User login
Lenalidomide maintenance therapy further improved depth of response in newly diagnosed, transplant-eligible patients with multiple myeloma in the EMN02/HO95 trial, based on the abstract of a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The study results also show that using multiparameter flow cytometry to monitor minimal residual disease (MRD) was predictive of patient outcome. A high-risk cytogenetic profile – defined as having del17, translocation (4;14), or translocation (14;16) – was the most important prognostic factor in MRD-positive patients, according to Stefania Oliva, MD, of the University of Torino [Italy] and her colleagues.
At 3 years, progression-free survival was 50% in MRD-positive patients and 77% in MRD-negative patients (hazard ratio, 2.87; P less than .001). High-risk cytogenetics was the most important risk factor (HR, 9.87; interaction-P = .001). Further, 48% of patients who had MRD before maintenance therapy and had a second evaluation for minimal residual disease after at least 1 year of lenalidomide therapy became MRD negative.
The trial (NCT01208766) participants were no older than age 65 years and received received bortezomib-cyclophosphamide-dexamethasone (VCD) induction therapy, then bortezomib-melphalan-prednisone (VMP) or high-dose melphalan intensification therapy followed by stem cell transplant, and subsequently bortezomib-lenalidomide-dexamethasone (VRD) consolidation therapy or no consolidation therapy, followed by lenalidomide maintenance therapy.
Of 316 patients who were evaluable before maintenance therapy, 18% had International Staging System stage III disease (beta-2 microglobulin of 5.5 mg/L or greater) and 22% had a high-risk cytogenetic profile.
For intensification therapy, 63% had received high-dose melphalan and 37% got VMP; thereafter 51% had received VRD. Nearly two-thirds of the 76% of patients who were MRD negative got high-dose melphalan, with a median follow-up of 30 months from MRD enrollment.
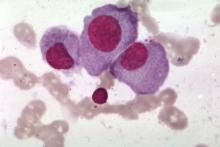
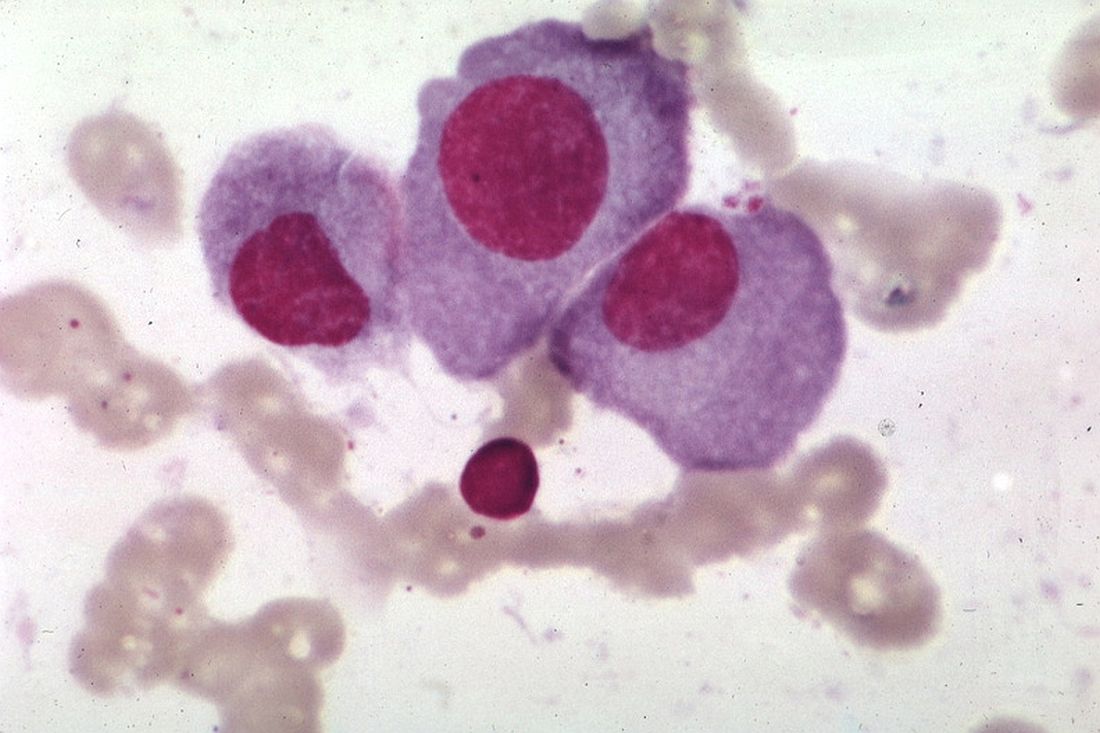
Patients who had at least a very good partial response underwent minimal residual disease evaluation before starting maintenance therapy and then every 6-12 months during maintenance therapy. Multiparameter flow cytometry was performed on bone marrow according to Euroflow-based methods (eight colors, two tubes) with a sensitivity of 10-5, and quality checks were performed to compare sensitivity and to show correlation between protocols.
Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011
mdales@frontlinemedcom.com
On Twitter @maryjodales
Lenalidomide maintenance therapy further improved depth of response in newly diagnosed, transplant-eligible patients with multiple myeloma in the EMN02/HO95 trial, based on the abstract of a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The study results also show that using multiparameter flow cytometry to monitor minimal residual disease (MRD) was predictive of patient outcome. A high-risk cytogenetic profile – defined as having del17, translocation (4;14), or translocation (14;16) – was the most important prognostic factor in MRD-positive patients, according to Stefania Oliva, MD, of the University of Torino [Italy] and her colleagues.
At 3 years, progression-free survival was 50% in MRD-positive patients and 77% in MRD-negative patients (hazard ratio, 2.87; P less than .001). High-risk cytogenetics was the most important risk factor (HR, 9.87; interaction-P = .001). Further, 48% of patients who had MRD before maintenance therapy and had a second evaluation for minimal residual disease after at least 1 year of lenalidomide therapy became MRD negative.
The trial (NCT01208766) participants were no older than age 65 years and received received bortezomib-cyclophosphamide-dexamethasone (VCD) induction therapy, then bortezomib-melphalan-prednisone (VMP) or high-dose melphalan intensification therapy followed by stem cell transplant, and subsequently bortezomib-lenalidomide-dexamethasone (VRD) consolidation therapy or no consolidation therapy, followed by lenalidomide maintenance therapy.
Of 316 patients who were evaluable before maintenance therapy, 18% had International Staging System stage III disease (beta-2 microglobulin of 5.5 mg/L or greater) and 22% had a high-risk cytogenetic profile.
For intensification therapy, 63% had received high-dose melphalan and 37% got VMP; thereafter 51% had received VRD. Nearly two-thirds of the 76% of patients who were MRD negative got high-dose melphalan, with a median follow-up of 30 months from MRD enrollment.
Patients who had at least a very good partial response underwent minimal residual disease evaluation before starting maintenance therapy and then every 6-12 months during maintenance therapy. Multiparameter flow cytometry was performed on bone marrow according to Euroflow-based methods (eight colors, two tubes) with a sensitivity of 10-5, and quality checks were performed to compare sensitivity and to show correlation between protocols.
Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011
mdales@frontlinemedcom.com
On Twitter @maryjodales
Lenalidomide maintenance therapy further improved depth of response in newly diagnosed, transplant-eligible patients with multiple myeloma in the EMN02/HO95 trial, based on the abstract of a poster to be presented at the annual meeting of the American Society of Clinical Oncology.
The study results also show that using multiparameter flow cytometry to monitor minimal residual disease (MRD) was predictive of patient outcome. A high-risk cytogenetic profile – defined as having del17, translocation (4;14), or translocation (14;16) – was the most important prognostic factor in MRD-positive patients, according to Stefania Oliva, MD, of the University of Torino [Italy] and her colleagues.
At 3 years, progression-free survival was 50% in MRD-positive patients and 77% in MRD-negative patients (hazard ratio, 2.87; P less than .001). High-risk cytogenetics was the most important risk factor (HR, 9.87; interaction-P = .001). Further, 48% of patients who had MRD before maintenance therapy and had a second evaluation for minimal residual disease after at least 1 year of lenalidomide therapy became MRD negative.
The trial (NCT01208766) participants were no older than age 65 years and received received bortezomib-cyclophosphamide-dexamethasone (VCD) induction therapy, then bortezomib-melphalan-prednisone (VMP) or high-dose melphalan intensification therapy followed by stem cell transplant, and subsequently bortezomib-lenalidomide-dexamethasone (VRD) consolidation therapy or no consolidation therapy, followed by lenalidomide maintenance therapy.
Of 316 patients who were evaluable before maintenance therapy, 18% had International Staging System stage III disease (beta-2 microglobulin of 5.5 mg/L or greater) and 22% had a high-risk cytogenetic profile.
For intensification therapy, 63% had received high-dose melphalan and 37% got VMP; thereafter 51% had received VRD. Nearly two-thirds of the 76% of patients who were MRD negative got high-dose melphalan, with a median follow-up of 30 months from MRD enrollment.
Patients who had at least a very good partial response underwent minimal residual disease evaluation before starting maintenance therapy and then every 6-12 months during maintenance therapy. Multiparameter flow cytometry was performed on bone marrow according to Euroflow-based methods (eight colors, two tubes) with a sensitivity of 10-5, and quality checks were performed to compare sensitivity and to show correlation between protocols.
Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011
mdales@frontlinemedcom.com
On Twitter @maryjodales
FROM 2017 ASCO ANNUAL MEETING
Key clinical point:
Major finding: 48% of patients who had minimal residual disease before maintenance therapy and had a second evaluation for MRD after at least 1 year of lenalidomide therapy became MRD negative.
Data source: A 3-year study of 316 patients who were evaluable before maintenance therapy in the EMN02/HO95 trial.
Disclosures: Dr. Oliva disclosed receiving honoraria from Celgene and Takeda.
Citation: Minimal residual disease (MRD) monitoring by multiparameter flow cytometry (MFC) in newly diagnosed transplant eligible multiple myeloma (MM) patients: Results from the EMN02/HO95 phase 3 trial. 2017 ASCO annual meeting. Abstract No: 8011