User login
In this age of technological marvels, it is easy to become so reliant on them as to neglect the value of bedside physical signs. Yet these signs provide information that adds no cost, is immediately available, and can be repeated at will.
Few physical findings are as useful but as undervalued as is the estimation of the jugular venous pressure. Unfortunately, many practitioners at many levels of seniority and experience do not measure it correctly, leading to a vicious circle of unreliable information, lack of confidence, and underuse. Another reason for its underuse is that the jugular venous pressure does not correlate precisely with the right atrial pressure, as we will see below.
In this review, we will attempt to clarify physiologic principles and describe technical details. Much of this is simple but, as always, the devil is in the details.
ANATOMIC CONSIDERATIONS
Think of the systemic veins as a soft-walled and mildly distensible reservoir with fingerlike projections, analogous to a partially fluidfilled surgical glove.1 In a semi-upright position, the venous system is partially filled with blood and is collapsed above the level that this blood reaches up to.
Blood is constantly flowing in and out of this reservoir, flowing in by venous return and flowing out by the pumping action of the right side of the heart. The volume in the venous reservoir and hence the pressure are normally maintained by the variability of right ventricular stroke volume in accordance with the Frank-Starling law. Excess volume and pressure indicate failure of this homeostatic mechanism.
The internal jugular veins, being continuous with the superior vena cava, provide a visible measure of the degree to which the systemic venous reservoir is filled, a manometer that reflects the pressure in the right atrium—at least in theory.2 Thus, the vertical height above the right atrium to which they are distended and above which they are in a collapsed state should reflect the right atrial pressure.
(In fact, the jugular venous pressure may underestimate the right atrial pressure, for reasons still not understood. This will be discussed below.)
In a healthy person, the visible jugular veins are fully collapsed when the person is standing and are often distended to a variable degree when the person is supine. Selecting an appropriate intermediate position permits the top of the column (the meniscus) to become visible in the neck between the clavicle and the mandible.
DISCREPANCY BETWEEN JUGULAR VENOUS AND RIGHT ATRIAL PRESSURE
Several reports have indicated that the jugular venous pressure may underestimate the right atrial pressure. Deol et al3 confirmed this, while establishing an excellent correlation between the level of venous collapse (observed on ultrasonography) and the jugular venous pressure. The difference between the right atrial pressure and the jugular venous pressure tended to be greater at higher venous pressures.3
Most people have a valve near the termination of the internal jugular vein, with variable competence. Inhibition of reflux of blood from the superior vena cava into the internal jugular vein by this valve is the most plausible cause of this disparity.4
The failure of the jugular venous pressure to correlate with the right atrial pressure has been cited by some as a reason to doubt the value of a sign that cardiologists have long relied on. How do we reconcile this apparent paradox? Careful review of the literature that has demonstrated this lack of correlation reveals the following:
- When unequal, the jugular venous pressure always underestimates the right atrial pressure.
- The lack of correlation is less evident at lower venous pressures.
This indicates the following:
- In the presence of congestive heart failure, the right atrial pressure is at least as high and perhaps higher than the jugular venous pressure. Hence, if the jugular venous pressure is high, further treatment, especially diuresis, is needed.
- A jugular venous pressure of zero implies a euvolemic state.
Thus, the jugular venous pressure provides excellent guidance when administering diuresis in congestive heart failure. These deductions obviously require the clinical judgment that the elevated right atrial pressure and jugular venous pressure do indeed reflect elevation of pulmonary capillary wedge pressure rather than other conditions discussed later in this article.
WHICH REFERENCE POINT TO USE?
The two points that can be used as references above which the jugular venous pressure is expressed are the center of the right atrium and the sternal angle. While the former may reflect physiology, the latter is preferred, as it is always visible and has the added advantage of being close to the upper limit of normal, which is about 3 cm above this level.
The difference in height between these two reference points has often been quoted as 5 cm, but this is an underestimate in the body positions used in examination.5 Seth et al6 found a mean of 8 cm at 30° elevation, 9.7 cm at 45°, and 9.8 cm at 60°. The difference also varied between patients, being larger in association with smoking, older age, large body mass index, and large anterior-posterior diameter. These factors should be considered when trying to evaluate the significance of a particular jugular venous pressure.
The junction of the midaxillary line and the fourth left intercostal space (“the phlebostatic point”) has been recommended as a reference point by some, as it is level with the mid-right atrium. However, using the phlebostatic point as a reference position is cumbersome and results in a valid measurement only with the patient in the supine position.7
TECHNIQUE IS VITAL
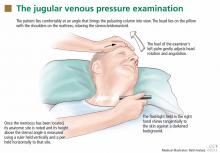
Close adherence to technical details is vital in reliably and reproducibly measuring the pressure in the internal jugular veins (Figure 1).
The right side is usually observed first, as it is the side on which the examiner usually stands. Using the right side also avoids the rare occurrence of external compression of the left brachiocephalic vein.
Head and shoulders
The sternocleidomastoid muscle lies anterior to each internal jugular vein.8 When tense, it impedes good observation. Shortening, and hence relaxing, this muscle permits the meniscus to be observed. Correct positioning is achieved by:
- Placing a folded pillow behind the patient’s head
- Keeping the shoulders on the mattress
- Turning the head away and elevating the jaw, both slightly; this is often best achieved by gentle pressure of the palm of the observer's hand on the patient's forehead.
Degree of head elevation
Although the proper degree of head elevation is sometimes said to be between 30° and 60°, these numbers are approximate. The correct angle is that which brings the venous meniscus into the window of visibility in the neck between the clavicle and mandible.
Lighting
Shining a flashlight tangentially to the skin is often helpful, casting shadows that improve the visibility of vein motion. Dimming the room lighting may further enhance this effect. Directing a light perpendicular to the skin is not helpful.
Also check the external jugular vein
Checking the external jugular vein can help establish that the jugular venous pressure is normal. If the vein is initially collapsed, light finger pressure at the base of the neck will distend it. If the distention rapidly clears after release of this pressure, the jugular venous pressure is not elevated. However, if external jugular venous distention persists, this does not prove true jugular venous pressure elevation, since it may reflect external compression of the vein by the cervical fascia or delayed blood flow caused by sclerotic venous valves.9 In these instances, the internal jugular pulsation level must be sought.
Jugular venous collapse with inspiration
Collapse of the inferior vena cava with forced inspiration is routinely evaluated during echocardiography as a way to estimate right atrial pressure. This finding has been extrapolated to the jugular veins, wherein the absence of venous collapse during vigorous inspiration or sniffing indicates elevated central venous pressures.10
Distinguishing venous from arterial pulsation
Features indicating venous rather than arterial pulsation were listed by Wood more than 50 years ago11 and are still relevant today. These include internal jugular pulsation that:
- Is soft, diffuse, undulant
- Is not palpable
- Has two crests and two troughs per cardiac cycle
- Has crests that do not coincide with the palpated carotid pulse (exceptions may be seen with the systolic timing of the v wave of tricuspid regurgitation)
- Has higher pressure in expiration, lower in inspiration (exceptions may be seen when Kussmaul physiology is present)
- Has pressure that rises with abdominal pressure
- Is obliterated by light pressure at the base of the neck.
In addition to the above criteria, a wave whose movement is predominantly a descent is nearly always venous.
Abdominojugular reflex
Firm, steady pressure over the abdomen will often result in a small rise in jugular venous pressure. In healthy people, this normalizes in a few seconds, even while manual pressure is maintained. Persistence of jugular venous pressure elevation beyond 10 seconds, followed by an abrupt fall upon withdrawal of manual pressure, is abnormal. This finding has implications similar to those of an elevated baseline jugular venous pressure.
SIGNIFICANCE OF JUGULAR VENOUS PRESSURE ELEVATION
Elevated jugular venous pressure is a manifestation of abnormal right heart dynamics, mostly commonly reflecting elevated pulmonary capillary wedge pressure from left heart failure.12 This usually implies fluid overload, indicating the need for diuresis.
Exceptions to this therapeutic implication include the presence of a primary right heart condition, pericardial disease, certain arrhythmias, and conditions that elevate intrathoracic pressure. These will be discussed below. One important example is the acute jugular venous pressure elevation seen in right ventricular infarction, in which the high venous pressure is compensatory and its reduction can produce hypotension and shock.13
Primary right heart conditions also include right-sided valvular disease, cor pulmonale (including pulmonary embolism and pulmonary hypertension), and the compressive effect of pericardial tamponade or constriction. A normal or near-normal jugular venous pressure significantly decreases the likelihood of significant constriction or of tamponade of a degree necessitating urgent pericardiocentesis.14
SPECIAL CIRCUMSTANCES
Presence of an intravenous line in the neck
An intravenous line in the neck will often prevent observation of the jugular venous pressure. A simple measure can often compensate for this. If the venous line can be temporarily disconnected, the central venous pressure can be measured directly. Using sterile technique, the line can be flushed with saline and aspirated to bring blood into the transparent tubing. Leaving the proximal end open to the air, and alternately raising and lowering it to confirm free flow, the level to which the blood rises can be easily observed. Observing small cardiac and respiratory variations of the meniscus confirms free communication with the central veins. Attaching the line to a transducer is another option, but this may be time-consuming, and establishing an accurate zero point is often difficult.
The previously described discrepancy between jugular venous pressure and central venous pressure has to be considered when drawing conclusions from this measurement.
Intrathoracic pressure elevators
Positive pressure ventilation will elevate intrathoracic pressure (including right atrial pressure) and hence the jugular venous pressure, making interpretation difficult.15 Large pleural effusions or pneumothorax may have a similar effect.16
Superior vena cava syndrome
Markedly elevated jugular venous pressure is here associated with absent or very diminished pulsation, as the caval obstruction has eliminated free communication with the right atrium.17 Associated facial plethora and edema, papilledema, and superficial venous distention over the chest wall will often confirm this diagnosis.
THE WAVEFORM
While the main purpose of viewing the neck veins is to establish the mean pressure, useful information can often be obtained by assessing the waveform. Abnormalities reflect arrhythmias, right heart hemodynamics, or pericardial disease.18 Changes may be subtle and difficult to detect, but some patterns can be quite readily appreciated (Figure 2). A limited selection follows.
Arrhythmias
Cannon a waves. These intermittent sharp positive deflections in the venous pulse represent right atrial contraction against a closed tricuspid valve. They are most commonly associated with premature ventricular complexes, but they occur in other conditions in which atrial and ventricular beating are dissociated, including complete heart block, atrioventricular dissociation, and electronic ventricular pacing.19–21
Repetitive cannon waves. These may be seen with atrioventricular junctional tachycardia or ventricular tachycardia with 1:1 retrograde ventriculoatrial conduction in which the tricuspid valve is closed to every atrial beat.
Fine rapid regular pulsation may be seen in atrial flutter and may be a useful clue in distinguishing this from sinus rhythm when there is 4:1 atrioventricular conduction and a normal ventricular rate.
Abnormal right heart hemodynamics
Large v waves (Lancisi sign). These surges, replacing the usual x descent in systole, are seen in tricuspid insufficiency when the right atrium and its venous attachments are not protected from the right ventricular systolic pressure.22 High right ventricular pressure will obviously enhance this systolic surge.
Large a waves. These reflect resistance to right atrial outflow and may be seen when right ventricular compliance is reduced by hypertrophy from chronic pressure overload or in tricuspid stenosis.23
Pericardial disease
Kussmaul sign is the paradoxical increase in jugular venous pressure with inspiration, observed in conditions associated with limited filling of the right ventricle. It is typically associated with constrictive pericarditis, although it occurs in only a minority of people with this condition.24 It may also be seen in restrictive cardiomyopathy, massive pulmonary embolism, right ventricular infarction, and tricuspid stenosis.25
Diaphragmatic descent during inspiration increases intra-abdominal pressure and decreases intrathoracic pressure. The resulting increased gradient between the abdomen and thorax enhances venous return from splanchnic vessels, which in the setting of a noncompliant right ventricle may result in increased right atrial (and, hence, jugular venous) pressure.26
It is important to point out that the Kussmaul sign does not occur with cardiac tamponade in the absence of associated pericardial constriction.
Exaggerated y descent is typically seen in pericardial constriction, in which the high pressure of the v wave falls rapidly at the onset of diastole, given initial minimal right ventricular resistance. Flow is abruptly stopped when the intrapericardial space is filled.
- Sherwood L. Human Physiology: From Cells to Systems. 8th ed. Belmont, CA: Brooks/Cole; 2012.
- Constant J. Using internal jugular pulsations as a manometer for right atrial pressure measurements. Cardiology 2000; 93:26–30.
- Deol GR, Collett N, Ashby A, Schmidt GA. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest 2011; 139:95–100.
- Wu X, Studer W, Erb T, Skarvan K, Seeberger MD. Competence of the internal jugular vein valve is damaged by cannulation and catheterization of the internal jugular vein. Anesthesiology 2000; 93:319–324.
- Ramana RK, Sanagala T, Lichtenberg R. A new angle on the angle of Louis. Congest Heart Fail 2006; 12:196–199.
- Seth R, Magner P, Matzinger F, van Walraven C. How far is the sternal angle from the mid-right atrium? J Gen Intern Med 2002; 17:852–856.
- Kee LL, Simonson JS, Stotts NA, Skov P, Schiller NB. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care 1993; 2:72–80.
- Park SY, Kim MJ, Kim MG, et al. Changes in the relationship between the right internal jugular vein and an anatomical landmark after head rotation. Korean J Anesthesiol 2011; 61:107–111.
- Sankoff J, Zidulka A. Non-invasive method for the rapid assessment of central venous pressure: description and validation by a single examiner. West J Emerg Med 2008; 9:201–205.
- Conn RD, O’Keefe JH. Simplified evaluation of the jugular venous pressure: significance of inspiratory collapse of jugular veins. Mo Med 2012; 109:150–152.
- Wood PH. Diseases of the Heart and Circulation. 2nd ed. Philadelphia, PA: Lippincott; 1956.
- Drazner MH, Brown RN, Kaiser PA, et al. Relationship of right- and left-sided filling pressures in patients with advanced heart failure: a 14-year multi-institutional analysis. J Heart Lung Transplant 2012; 31:67–72.
- Clark G, Strauss HD, Roberts R. Dobutamine vs furosemide in the treatment of cardiac failure due to right ventricular infarction. Chest 1980; 77:220–223.
- Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA 2007; 297:1810–1818.
- Zhou Q, Xiao W, An E, Zhou H, Yan M. Effects of four different positive airway pressures on right internal jugular vein catheterisation. Eur J Anaesthesiol 2012; 29:223–228.
- Jolobe OM. Disproportionate elevation of jugular venous pressure in pleural effusion. Br J Hosp Med (Lond) 2011; 72:582–585.
- Seo M, Shin WJ, Jun IG. Central venous catheter-related superior vena cava syndrome following renal transplantation—a case report. Korean J Anesthesiol 2012; 63:550–554.
- Applefeld MM. The jugular venous pressure and pulse contour. In:Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- El Gamal MI, Van Gelder LM. Chronic ventricular pacing with ventriculo-atrial conduction versus atrial pacing in three patients with symptomatic sinus bradycardia. Pacing Clin Electrophysiol 1981; 4:100–105.
- Berman ND, Waxman MB. Cannon waves with A-V association. Am Heart J 1976; 91:643–644.
- Luisada AA, Singhal A, Kim K. The jugular and hepatic tracings in normal subjects and in conduction defects. Acta Cardiol 1983; 38:405–424.
- Miller MJ, McKay RG, Ferguson JJ, et al. Right atrial pressure-volume relationships in tricuspid regurgitation. Circulation 1986; 73:799–808.
- Wooley CF, Fontana ME, Kilman JW, Ryan JM. Tricuspid stenosis. Atrial systolic murmur, tricuspid opening snap, and right atrial pressure pulse. Am J Med 1985; 78:375–384.
- McGee SR. Evidence-Based Physical Diagnosis. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012.
- Mittal SR, Garg S, Lalgarhia M. Jugular venous pressure and pulse wave form in the diagnosis of right ventricular infarction. Int J Cardiol 1996; 53:253–256.
- Bilchick KC, Wise RA. Paradoxical physical findings described by Kussmaul: pulsus paradoxus and Kussmaul’s sign. Lancet 2002; 359:1940–1942.
In this age of technological marvels, it is easy to become so reliant on them as to neglect the value of bedside physical signs. Yet these signs provide information that adds no cost, is immediately available, and can be repeated at will.
Few physical findings are as useful but as undervalued as is the estimation of the jugular venous pressure. Unfortunately, many practitioners at many levels of seniority and experience do not measure it correctly, leading to a vicious circle of unreliable information, lack of confidence, and underuse. Another reason for its underuse is that the jugular venous pressure does not correlate precisely with the right atrial pressure, as we will see below.
In this review, we will attempt to clarify physiologic principles and describe technical details. Much of this is simple but, as always, the devil is in the details.
ANATOMIC CONSIDERATIONS
Think of the systemic veins as a soft-walled and mildly distensible reservoir with fingerlike projections, analogous to a partially fluidfilled surgical glove.1 In a semi-upright position, the venous system is partially filled with blood and is collapsed above the level that this blood reaches up to.
Blood is constantly flowing in and out of this reservoir, flowing in by venous return and flowing out by the pumping action of the right side of the heart. The volume in the venous reservoir and hence the pressure are normally maintained by the variability of right ventricular stroke volume in accordance with the Frank-Starling law. Excess volume and pressure indicate failure of this homeostatic mechanism.
The internal jugular veins, being continuous with the superior vena cava, provide a visible measure of the degree to which the systemic venous reservoir is filled, a manometer that reflects the pressure in the right atrium—at least in theory.2 Thus, the vertical height above the right atrium to which they are distended and above which they are in a collapsed state should reflect the right atrial pressure.
(In fact, the jugular venous pressure may underestimate the right atrial pressure, for reasons still not understood. This will be discussed below.)
In a healthy person, the visible jugular veins are fully collapsed when the person is standing and are often distended to a variable degree when the person is supine. Selecting an appropriate intermediate position permits the top of the column (the meniscus) to become visible in the neck between the clavicle and the mandible.
DISCREPANCY BETWEEN JUGULAR VENOUS AND RIGHT ATRIAL PRESSURE
Several reports have indicated that the jugular venous pressure may underestimate the right atrial pressure. Deol et al3 confirmed this, while establishing an excellent correlation between the level of venous collapse (observed on ultrasonography) and the jugular venous pressure. The difference between the right atrial pressure and the jugular venous pressure tended to be greater at higher venous pressures.3
Most people have a valve near the termination of the internal jugular vein, with variable competence. Inhibition of reflux of blood from the superior vena cava into the internal jugular vein by this valve is the most plausible cause of this disparity.4
The failure of the jugular venous pressure to correlate with the right atrial pressure has been cited by some as a reason to doubt the value of a sign that cardiologists have long relied on. How do we reconcile this apparent paradox? Careful review of the literature that has demonstrated this lack of correlation reveals the following:
- When unequal, the jugular venous pressure always underestimates the right atrial pressure.
- The lack of correlation is less evident at lower venous pressures.
This indicates the following:
- In the presence of congestive heart failure, the right atrial pressure is at least as high and perhaps higher than the jugular venous pressure. Hence, if the jugular venous pressure is high, further treatment, especially diuresis, is needed.
- A jugular venous pressure of zero implies a euvolemic state.
Thus, the jugular venous pressure provides excellent guidance when administering diuresis in congestive heart failure. These deductions obviously require the clinical judgment that the elevated right atrial pressure and jugular venous pressure do indeed reflect elevation of pulmonary capillary wedge pressure rather than other conditions discussed later in this article.
WHICH REFERENCE POINT TO USE?
The two points that can be used as references above which the jugular venous pressure is expressed are the center of the right atrium and the sternal angle. While the former may reflect physiology, the latter is preferred, as it is always visible and has the added advantage of being close to the upper limit of normal, which is about 3 cm above this level.
The difference in height between these two reference points has often been quoted as 5 cm, but this is an underestimate in the body positions used in examination.5 Seth et al6 found a mean of 8 cm at 30° elevation, 9.7 cm at 45°, and 9.8 cm at 60°. The difference also varied between patients, being larger in association with smoking, older age, large body mass index, and large anterior-posterior diameter. These factors should be considered when trying to evaluate the significance of a particular jugular venous pressure.
The junction of the midaxillary line and the fourth left intercostal space (“the phlebostatic point”) has been recommended as a reference point by some, as it is level with the mid-right atrium. However, using the phlebostatic point as a reference position is cumbersome and results in a valid measurement only with the patient in the supine position.7
TECHNIQUE IS VITAL
Close adherence to technical details is vital in reliably and reproducibly measuring the pressure in the internal jugular veins (Figure 1).
The right side is usually observed first, as it is the side on which the examiner usually stands. Using the right side also avoids the rare occurrence of external compression of the left brachiocephalic vein.
Head and shoulders
The sternocleidomastoid muscle lies anterior to each internal jugular vein.8 When tense, it impedes good observation. Shortening, and hence relaxing, this muscle permits the meniscus to be observed. Correct positioning is achieved by:
- Placing a folded pillow behind the patient’s head
- Keeping the shoulders on the mattress
- Turning the head away and elevating the jaw, both slightly; this is often best achieved by gentle pressure of the palm of the observer's hand on the patient's forehead.
Degree of head elevation
Although the proper degree of head elevation is sometimes said to be between 30° and 60°, these numbers are approximate. The correct angle is that which brings the venous meniscus into the window of visibility in the neck between the clavicle and mandible.
Lighting
Shining a flashlight tangentially to the skin is often helpful, casting shadows that improve the visibility of vein motion. Dimming the room lighting may further enhance this effect. Directing a light perpendicular to the skin is not helpful.
Also check the external jugular vein
Checking the external jugular vein can help establish that the jugular venous pressure is normal. If the vein is initially collapsed, light finger pressure at the base of the neck will distend it. If the distention rapidly clears after release of this pressure, the jugular venous pressure is not elevated. However, if external jugular venous distention persists, this does not prove true jugular venous pressure elevation, since it may reflect external compression of the vein by the cervical fascia or delayed blood flow caused by sclerotic venous valves.9 In these instances, the internal jugular pulsation level must be sought.
Jugular venous collapse with inspiration
Collapse of the inferior vena cava with forced inspiration is routinely evaluated during echocardiography as a way to estimate right atrial pressure. This finding has been extrapolated to the jugular veins, wherein the absence of venous collapse during vigorous inspiration or sniffing indicates elevated central venous pressures.10
Distinguishing venous from arterial pulsation
Features indicating venous rather than arterial pulsation were listed by Wood more than 50 years ago11 and are still relevant today. These include internal jugular pulsation that:
- Is soft, diffuse, undulant
- Is not palpable
- Has two crests and two troughs per cardiac cycle
- Has crests that do not coincide with the palpated carotid pulse (exceptions may be seen with the systolic timing of the v wave of tricuspid regurgitation)
- Has higher pressure in expiration, lower in inspiration (exceptions may be seen when Kussmaul physiology is present)
- Has pressure that rises with abdominal pressure
- Is obliterated by light pressure at the base of the neck.
In addition to the above criteria, a wave whose movement is predominantly a descent is nearly always venous.
Abdominojugular reflex
Firm, steady pressure over the abdomen will often result in a small rise in jugular venous pressure. In healthy people, this normalizes in a few seconds, even while manual pressure is maintained. Persistence of jugular venous pressure elevation beyond 10 seconds, followed by an abrupt fall upon withdrawal of manual pressure, is abnormal. This finding has implications similar to those of an elevated baseline jugular venous pressure.
SIGNIFICANCE OF JUGULAR VENOUS PRESSURE ELEVATION
Elevated jugular venous pressure is a manifestation of abnormal right heart dynamics, mostly commonly reflecting elevated pulmonary capillary wedge pressure from left heart failure.12 This usually implies fluid overload, indicating the need for diuresis.
Exceptions to this therapeutic implication include the presence of a primary right heart condition, pericardial disease, certain arrhythmias, and conditions that elevate intrathoracic pressure. These will be discussed below. One important example is the acute jugular venous pressure elevation seen in right ventricular infarction, in which the high venous pressure is compensatory and its reduction can produce hypotension and shock.13
Primary right heart conditions also include right-sided valvular disease, cor pulmonale (including pulmonary embolism and pulmonary hypertension), and the compressive effect of pericardial tamponade or constriction. A normal or near-normal jugular venous pressure significantly decreases the likelihood of significant constriction or of tamponade of a degree necessitating urgent pericardiocentesis.14
SPECIAL CIRCUMSTANCES
Presence of an intravenous line in the neck
An intravenous line in the neck will often prevent observation of the jugular venous pressure. A simple measure can often compensate for this. If the venous line can be temporarily disconnected, the central venous pressure can be measured directly. Using sterile technique, the line can be flushed with saline and aspirated to bring blood into the transparent tubing. Leaving the proximal end open to the air, and alternately raising and lowering it to confirm free flow, the level to which the blood rises can be easily observed. Observing small cardiac and respiratory variations of the meniscus confirms free communication with the central veins. Attaching the line to a transducer is another option, but this may be time-consuming, and establishing an accurate zero point is often difficult.
The previously described discrepancy between jugular venous pressure and central venous pressure has to be considered when drawing conclusions from this measurement.
Intrathoracic pressure elevators
Positive pressure ventilation will elevate intrathoracic pressure (including right atrial pressure) and hence the jugular venous pressure, making interpretation difficult.15 Large pleural effusions or pneumothorax may have a similar effect.16
Superior vena cava syndrome
Markedly elevated jugular venous pressure is here associated with absent or very diminished pulsation, as the caval obstruction has eliminated free communication with the right atrium.17 Associated facial plethora and edema, papilledema, and superficial venous distention over the chest wall will often confirm this diagnosis.
THE WAVEFORM
While the main purpose of viewing the neck veins is to establish the mean pressure, useful information can often be obtained by assessing the waveform. Abnormalities reflect arrhythmias, right heart hemodynamics, or pericardial disease.18 Changes may be subtle and difficult to detect, but some patterns can be quite readily appreciated (Figure 2). A limited selection follows.
Arrhythmias
Cannon a waves. These intermittent sharp positive deflections in the venous pulse represent right atrial contraction against a closed tricuspid valve. They are most commonly associated with premature ventricular complexes, but they occur in other conditions in which atrial and ventricular beating are dissociated, including complete heart block, atrioventricular dissociation, and electronic ventricular pacing.19–21
Repetitive cannon waves. These may be seen with atrioventricular junctional tachycardia or ventricular tachycardia with 1:1 retrograde ventriculoatrial conduction in which the tricuspid valve is closed to every atrial beat.
Fine rapid regular pulsation may be seen in atrial flutter and may be a useful clue in distinguishing this from sinus rhythm when there is 4:1 atrioventricular conduction and a normal ventricular rate.
Abnormal right heart hemodynamics
Large v waves (Lancisi sign). These surges, replacing the usual x descent in systole, are seen in tricuspid insufficiency when the right atrium and its venous attachments are not protected from the right ventricular systolic pressure.22 High right ventricular pressure will obviously enhance this systolic surge.
Large a waves. These reflect resistance to right atrial outflow and may be seen when right ventricular compliance is reduced by hypertrophy from chronic pressure overload or in tricuspid stenosis.23
Pericardial disease
Kussmaul sign is the paradoxical increase in jugular venous pressure with inspiration, observed in conditions associated with limited filling of the right ventricle. It is typically associated with constrictive pericarditis, although it occurs in only a minority of people with this condition.24 It may also be seen in restrictive cardiomyopathy, massive pulmonary embolism, right ventricular infarction, and tricuspid stenosis.25
Diaphragmatic descent during inspiration increases intra-abdominal pressure and decreases intrathoracic pressure. The resulting increased gradient between the abdomen and thorax enhances venous return from splanchnic vessels, which in the setting of a noncompliant right ventricle may result in increased right atrial (and, hence, jugular venous) pressure.26
It is important to point out that the Kussmaul sign does not occur with cardiac tamponade in the absence of associated pericardial constriction.
Exaggerated y descent is typically seen in pericardial constriction, in which the high pressure of the v wave falls rapidly at the onset of diastole, given initial minimal right ventricular resistance. Flow is abruptly stopped when the intrapericardial space is filled.
In this age of technological marvels, it is easy to become so reliant on them as to neglect the value of bedside physical signs. Yet these signs provide information that adds no cost, is immediately available, and can be repeated at will.
Few physical findings are as useful but as undervalued as is the estimation of the jugular venous pressure. Unfortunately, many practitioners at many levels of seniority and experience do not measure it correctly, leading to a vicious circle of unreliable information, lack of confidence, and underuse. Another reason for its underuse is that the jugular venous pressure does not correlate precisely with the right atrial pressure, as we will see below.
In this review, we will attempt to clarify physiologic principles and describe technical details. Much of this is simple but, as always, the devil is in the details.
ANATOMIC CONSIDERATIONS
Think of the systemic veins as a soft-walled and mildly distensible reservoir with fingerlike projections, analogous to a partially fluidfilled surgical glove.1 In a semi-upright position, the venous system is partially filled with blood and is collapsed above the level that this blood reaches up to.
Blood is constantly flowing in and out of this reservoir, flowing in by venous return and flowing out by the pumping action of the right side of the heart. The volume in the venous reservoir and hence the pressure are normally maintained by the variability of right ventricular stroke volume in accordance with the Frank-Starling law. Excess volume and pressure indicate failure of this homeostatic mechanism.
The internal jugular veins, being continuous with the superior vena cava, provide a visible measure of the degree to which the systemic venous reservoir is filled, a manometer that reflects the pressure in the right atrium—at least in theory.2 Thus, the vertical height above the right atrium to which they are distended and above which they are in a collapsed state should reflect the right atrial pressure.
(In fact, the jugular venous pressure may underestimate the right atrial pressure, for reasons still not understood. This will be discussed below.)
In a healthy person, the visible jugular veins are fully collapsed when the person is standing and are often distended to a variable degree when the person is supine. Selecting an appropriate intermediate position permits the top of the column (the meniscus) to become visible in the neck between the clavicle and the mandible.
DISCREPANCY BETWEEN JUGULAR VENOUS AND RIGHT ATRIAL PRESSURE
Several reports have indicated that the jugular venous pressure may underestimate the right atrial pressure. Deol et al3 confirmed this, while establishing an excellent correlation between the level of venous collapse (observed on ultrasonography) and the jugular venous pressure. The difference between the right atrial pressure and the jugular venous pressure tended to be greater at higher venous pressures.3
Most people have a valve near the termination of the internal jugular vein, with variable competence. Inhibition of reflux of blood from the superior vena cava into the internal jugular vein by this valve is the most plausible cause of this disparity.4
The failure of the jugular venous pressure to correlate with the right atrial pressure has been cited by some as a reason to doubt the value of a sign that cardiologists have long relied on. How do we reconcile this apparent paradox? Careful review of the literature that has demonstrated this lack of correlation reveals the following:
- When unequal, the jugular venous pressure always underestimates the right atrial pressure.
- The lack of correlation is less evident at lower venous pressures.
This indicates the following:
- In the presence of congestive heart failure, the right atrial pressure is at least as high and perhaps higher than the jugular venous pressure. Hence, if the jugular venous pressure is high, further treatment, especially diuresis, is needed.
- A jugular venous pressure of zero implies a euvolemic state.
Thus, the jugular venous pressure provides excellent guidance when administering diuresis in congestive heart failure. These deductions obviously require the clinical judgment that the elevated right atrial pressure and jugular venous pressure do indeed reflect elevation of pulmonary capillary wedge pressure rather than other conditions discussed later in this article.
WHICH REFERENCE POINT TO USE?
The two points that can be used as references above which the jugular venous pressure is expressed are the center of the right atrium and the sternal angle. While the former may reflect physiology, the latter is preferred, as it is always visible and has the added advantage of being close to the upper limit of normal, which is about 3 cm above this level.
The difference in height between these two reference points has often been quoted as 5 cm, but this is an underestimate in the body positions used in examination.5 Seth et al6 found a mean of 8 cm at 30° elevation, 9.7 cm at 45°, and 9.8 cm at 60°. The difference also varied between patients, being larger in association with smoking, older age, large body mass index, and large anterior-posterior diameter. These factors should be considered when trying to evaluate the significance of a particular jugular venous pressure.
The junction of the midaxillary line and the fourth left intercostal space (“the phlebostatic point”) has been recommended as a reference point by some, as it is level with the mid-right atrium. However, using the phlebostatic point as a reference position is cumbersome and results in a valid measurement only with the patient in the supine position.7
TECHNIQUE IS VITAL
Close adherence to technical details is vital in reliably and reproducibly measuring the pressure in the internal jugular veins (Figure 1).
The right side is usually observed first, as it is the side on which the examiner usually stands. Using the right side also avoids the rare occurrence of external compression of the left brachiocephalic vein.
Head and shoulders
The sternocleidomastoid muscle lies anterior to each internal jugular vein.8 When tense, it impedes good observation. Shortening, and hence relaxing, this muscle permits the meniscus to be observed. Correct positioning is achieved by:
- Placing a folded pillow behind the patient’s head
- Keeping the shoulders on the mattress
- Turning the head away and elevating the jaw, both slightly; this is often best achieved by gentle pressure of the palm of the observer's hand on the patient's forehead.
Degree of head elevation
Although the proper degree of head elevation is sometimes said to be between 30° and 60°, these numbers are approximate. The correct angle is that which brings the venous meniscus into the window of visibility in the neck between the clavicle and mandible.
Lighting
Shining a flashlight tangentially to the skin is often helpful, casting shadows that improve the visibility of vein motion. Dimming the room lighting may further enhance this effect. Directing a light perpendicular to the skin is not helpful.
Also check the external jugular vein
Checking the external jugular vein can help establish that the jugular venous pressure is normal. If the vein is initially collapsed, light finger pressure at the base of the neck will distend it. If the distention rapidly clears after release of this pressure, the jugular venous pressure is not elevated. However, if external jugular venous distention persists, this does not prove true jugular venous pressure elevation, since it may reflect external compression of the vein by the cervical fascia or delayed blood flow caused by sclerotic venous valves.9 In these instances, the internal jugular pulsation level must be sought.
Jugular venous collapse with inspiration
Collapse of the inferior vena cava with forced inspiration is routinely evaluated during echocardiography as a way to estimate right atrial pressure. This finding has been extrapolated to the jugular veins, wherein the absence of venous collapse during vigorous inspiration or sniffing indicates elevated central venous pressures.10
Distinguishing venous from arterial pulsation
Features indicating venous rather than arterial pulsation were listed by Wood more than 50 years ago11 and are still relevant today. These include internal jugular pulsation that:
- Is soft, diffuse, undulant
- Is not palpable
- Has two crests and two troughs per cardiac cycle
- Has crests that do not coincide with the palpated carotid pulse (exceptions may be seen with the systolic timing of the v wave of tricuspid regurgitation)
- Has higher pressure in expiration, lower in inspiration (exceptions may be seen when Kussmaul physiology is present)
- Has pressure that rises with abdominal pressure
- Is obliterated by light pressure at the base of the neck.
In addition to the above criteria, a wave whose movement is predominantly a descent is nearly always venous.
Abdominojugular reflex
Firm, steady pressure over the abdomen will often result in a small rise in jugular venous pressure. In healthy people, this normalizes in a few seconds, even while manual pressure is maintained. Persistence of jugular venous pressure elevation beyond 10 seconds, followed by an abrupt fall upon withdrawal of manual pressure, is abnormal. This finding has implications similar to those of an elevated baseline jugular venous pressure.
SIGNIFICANCE OF JUGULAR VENOUS PRESSURE ELEVATION
Elevated jugular venous pressure is a manifestation of abnormal right heart dynamics, mostly commonly reflecting elevated pulmonary capillary wedge pressure from left heart failure.12 This usually implies fluid overload, indicating the need for diuresis.
Exceptions to this therapeutic implication include the presence of a primary right heart condition, pericardial disease, certain arrhythmias, and conditions that elevate intrathoracic pressure. These will be discussed below. One important example is the acute jugular venous pressure elevation seen in right ventricular infarction, in which the high venous pressure is compensatory and its reduction can produce hypotension and shock.13
Primary right heart conditions also include right-sided valvular disease, cor pulmonale (including pulmonary embolism and pulmonary hypertension), and the compressive effect of pericardial tamponade or constriction. A normal or near-normal jugular venous pressure significantly decreases the likelihood of significant constriction or of tamponade of a degree necessitating urgent pericardiocentesis.14
SPECIAL CIRCUMSTANCES
Presence of an intravenous line in the neck
An intravenous line in the neck will often prevent observation of the jugular venous pressure. A simple measure can often compensate for this. If the venous line can be temporarily disconnected, the central venous pressure can be measured directly. Using sterile technique, the line can be flushed with saline and aspirated to bring blood into the transparent tubing. Leaving the proximal end open to the air, and alternately raising and lowering it to confirm free flow, the level to which the blood rises can be easily observed. Observing small cardiac and respiratory variations of the meniscus confirms free communication with the central veins. Attaching the line to a transducer is another option, but this may be time-consuming, and establishing an accurate zero point is often difficult.
The previously described discrepancy between jugular venous pressure and central venous pressure has to be considered when drawing conclusions from this measurement.
Intrathoracic pressure elevators
Positive pressure ventilation will elevate intrathoracic pressure (including right atrial pressure) and hence the jugular venous pressure, making interpretation difficult.15 Large pleural effusions or pneumothorax may have a similar effect.16
Superior vena cava syndrome
Markedly elevated jugular venous pressure is here associated with absent or very diminished pulsation, as the caval obstruction has eliminated free communication with the right atrium.17 Associated facial plethora and edema, papilledema, and superficial venous distention over the chest wall will often confirm this diagnosis.
THE WAVEFORM
While the main purpose of viewing the neck veins is to establish the mean pressure, useful information can often be obtained by assessing the waveform. Abnormalities reflect arrhythmias, right heart hemodynamics, or pericardial disease.18 Changes may be subtle and difficult to detect, but some patterns can be quite readily appreciated (Figure 2). A limited selection follows.
Arrhythmias
Cannon a waves. These intermittent sharp positive deflections in the venous pulse represent right atrial contraction against a closed tricuspid valve. They are most commonly associated with premature ventricular complexes, but they occur in other conditions in which atrial and ventricular beating are dissociated, including complete heart block, atrioventricular dissociation, and electronic ventricular pacing.19–21
Repetitive cannon waves. These may be seen with atrioventricular junctional tachycardia or ventricular tachycardia with 1:1 retrograde ventriculoatrial conduction in which the tricuspid valve is closed to every atrial beat.
Fine rapid regular pulsation may be seen in atrial flutter and may be a useful clue in distinguishing this from sinus rhythm when there is 4:1 atrioventricular conduction and a normal ventricular rate.
Abnormal right heart hemodynamics
Large v waves (Lancisi sign). These surges, replacing the usual x descent in systole, are seen in tricuspid insufficiency when the right atrium and its venous attachments are not protected from the right ventricular systolic pressure.22 High right ventricular pressure will obviously enhance this systolic surge.
Large a waves. These reflect resistance to right atrial outflow and may be seen when right ventricular compliance is reduced by hypertrophy from chronic pressure overload or in tricuspid stenosis.23
Pericardial disease
Kussmaul sign is the paradoxical increase in jugular venous pressure with inspiration, observed in conditions associated with limited filling of the right ventricle. It is typically associated with constrictive pericarditis, although it occurs in only a minority of people with this condition.24 It may also be seen in restrictive cardiomyopathy, massive pulmonary embolism, right ventricular infarction, and tricuspid stenosis.25
Diaphragmatic descent during inspiration increases intra-abdominal pressure and decreases intrathoracic pressure. The resulting increased gradient between the abdomen and thorax enhances venous return from splanchnic vessels, which in the setting of a noncompliant right ventricle may result in increased right atrial (and, hence, jugular venous) pressure.26
It is important to point out that the Kussmaul sign does not occur with cardiac tamponade in the absence of associated pericardial constriction.
Exaggerated y descent is typically seen in pericardial constriction, in which the high pressure of the v wave falls rapidly at the onset of diastole, given initial minimal right ventricular resistance. Flow is abruptly stopped when the intrapericardial space is filled.
- Sherwood L. Human Physiology: From Cells to Systems. 8th ed. Belmont, CA: Brooks/Cole; 2012.
- Constant J. Using internal jugular pulsations as a manometer for right atrial pressure measurements. Cardiology 2000; 93:26–30.
- Deol GR, Collett N, Ashby A, Schmidt GA. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest 2011; 139:95–100.
- Wu X, Studer W, Erb T, Skarvan K, Seeberger MD. Competence of the internal jugular vein valve is damaged by cannulation and catheterization of the internal jugular vein. Anesthesiology 2000; 93:319–324.
- Ramana RK, Sanagala T, Lichtenberg R. A new angle on the angle of Louis. Congest Heart Fail 2006; 12:196–199.
- Seth R, Magner P, Matzinger F, van Walraven C. How far is the sternal angle from the mid-right atrium? J Gen Intern Med 2002; 17:852–856.
- Kee LL, Simonson JS, Stotts NA, Skov P, Schiller NB. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care 1993; 2:72–80.
- Park SY, Kim MJ, Kim MG, et al. Changes in the relationship between the right internal jugular vein and an anatomical landmark after head rotation. Korean J Anesthesiol 2011; 61:107–111.
- Sankoff J, Zidulka A. Non-invasive method for the rapid assessment of central venous pressure: description and validation by a single examiner. West J Emerg Med 2008; 9:201–205.
- Conn RD, O’Keefe JH. Simplified evaluation of the jugular venous pressure: significance of inspiratory collapse of jugular veins. Mo Med 2012; 109:150–152.
- Wood PH. Diseases of the Heart and Circulation. 2nd ed. Philadelphia, PA: Lippincott; 1956.
- Drazner MH, Brown RN, Kaiser PA, et al. Relationship of right- and left-sided filling pressures in patients with advanced heart failure: a 14-year multi-institutional analysis. J Heart Lung Transplant 2012; 31:67–72.
- Clark G, Strauss HD, Roberts R. Dobutamine vs furosemide in the treatment of cardiac failure due to right ventricular infarction. Chest 1980; 77:220–223.
- Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA 2007; 297:1810–1818.
- Zhou Q, Xiao W, An E, Zhou H, Yan M. Effects of four different positive airway pressures on right internal jugular vein catheterisation. Eur J Anaesthesiol 2012; 29:223–228.
- Jolobe OM. Disproportionate elevation of jugular venous pressure in pleural effusion. Br J Hosp Med (Lond) 2011; 72:582–585.
- Seo M, Shin WJ, Jun IG. Central venous catheter-related superior vena cava syndrome following renal transplantation—a case report. Korean J Anesthesiol 2012; 63:550–554.
- Applefeld MM. The jugular venous pressure and pulse contour. In:Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- El Gamal MI, Van Gelder LM. Chronic ventricular pacing with ventriculo-atrial conduction versus atrial pacing in three patients with symptomatic sinus bradycardia. Pacing Clin Electrophysiol 1981; 4:100–105.
- Berman ND, Waxman MB. Cannon waves with A-V association. Am Heart J 1976; 91:643–644.
- Luisada AA, Singhal A, Kim K. The jugular and hepatic tracings in normal subjects and in conduction defects. Acta Cardiol 1983; 38:405–424.
- Miller MJ, McKay RG, Ferguson JJ, et al. Right atrial pressure-volume relationships in tricuspid regurgitation. Circulation 1986; 73:799–808.
- Wooley CF, Fontana ME, Kilman JW, Ryan JM. Tricuspid stenosis. Atrial systolic murmur, tricuspid opening snap, and right atrial pressure pulse. Am J Med 1985; 78:375–384.
- McGee SR. Evidence-Based Physical Diagnosis. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012.
- Mittal SR, Garg S, Lalgarhia M. Jugular venous pressure and pulse wave form in the diagnosis of right ventricular infarction. Int J Cardiol 1996; 53:253–256.
- Bilchick KC, Wise RA. Paradoxical physical findings described by Kussmaul: pulsus paradoxus and Kussmaul’s sign. Lancet 2002; 359:1940–1942.
- Sherwood L. Human Physiology: From Cells to Systems. 8th ed. Belmont, CA: Brooks/Cole; 2012.
- Constant J. Using internal jugular pulsations as a manometer for right atrial pressure measurements. Cardiology 2000; 93:26–30.
- Deol GR, Collett N, Ashby A, Schmidt GA. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest 2011; 139:95–100.
- Wu X, Studer W, Erb T, Skarvan K, Seeberger MD. Competence of the internal jugular vein valve is damaged by cannulation and catheterization of the internal jugular vein. Anesthesiology 2000; 93:319–324.
- Ramana RK, Sanagala T, Lichtenberg R. A new angle on the angle of Louis. Congest Heart Fail 2006; 12:196–199.
- Seth R, Magner P, Matzinger F, van Walraven C. How far is the sternal angle from the mid-right atrium? J Gen Intern Med 2002; 17:852–856.
- Kee LL, Simonson JS, Stotts NA, Skov P, Schiller NB. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care 1993; 2:72–80.
- Park SY, Kim MJ, Kim MG, et al. Changes in the relationship between the right internal jugular vein and an anatomical landmark after head rotation. Korean J Anesthesiol 2011; 61:107–111.
- Sankoff J, Zidulka A. Non-invasive method for the rapid assessment of central venous pressure: description and validation by a single examiner. West J Emerg Med 2008; 9:201–205.
- Conn RD, O’Keefe JH. Simplified evaluation of the jugular venous pressure: significance of inspiratory collapse of jugular veins. Mo Med 2012; 109:150–152.
- Wood PH. Diseases of the Heart and Circulation. 2nd ed. Philadelphia, PA: Lippincott; 1956.
- Drazner MH, Brown RN, Kaiser PA, et al. Relationship of right- and left-sided filling pressures in patients with advanced heart failure: a 14-year multi-institutional analysis. J Heart Lung Transplant 2012; 31:67–72.
- Clark G, Strauss HD, Roberts R. Dobutamine vs furosemide in the treatment of cardiac failure due to right ventricular infarction. Chest 1980; 77:220–223.
- Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA 2007; 297:1810–1818.
- Zhou Q, Xiao W, An E, Zhou H, Yan M. Effects of four different positive airway pressures on right internal jugular vein catheterisation. Eur J Anaesthesiol 2012; 29:223–228.
- Jolobe OM. Disproportionate elevation of jugular venous pressure in pleural effusion. Br J Hosp Med (Lond) 2011; 72:582–585.
- Seo M, Shin WJ, Jun IG. Central venous catheter-related superior vena cava syndrome following renal transplantation—a case report. Korean J Anesthesiol 2012; 63:550–554.
- Applefeld MM. The jugular venous pressure and pulse contour. In:Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- El Gamal MI, Van Gelder LM. Chronic ventricular pacing with ventriculo-atrial conduction versus atrial pacing in three patients with symptomatic sinus bradycardia. Pacing Clin Electrophysiol 1981; 4:100–105.
- Berman ND, Waxman MB. Cannon waves with A-V association. Am Heart J 1976; 91:643–644.
- Luisada AA, Singhal A, Kim K. The jugular and hepatic tracings in normal subjects and in conduction defects. Acta Cardiol 1983; 38:405–424.
- Miller MJ, McKay RG, Ferguson JJ, et al. Right atrial pressure-volume relationships in tricuspid regurgitation. Circulation 1986; 73:799–808.
- Wooley CF, Fontana ME, Kilman JW, Ryan JM. Tricuspid stenosis. Atrial systolic murmur, tricuspid opening snap, and right atrial pressure pulse. Am J Med 1985; 78:375–384.
- McGee SR. Evidence-Based Physical Diagnosis. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012.
- Mittal SR, Garg S, Lalgarhia M. Jugular venous pressure and pulse wave form in the diagnosis of right ventricular infarction. Int J Cardiol 1996; 53:253–256.
- Bilchick KC, Wise RA. Paradoxical physical findings described by Kussmaul: pulsus paradoxus and Kussmaul’s sign. Lancet 2002; 359:1940–1942.
KEY POINTS
- If the jugular venous pressure differs from the true right atrial pressure, the jugular venous pressure is always the lower value.
- The jugular venous pressure is useful to observe when diagnosing congestive heart failure and when considering the need for or the adequacy of diuresis.
- The jugular venous wave form is more difficult to observe than its elevation but can yield useful information in the assessment of certain arrhythmias, right-heart conditions, and pericardial disease.