematous periorbital swelling. A rapid increase in the patient’s temperature and swelling of tissue may occur. Movement of the extraocular muscles and visual acuity are usually normal.7
Blood dyscrasias usually involve a history of external bleeding.7 A thorough laboratory evaluation, including a complete blood count, platelet function tests, and a blood coagulation profile, is usually sufficient to exclude these cases.
A variety of treatment options
Clinicians have used angiotensin-converting enzyme inhibitors, long-acting nitrates, vasodilators, and diuretics to treat cardiac amyloidosis with varying results. For patients with atrial fibrillation (AF), ibutilide and amiodarone are useful antiarrhythmic drugs.3,8 In addition, experts recommend anticoagulation therapy with warfarin, dabigatran, or rivaroxaban for patients with AF because of the high risk of stroke.3,8 Symptomatic bradycardia and high-grade conduction-system disease usually require pacemaker implantation.
A guarded prognosis. The prognosis for patients with primary systemic amyloidosis is usually poor. Cardiac failure and renal failure are the major causes of death. The median survival time is 13 months, and only 5% of patients survive longer than 10 years.4,5
Our patient was prescribed furosemide 40 mg/d, ramipril 1.25 mg/d, and spironolactone 25 mg/d. Within a couple weeks, his symptoms improved. However, 3 months after being diagnosed, the patient succumbed to heart failure.
CORRESPONDENCE
Sudip Kumar Ghosh, MD, DNB, Department of Dermatology, Venereology, and Leprosy, R. G. Kar Medical College, 1, Khudiram Bose Sarani, Kolkata, West Bengal 700004, India; dr_skghosh@yahoo.co.in.
A 54-year-old man presented at our facility with a 3-month history of exertional breathlessness and purple blotches around his eyes. Examination revealed bilateral periorbital and perioral ecchymosis, purpuric spots along his waist, and waxy papules on his eyelids (FIGURE 1). In addition, the patient had macroglossia with nodular infiltration and irregular indentations at the lateral margin of his tongue (FIGURE 2).
The patient also had a raised jugular venous pressure and prominent atrial and ventricular waves. Further examination revealed a fourth heart sound over the left ventricular apex, as well as bilateral basal rales. All other systems were normal except for mild hepatomegaly.
Routine hematologic and biochemical lab work was unremarkable. X-rays of the spine and skull were normal, but a chest x-ray showed mild cardiomegaly. An electrocardiogram (EKG) showed a QS complex from leads V1 to V4 (a pseudo-infarction pattern; FIGURE 3A). An echocardiogram showed biatrial enlargement, left ventricular hypertrophy with a left ventricular ejection fraction of 48%, a speckled pattern on the myocardium, a thickened interatrial septum, and mild pericardial effusion (FIGURE 3B).
A color Doppler revealed mild mitral and tricuspid regurgitation with a restrictive pattern of mitral valve flow. Serum protein electrophoresis was normal.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Primary systemic amyloidosis
A diagnosis of primary systemic amyloidosis was confirmed with histopathologic examination of the abdominal fat pad using Congo red stain. Clinical, imaging, and laboratory features supported this diagnosis.
Primary systemic amyloidosis (also known as light-chain amyloidosis) is the most common type of systemic amyloidosis, affecting an estimated 5 to 12 million people per year.1,2 It occurs when there is a buildup of the abnormal protein amyloid. Organs that may be affected include the heart, kidneys, skin, nerves, and liver. There are no clear environmental, racial, or genetic risk factors for this condition.
With primary systemic amyloidosis, the ecchymosis present around the eyes may also appear elsewhere on the body (pinch purpura). Other symptoms may include macroglossia; sensory and autonomic neuropathy; and concomitant renal, cardiac, and hepatic involvement. In elderly patients with these symptoms, myeloma-associated systemic amyloidosis should be ruled out.2 Histopathologic examination of the abdominal fat pad or rectum is usually diagnostic.
Systemic amyloidosis and the heart
In patients with symptoms of congestive heart failure, a finding of thick heart walls on echocardiogram may indicate cardiac amyloidosis, particularly if there is no other underlying heart disease that could explain such findings. An even stronger indicator is the additional finding of low-voltage complexes on EKG.3
Periorbital ecchymosis can be a sign of many conditions
Bilateral periorbital ecchymosis, also known as “raccoon eyes,” was an important clinical clue to the diagnosis in our patient, but multiple conditions should be considered when raccoon eyes are present.
Basal skull fracture occurs with a history of trauma. Clinical and radiologic signs of injuries can usually be found in other areas of the body.6
Periorbital cellulitis presents with unilateral erythematous periorbital swelling. A rapid increase in the patient’s temperature and swelling of tissue may occur. Movement of the extraocular muscles and visual acuity are usually normal.7
Blood dyscrasias usually involve a history of external bleeding.7 A thorough laboratory evaluation, including a complete blood count, platelet function tests, and a blood coagulation profile, is usually sufficient to exclude these cases.
A variety of treatment options
Clinicians have used angiotensin-converting enzyme inhibitors, long-acting nitrates, vasodilators, and diuretics to treat cardiac amyloidosis with varying results. For patients with atrial fibrillation (AF), ibutilide and amiodarone are useful antiarrhythmic drugs.3,8 In addition, experts recommend anticoagulation therapy with warfarin, dabigatran, or rivaroxaban for patients with AF because of the high risk of stroke.3,8 Symptomatic bradycardia and high-grade conduction-system disease usually require pacemaker implantation.
A guarded prognosis. The prognosis for patients with primary systemic amyloidosis is usually poor. Cardiac failure and renal failure are the major causes of death. The median survival time is 13 months, and only 5% of patients survive longer than 10 years.4,5
Our patient was prescribed furosemide 40 mg/d, ramipril 1.25 mg/d, and spironolactone 25 mg/d. Within a couple weeks, his symptoms improved. However, 3 months after being diagnosed, the patient succumbed to heart failure.
CORRESPONDENCE
Sudip Kumar Ghosh, MD, DNB, Department of Dermatology, Venereology, and Leprosy, R. G. Kar Medical College, 1, Khudiram Bose Sarani, Kolkata, West Bengal 700004, India; dr_skghosh@yahoo.co.in.
1. Gertz MA. The classification and typing of amyloid deposits. Am J Clin Pathol. 2004;121:787-789.
2. Sanchorawala V. Light-chain (AL) amyloidosis: diagnosis and treatment. Clin J Am Soc Nephrol. 2006;1:1331-1341.
3. Quarta CC, Kruger JL, Falk RH. Cardiac amyloidosis. Circulation. 2012;126:e178-e182.
4. Kyle RA, Gertz MA, Greipp PR, et al. A trial of three regimens for primary amyloidosis: colchicine alone, melphalan and prednisone, and melphalan, prednisone, and colchicine. N Engl J Med. 1997;336:1202-1207.
5. Kyle RA, Gertz MA, Greipp PR, et al. Long-term survival (10 years or more) in 30 patients with primary amyloidosis. Blood. 1999;93:1062-1066.
6. Somasundaram A, Laxton AW, Perrin RG. The clinical features of periorbital ecchymosis in a series of trauma patients. Injury. 2014;45:203-205.
7. Ghosh SK, Dutta A, Basu M. Raccoon eyes in a case of metastatic neuroblastoma. Indian J Dermatol Venereol Leprol. 2012;78:740-741.
8. Hassan W, Al-Sergani H, Mourad W, et al. Amyloid heart disease. New frontiers and insights in pathophysiology, diagnosis, and management. Tex Heart Inst J. 2005;32:178-184.
1. Gertz MA. The classification and typing of amyloid deposits. Am J Clin Pathol. 2004;121:787-789.
2. Sanchorawala V. Light-chain (AL) amyloidosis: diagnosis and treatment. Clin J Am Soc Nephrol. 2006;1:1331-1341.
3. Quarta CC, Kruger JL, Falk RH. Cardiac amyloidosis. Circulation. 2012;126:e178-e182.
4. Kyle RA, Gertz MA, Greipp PR, et al. A trial of three regimens for primary amyloidosis: colchicine alone, melphalan and prednisone, and melphalan, prednisone, and colchicine. N Engl J Med. 1997;336:1202-1207.
5. Kyle RA, Gertz MA, Greipp PR, et al. Long-term survival (10 years or more) in 30 patients with primary amyloidosis. Blood. 1999;93:1062-1066.
6. Somasundaram A, Laxton AW, Perrin RG. The clinical features of periorbital ecchymosis in a series of trauma patients. Injury. 2014;45:203-205.
7. Ghosh SK, Dutta A, Basu M. Raccoon eyes in a case of metastatic neuroblastoma. Indian J Dermatol Venereol Leprol. 2012;78:740-741.
8. Hassan W, Al-Sergani H, Mourad W, et al. Amyloid heart disease. New frontiers and insights in pathophysiology, diagnosis, and management. Tex Heart Inst J. 2005;32:178-184.