User login
• Delay discharge of late preterm infants to a minimum of 48 hours to prevent readmission. B
• Perform transcutaneous or total serum bilirubin testing before discharging late preterm infants. C
• Perform a formal feeding assessment of breastfed infants prior to discharge. C
• Ensure that a follow-up appointment is made for 24 to 48 hours after discharge. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Laura M delivers her third baby at 35 weeks 4 days after an uneventful spontaneous labor. Julia, 5 lb 1 oz, has Apgar scores of 8 and 9. You see them on the mother-baby unit Friday afternoon, 36 hours after the delivery.
Ms. M has successfully breastfed her other 2 children and is planning to breastfeed Julia as well. She says the infant is nursing well today but seemed sleepy yesterday. The nursing notes say that Julia went to the nursery overnight because her mother was tired, and the infant spit up after receiving a formula bottle. Ms. M is asking you to discharge her because tomorrow is her son’s birthday. After considering this and her experience with breastfeeding, you decide to discharge her with follow-up on Monday instead of checking her out to your partner for the weekend.
Ms. M returns to your office on Monday with Julia, whose weight is down 10% and is “glowing yellow.” The baby is not latching well at the breast and is spitting up when Ms. M tries to supplement with formula. After examining Julia and checking lab work (bilirubin, 20 mg/dL), you decide to readmit her for feeding difficulties and hyperbilirubinemia.
Complications are common with late preterm infants, which refers to babies born between 34 weeks 0 days and 36 weeks 6 days of pregnancy. Between 1990 and 2006, there was a dramatic (25%) increase in the rate of late preterm infants in the United States, although more recently this number has leveled off.1
Several factors have been linked to increased late preterm births: maternal obesity, increased maternal age, and the increasing rate of multiple gestation pregnancies that have resulted from the expanded use of reproductive technology.2 Similarly, treatment of severe preeclampsia and premature rupture of membranes often includes delivery after 34 weeks of gestation,3 further contributing to the problem. Finally, higher rates of antenatal screening have contributed to more inductions and cesarean sections at earlier gestational ages. One study even found a correlation between higher malpractice premiums and more frequent late preterm inductions.4
Don’t let their appearance fool you
At first appearance, late preterm infants are similar to term infants in terms of Apgar scores,5 size, and weight.2 However, the care of these infants can be complex. They are often placed in well-infant nurseries under the same protocols as term infants and discharged before an adequate observation period. These infants have both increased short- and long-term morbidity and mortality and use a significant amount of health care resources.5 Morbidity in these infants decreases with each week of gestation from 34 weeks to a nadir at 39 weeks and can be unrelated to maternal and pregnancy complications.6
The following are some important issues to keep in mind when caring for these infants.
Hypothermia and hypoglycemia
Late preterm infants experience increased cold stress because of their limited fat stores, reduced brown fat, an immature epidermal barrier, and increased surface area to body mass ratio.2 Hypothermia increases the metabolic demands on the neonate and can worsen hypoglycemia as well as respiratory distress.7
Ideally, clinicians should dry these infants with warm blankets, place them skin-to-skin with their mother, and cover them with a warm blanket and cap to avoid excess energy expenditure.8 If conditions necessitate, neonates can be placed in a radiant warmer. Infants’ temperature needs to be monitored within the first 30 minutes of life and frequently reassessed during the first 12 hours of life—the “transition period.”8 The infant’s axillary temperature should be maintained between 36.5°C and 37.4°C (97.7-99.3°F); the temperature should remain stable in an open crib for the 12 hours before discharge.2
Decreased glycogen stores, increased glucose utilization, and immature hepatic enzymes help to explain the fact that hypoglycemia is 3 times more common in late preterm infants compared with full-term neonates.7 In all newborns, glucose levels decrease to their nadir between 30 and 90 minutes of life and normally trigger the breakdown of glycogen if the infant does not eat.7 Hypoglycemia can manifest as a change in level of consciousness, apnea, cyanosis, tachypnea, hypothermia, and seizures.9 The evidence is limited and there is controversy as to what level of hypoglycemia and over what duration of time is harmful.9
Most experts agree that breastfeeding should be started in the delivery room, and plasma glucose checked at 60 minutes of life and any time an infant is symptomatic. A level less than 45 mg/dL during the transition period should prompt feeding.9 Glucose levels should be rechecked within an hour of feeding and every 3 hours thereafter. If the level remains low or the infant is not interested in feeding, give a bolus of D10W and consider an infusion.7,10 TABLE 110 highlights one proposed method of glucose management.
TABLE 1
How best to manage glucose in a late preterm newborn10
| Asymptomatic late preterm infants | Glucose level (mg/dL) | Response |
|---|---|---|
| Check plasma glucose at 1 hour of life | <45 | Feed, recheck 1 h |
| Subsequent glucose monitoring | <35 | IV infusion* |
| >35 | Rescreen q3h for 36 h | |
| Symptomatic late preterm infants | ||
| Infusion for goal >55 mg/dL | <45 | Minibolus;† IV infusion* |
| *IV infusion=D10W at 6-8 mg/kg/min. †Minibolus=200 mg/kg D10W (2 mL/kg). Adapted with permission from: Macmillan Publishers Ltd. Adamkin DH. Late preterm infants: severe hyperbilirubinemia and postnatal glucose homeostasis. J Perinatol. 2009;29:S12-S17. Copyright 2009. | ||
Respiratory distress
At least 30% of late preterm infants will have some evidence of respiratory distress,5 which is defined as the need for oxygen supplementation due to tachypnea, grunting, nasal flaring, retractions, or cyanosis. Those at highest risk are white males born via cesarean section.11 Transient tachypnea of the newborn (TTN) appears to be the cause of almost half the cases of respiratory distress in these young patients.12 As this is a diagnosis by exclusion, consider other common causes: respiratory distress syndrome, neonatal pneumonia, meconium aspiration syndrome, and persistent pulmonary hypertension.12 The need for ventilator support is a significant concern in this group and increases exponentially with decreasing gestational age.6
Hyperbilirubinemia
More than half of all late preterm infants will present with clinically significant jaundice.5 Late preterm infants have an increased bilirubin load, decreased uptake of bilirubin, and delayed conjugation. They are less able to bind bilirubin to albumin, which increases their predisposition to bilirubin-induced neurological dysfunction and kernicterus.13 They also have more difficulty with breastfeeding, which exacerbates their hyperbilirubinemia.14
Infants born at 36 weeks have an 8-fold increased risk of developing severe hyperbilirubinemia (total serum bilirubin >20 mg/dL) than those born at 41 weeks,13 which explains why they are disproportionately represented in the US Pilot Kernicterus Registry.14 These infants can develop neurological sequelae at lower levels of bilirubin than their term counterparts and have less chance of complete recovery once intensive therapy has been implemented.14
The 2 main risk factors for severe hyperbilirubinemia have to do with discharge time and breastfeeding. Discharge at less than 48 hours is a risk factor for both term and late preterm infants.14,15 This is likely due to the fact that bilirubin peaks in late preterm infants between Days 5 and 7, and in term infants between Days 3 and 5.16 Difficulties with breastfeeding, the second risk factor,17 can be due to a combination of delayed maternal lactogenesis and ineffective milk removal on the part of the infant.18 When infants ingest smaller volumes of milk, bowel movements are infrequent and the bilirubin in the gut gets reabsorbed instead of excreted.
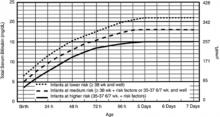
American Academy of Pediatrics (AAP) guidelines suggest measuring total serum bilirubin or transcutaneous bilirubin and plotting the value on an hour-specific, gestational-age-specific, risk-specific nomogram (FIGURE).19 Alternately, BiliTool (http://www.bilitool.org) can be used to individualize an infant’s risk.
FIGURE
Bilirubin levels and risk of significant hyperbilirubinemia19
Bilirubin levels should be plotted according to the infant’s hours of life and assessed according to risk factors on the appropriate risk line. If infants are 34 weeks 0 days to 34 weeks 6 days, they should be assessed on the high risk line.
- Use total bilirubin. Do not subtract direct reacting or conjugated bilirubin.
- Risk factors include isoimmune hemolytic disease, G6PD deficiency, asphyxia, significant lethargy, temperature instability, sepsis, acidosis, or albumin <3.0 g/dL (if measured).
- For well infants 35-37 6/7 weeks, you can adjust the total serum bilirubin (TSB) levels for intervention around the medium risk line. It is an option to intervene at lower TSB levels for infants closer to 35 weeks and at higher TSB levels for those closer to 37 6/7 weeks.
- It is an option to provide conventional phototherapy in the hospital or at home at TSB levels of 2-3 mg/dL (35-50 mmol/L) below those shown, but home phototherapy should not be used in any infant with risk factors.
Reprinted with permission from: American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316. Copyright © 2004 by the American Academy of Pediatrics.
Feeding difficulties
The advantages of breast milk feeding for these babies are great. Unfortunately, it is breastfed infants who are more likely to have feeding difficulties and are at higher risk for readmission.17 Early feeding skills are complex and challenging. Because of their immaturity, late preterm infants have less effective suck and swallow coordination. They can be sleepier and have less stamina.10 Infants require coordinated oral motor movements, breathing, and swallowing to avoid desaturation and aspiration.20 It is also important to note that almost every reported case of kernicterus in the past 20 years has been in breastfed infants whose feeding was not well established.13 First-born infants are especially at risk, as it takes longer to establish an adequate supply of milk.
For late preterm infants, it is imperative to establish successful breastfeeding to avoid dehydration and jaundice. Lactation consultation, education, and close follow-up are essential to successful breastfeeding in this group.18 The AAP Committee on Fetus and Newborn recommends a formal breastfeeding evaluation by trained caregivers at least twice daily prior to discharge.2
Brain injury
Late gestation is a critical period of brain growth. The 34-week-old brain weighs 65% of the term brain and increases linearly with each week. Fifty percent of the increase in cortical volume happens after 34 weeks.21 The risk of intraventricular hemorrhage and periventricular leukomalacia, while common in earlier preemies, is rare in infants born after 34 weeks. However, there is evidence to suggest other complications. Late preterm infants are more likely to be diagnosed with developmental delay and require special resources in preschool and less likely to be ready for school.22
Sepsis
While late preterm neonates do have a small but significant increase in culture-proven sepsis and pneumonia compared with term babies,6 the work-up for possible sepsis is 3 times more likely. When these infants have poor feeding, mild respiratory distress, or TTN, physicians become concerned about sepsis and initiate a work-up.5 Currently there are no management guidelines for sepsis evaluation in this subset of preterm infants.23
Readmission is a distinct possibility
One study of healthy late preterm infants showed a readmission rate of 4.8%. The most common reasons for readmission were jaundice and infection.17 Risk factors for readmission were breastfeeding, primiparity, labor and delivery complications, public payer source at delivery, and a mother of Asian/Pacific Islander ethnicity.17 Another study showed that discharge at less than 48 hours significantly increased the likelihood of readmission, even more so if the infant was breastfeeding.15
Several recent studies have highlighted a relationship between decreasing gestational age and a wide range of long-term adverse outcomes. In the early years of childhood, there is an increased risk for developmental delay and decreased kindergarten readiness.22 There is also a significant risk for disability, including cerebral palsy, mental retardation, and behavioral disorders.
Late preterm infants are at greater risk for several complications and the mortality rate is high in this group, when compared with term infants. By initial appearance and even weight, they rival their term counterparts. However, while they may look much like term babies and not weigh much less, they need more intense monitoring and should meet stringent discharge criteria (TABLE 22).
TABLE 2
Minimum discharge criteria for late preterm infants2
All criteria should be met prior to discharge.
|
| Adapted with permission from: Engle WA, Tomashek KM, Wallman C, Committee on Fetus and Newborn. “Late-preterm” infants: a population at risk. Pediatrics. 2007;120:1390-1401. Copyright © 2007 by the American Academy of Pediatrics. |
Clearly, more studies need to be done to address the unique needs and specific treatment guidelines for these infants. In fact, hospitals may need to consider introducing neonatal observation nurseries with protocols specifically tailored for late preterm infants.
CASE Ms. M and Julia likely would have been better served with an extra day in the hospital to address feeding issues and monitor for hyperbilirubinemia. Julia received phototherapy, IV fluids, and intensive lactation support, which included pumped breast milk given through a supplemental nursing system.
Over the course of 48 hours, her bilirubin decreased to 14 mg/dL and she was able to feed for longer periods of time without tiring. While both Ms. M and Julia’s initial outcomes were good, an extra day of feeding support may have prevented a readmission, thousands of dollars in care, and unnecessary stress on both mother and baby.
CORRESPONDENCE
Kimberly Stuckey-Schrock, MD, IU Health Goshen, Lincoln Avenue Family Medicine, 400 W Lincoln Avenue, Goshen, IN 46526; kstuckeyschr@iuhealth.org
1. Martin JA, Hamilton BE, Sutton PD, et al. Birth: final data for 2008. Natl Vital Stat Rep. 2010;59:1, 3-71.
2. Engle WA, Tomashek KM, Wallman C. Committee on Fetus and Newborn. “Late-preterm” infants: a population at risk. Pediatrics. 2007;120:1390-1401.
3. Gabbe SG, Niebyl JR, Simpson JL. eds. Obstetrics Normal and Problem Pregnancies. Philadelphia, Pa: Churchill Livingstone; 2007.
4. Murthy K, Grobman WA, Lee TA, et al. Obstetricians’ rising liability insurance premiums and inductions at late preterm gestations. Med Care. 2009;47:425-430.
5. Wang ML, Dorer DJ, Fleming MP, et al. Clinical outcomes of near-term infants. Pediatrics. 2004;114:372-376.
6. Melamed N, Klinger G, Tenenbaum-Gavish K, et al. Short-term neonatal outcome in low-risk, spontaneous, singleton, late preterm deliveries. Obstet Gynecol. 2009;114:253-260.
7. Garg M, Devaskar SU. Glucose metabolism in the late preterm infant. Clin Perinatol. 2006;33:853-870.
8. Laptook A, Jackson G. Cold stress and hypoglycemia in the late preterm (“near-term”) infant: impact on nursery of admission. Semin Perinatol. 2006;30:24-27.
9. Cornblath M, Hawdon JM, Williams AF, et al. Controversies regarding definition of neonatal hypoglycemia: suggested operational thresholds. Pediatrics. 2000;105:1141-1145.
10. Adamkin D. Late preterm infants: severe hyperbilirubinemia and postnatal glucose homeostasis. J Perinatol. 2009;29(suppl):S12-S17.
11. Clark R. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol. 2005;25:251-257.
12. Kalyoncu O, Aygun C, Cetinoglu E, et al. Neonatal morbidity and mortality of late-preterm babies. J Matern Fetal Neonatal Med. 2010;23:607-612.
13. Watchko J. Hyperbilirubinemia and bilirubin toxicity in the late preterm infant. Clin Perinatol. 2006;33:839-852.
14. Bhutani V. Kernicterus in late preterm infants cared for as term healthy infants. Semin Perinatol. 2006;30:89-97.
15. Tomashek KM, Shapiro-Mendoza CK, Weiss J, et al. Early discharge among late preterm and term newborns and risk of neonatal morbidity. Semin Perinatol. 2006;30:61-68.
16. Sarici SU, Serdar MA, Korkmaz A, et al. Incidence, course, and prediction of hyperbilirubinemia in near-term and term newborns. Pediatrics. 2004;113:775-780.
17. Shapiro-Mendoza CK, Tomashek K, Kotelchuck M, et al. Risk factors for neonatal morbidity and mortality among “healthy” late preterm newborns. Semin Perinatol. 2006;30:54-60.
18. Meier PP, Furman LM, Degenhardt M. Increased lactation risk for late preterm infants and mothers: evidence and management strategies to protect breastfeeding. J Midwifery Women’s Health. 2007;52:579-587.
19. American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316.
20. Thoyre S, Shaker CS, Pridham KF. The early feeding skills assessment for preterm infants. Neonatal Netw. 2005;24:7-16.
21. Adams-Chapman I. Neurodevelopmental outcomes of the late preterm infant. Clin Perinatol. 2006;33:947-964.
22. Morse SB, Zheng H, Tang Y, et al. Early school age outcomes of late preterm infants. Pediatrics. 2009;123:622-629.
23. Cohen-Wolkowiez M, Moran C, Benjamin D, et al. Early and late onset sepsis in late preterm infants. Pediatr Infect Dis J. 2009;28:1052-1056.
• Delay discharge of late preterm infants to a minimum of 48 hours to prevent readmission. B
• Perform transcutaneous or total serum bilirubin testing before discharging late preterm infants. C
• Perform a formal feeding assessment of breastfed infants prior to discharge. C
• Ensure that a follow-up appointment is made for 24 to 48 hours after discharge. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Laura M delivers her third baby at 35 weeks 4 days after an uneventful spontaneous labor. Julia, 5 lb 1 oz, has Apgar scores of 8 and 9. You see them on the mother-baby unit Friday afternoon, 36 hours after the delivery.
Ms. M has successfully breastfed her other 2 children and is planning to breastfeed Julia as well. She says the infant is nursing well today but seemed sleepy yesterday. The nursing notes say that Julia went to the nursery overnight because her mother was tired, and the infant spit up after receiving a formula bottle. Ms. M is asking you to discharge her because tomorrow is her son’s birthday. After considering this and her experience with breastfeeding, you decide to discharge her with follow-up on Monday instead of checking her out to your partner for the weekend.
Ms. M returns to your office on Monday with Julia, whose weight is down 10% and is “glowing yellow.” The baby is not latching well at the breast and is spitting up when Ms. M tries to supplement with formula. After examining Julia and checking lab work (bilirubin, 20 mg/dL), you decide to readmit her for feeding difficulties and hyperbilirubinemia.
Complications are common with late preterm infants, which refers to babies born between 34 weeks 0 days and 36 weeks 6 days of pregnancy. Between 1990 and 2006, there was a dramatic (25%) increase in the rate of late preterm infants in the United States, although more recently this number has leveled off.1
Several factors have been linked to increased late preterm births: maternal obesity, increased maternal age, and the increasing rate of multiple gestation pregnancies that have resulted from the expanded use of reproductive technology.2 Similarly, treatment of severe preeclampsia and premature rupture of membranes often includes delivery after 34 weeks of gestation,3 further contributing to the problem. Finally, higher rates of antenatal screening have contributed to more inductions and cesarean sections at earlier gestational ages. One study even found a correlation between higher malpractice premiums and more frequent late preterm inductions.4
Don’t let their appearance fool you
At first appearance, late preterm infants are similar to term infants in terms of Apgar scores,5 size, and weight.2 However, the care of these infants can be complex. They are often placed in well-infant nurseries under the same protocols as term infants and discharged before an adequate observation period. These infants have both increased short- and long-term morbidity and mortality and use a significant amount of health care resources.5 Morbidity in these infants decreases with each week of gestation from 34 weeks to a nadir at 39 weeks and can be unrelated to maternal and pregnancy complications.6
The following are some important issues to keep in mind when caring for these infants.
Hypothermia and hypoglycemia
Late preterm infants experience increased cold stress because of their limited fat stores, reduced brown fat, an immature epidermal barrier, and increased surface area to body mass ratio.2 Hypothermia increases the metabolic demands on the neonate and can worsen hypoglycemia as well as respiratory distress.7
Ideally, clinicians should dry these infants with warm blankets, place them skin-to-skin with their mother, and cover them with a warm blanket and cap to avoid excess energy expenditure.8 If conditions necessitate, neonates can be placed in a radiant warmer. Infants’ temperature needs to be monitored within the first 30 minutes of life and frequently reassessed during the first 12 hours of life—the “transition period.”8 The infant’s axillary temperature should be maintained between 36.5°C and 37.4°C (97.7-99.3°F); the temperature should remain stable in an open crib for the 12 hours before discharge.2
Decreased glycogen stores, increased glucose utilization, and immature hepatic enzymes help to explain the fact that hypoglycemia is 3 times more common in late preterm infants compared with full-term neonates.7 In all newborns, glucose levels decrease to their nadir between 30 and 90 minutes of life and normally trigger the breakdown of glycogen if the infant does not eat.7 Hypoglycemia can manifest as a change in level of consciousness, apnea, cyanosis, tachypnea, hypothermia, and seizures.9 The evidence is limited and there is controversy as to what level of hypoglycemia and over what duration of time is harmful.9
Most experts agree that breastfeeding should be started in the delivery room, and plasma glucose checked at 60 minutes of life and any time an infant is symptomatic. A level less than 45 mg/dL during the transition period should prompt feeding.9 Glucose levels should be rechecked within an hour of feeding and every 3 hours thereafter. If the level remains low or the infant is not interested in feeding, give a bolus of D10W and consider an infusion.7,10 TABLE 110 highlights one proposed method of glucose management.
TABLE 1
How best to manage glucose in a late preterm newborn10
| Asymptomatic late preterm infants | Glucose level (mg/dL) | Response |
|---|---|---|
| Check plasma glucose at 1 hour of life | <45 | Feed, recheck 1 h |
| Subsequent glucose monitoring | <35 | IV infusion* |
| >35 | Rescreen q3h for 36 h | |
| Symptomatic late preterm infants | ||
| Infusion for goal >55 mg/dL | <45 | Minibolus;† IV infusion* |
| *IV infusion=D10W at 6-8 mg/kg/min. †Minibolus=200 mg/kg D10W (2 mL/kg). Adapted with permission from: Macmillan Publishers Ltd. Adamkin DH. Late preterm infants: severe hyperbilirubinemia and postnatal glucose homeostasis. J Perinatol. 2009;29:S12-S17. Copyright 2009. | ||
Respiratory distress
At least 30% of late preterm infants will have some evidence of respiratory distress,5 which is defined as the need for oxygen supplementation due to tachypnea, grunting, nasal flaring, retractions, or cyanosis. Those at highest risk are white males born via cesarean section.11 Transient tachypnea of the newborn (TTN) appears to be the cause of almost half the cases of respiratory distress in these young patients.12 As this is a diagnosis by exclusion, consider other common causes: respiratory distress syndrome, neonatal pneumonia, meconium aspiration syndrome, and persistent pulmonary hypertension.12 The need for ventilator support is a significant concern in this group and increases exponentially with decreasing gestational age.6
Hyperbilirubinemia
More than half of all late preterm infants will present with clinically significant jaundice.5 Late preterm infants have an increased bilirubin load, decreased uptake of bilirubin, and delayed conjugation. They are less able to bind bilirubin to albumin, which increases their predisposition to bilirubin-induced neurological dysfunction and kernicterus.13 They also have more difficulty with breastfeeding, which exacerbates their hyperbilirubinemia.14
Infants born at 36 weeks have an 8-fold increased risk of developing severe hyperbilirubinemia (total serum bilirubin >20 mg/dL) than those born at 41 weeks,13 which explains why they are disproportionately represented in the US Pilot Kernicterus Registry.14 These infants can develop neurological sequelae at lower levels of bilirubin than their term counterparts and have less chance of complete recovery once intensive therapy has been implemented.14
The 2 main risk factors for severe hyperbilirubinemia have to do with discharge time and breastfeeding. Discharge at less than 48 hours is a risk factor for both term and late preterm infants.14,15 This is likely due to the fact that bilirubin peaks in late preterm infants between Days 5 and 7, and in term infants between Days 3 and 5.16 Difficulties with breastfeeding, the second risk factor,17 can be due to a combination of delayed maternal lactogenesis and ineffective milk removal on the part of the infant.18 When infants ingest smaller volumes of milk, bowel movements are infrequent and the bilirubin in the gut gets reabsorbed instead of excreted.
American Academy of Pediatrics (AAP) guidelines suggest measuring total serum bilirubin or transcutaneous bilirubin and plotting the value on an hour-specific, gestational-age-specific, risk-specific nomogram (FIGURE).19 Alternately, BiliTool (http://www.bilitool.org) can be used to individualize an infant’s risk.
FIGURE
Bilirubin levels and risk of significant hyperbilirubinemia19
Bilirubin levels should be plotted according to the infant’s hours of life and assessed according to risk factors on the appropriate risk line. If infants are 34 weeks 0 days to 34 weeks 6 days, they should be assessed on the high risk line.
- Use total bilirubin. Do not subtract direct reacting or conjugated bilirubin.
- Risk factors include isoimmune hemolytic disease, G6PD deficiency, asphyxia, significant lethargy, temperature instability, sepsis, acidosis, or albumin <3.0 g/dL (if measured).
- For well infants 35-37 6/7 weeks, you can adjust the total serum bilirubin (TSB) levels for intervention around the medium risk line. It is an option to intervene at lower TSB levels for infants closer to 35 weeks and at higher TSB levels for those closer to 37 6/7 weeks.
- It is an option to provide conventional phototherapy in the hospital or at home at TSB levels of 2-3 mg/dL (35-50 mmol/L) below those shown, but home phototherapy should not be used in any infant with risk factors.
Reprinted with permission from: American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316. Copyright © 2004 by the American Academy of Pediatrics.
Feeding difficulties
The advantages of breast milk feeding for these babies are great. Unfortunately, it is breastfed infants who are more likely to have feeding difficulties and are at higher risk for readmission.17 Early feeding skills are complex and challenging. Because of their immaturity, late preterm infants have less effective suck and swallow coordination. They can be sleepier and have less stamina.10 Infants require coordinated oral motor movements, breathing, and swallowing to avoid desaturation and aspiration.20 It is also important to note that almost every reported case of kernicterus in the past 20 years has been in breastfed infants whose feeding was not well established.13 First-born infants are especially at risk, as it takes longer to establish an adequate supply of milk.
For late preterm infants, it is imperative to establish successful breastfeeding to avoid dehydration and jaundice. Lactation consultation, education, and close follow-up are essential to successful breastfeeding in this group.18 The AAP Committee on Fetus and Newborn recommends a formal breastfeeding evaluation by trained caregivers at least twice daily prior to discharge.2
Brain injury
Late gestation is a critical period of brain growth. The 34-week-old brain weighs 65% of the term brain and increases linearly with each week. Fifty percent of the increase in cortical volume happens after 34 weeks.21 The risk of intraventricular hemorrhage and periventricular leukomalacia, while common in earlier preemies, is rare in infants born after 34 weeks. However, there is evidence to suggest other complications. Late preterm infants are more likely to be diagnosed with developmental delay and require special resources in preschool and less likely to be ready for school.22
Sepsis
While late preterm neonates do have a small but significant increase in culture-proven sepsis and pneumonia compared with term babies,6 the work-up for possible sepsis is 3 times more likely. When these infants have poor feeding, mild respiratory distress, or TTN, physicians become concerned about sepsis and initiate a work-up.5 Currently there are no management guidelines for sepsis evaluation in this subset of preterm infants.23
Readmission is a distinct possibility
One study of healthy late preterm infants showed a readmission rate of 4.8%. The most common reasons for readmission were jaundice and infection.17 Risk factors for readmission were breastfeeding, primiparity, labor and delivery complications, public payer source at delivery, and a mother of Asian/Pacific Islander ethnicity.17 Another study showed that discharge at less than 48 hours significantly increased the likelihood of readmission, even more so if the infant was breastfeeding.15
Several recent studies have highlighted a relationship between decreasing gestational age and a wide range of long-term adverse outcomes. In the early years of childhood, there is an increased risk for developmental delay and decreased kindergarten readiness.22 There is also a significant risk for disability, including cerebral palsy, mental retardation, and behavioral disorders.
Late preterm infants are at greater risk for several complications and the mortality rate is high in this group, when compared with term infants. By initial appearance and even weight, they rival their term counterparts. However, while they may look much like term babies and not weigh much less, they need more intense monitoring and should meet stringent discharge criteria (TABLE 22).
TABLE 2
Minimum discharge criteria for late preterm infants2
All criteria should be met prior to discharge.
|
| Adapted with permission from: Engle WA, Tomashek KM, Wallman C, Committee on Fetus and Newborn. “Late-preterm” infants: a population at risk. Pediatrics. 2007;120:1390-1401. Copyright © 2007 by the American Academy of Pediatrics. |
Clearly, more studies need to be done to address the unique needs and specific treatment guidelines for these infants. In fact, hospitals may need to consider introducing neonatal observation nurseries with protocols specifically tailored for late preterm infants.
CASE Ms. M and Julia likely would have been better served with an extra day in the hospital to address feeding issues and monitor for hyperbilirubinemia. Julia received phototherapy, IV fluids, and intensive lactation support, which included pumped breast milk given through a supplemental nursing system.
Over the course of 48 hours, her bilirubin decreased to 14 mg/dL and she was able to feed for longer periods of time without tiring. While both Ms. M and Julia’s initial outcomes were good, an extra day of feeding support may have prevented a readmission, thousands of dollars in care, and unnecessary stress on both mother and baby.
CORRESPONDENCE
Kimberly Stuckey-Schrock, MD, IU Health Goshen, Lincoln Avenue Family Medicine, 400 W Lincoln Avenue, Goshen, IN 46526; kstuckeyschr@iuhealth.org
• Delay discharge of late preterm infants to a minimum of 48 hours to prevent readmission. B
• Perform transcutaneous or total serum bilirubin testing before discharging late preterm infants. C
• Perform a formal feeding assessment of breastfed infants prior to discharge. C
• Ensure that a follow-up appointment is made for 24 to 48 hours after discharge. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Laura M delivers her third baby at 35 weeks 4 days after an uneventful spontaneous labor. Julia, 5 lb 1 oz, has Apgar scores of 8 and 9. You see them on the mother-baby unit Friday afternoon, 36 hours after the delivery.
Ms. M has successfully breastfed her other 2 children and is planning to breastfeed Julia as well. She says the infant is nursing well today but seemed sleepy yesterday. The nursing notes say that Julia went to the nursery overnight because her mother was tired, and the infant spit up after receiving a formula bottle. Ms. M is asking you to discharge her because tomorrow is her son’s birthday. After considering this and her experience with breastfeeding, you decide to discharge her with follow-up on Monday instead of checking her out to your partner for the weekend.
Ms. M returns to your office on Monday with Julia, whose weight is down 10% and is “glowing yellow.” The baby is not latching well at the breast and is spitting up when Ms. M tries to supplement with formula. After examining Julia and checking lab work (bilirubin, 20 mg/dL), you decide to readmit her for feeding difficulties and hyperbilirubinemia.
Complications are common with late preterm infants, which refers to babies born between 34 weeks 0 days and 36 weeks 6 days of pregnancy. Between 1990 and 2006, there was a dramatic (25%) increase in the rate of late preterm infants in the United States, although more recently this number has leveled off.1
Several factors have been linked to increased late preterm births: maternal obesity, increased maternal age, and the increasing rate of multiple gestation pregnancies that have resulted from the expanded use of reproductive technology.2 Similarly, treatment of severe preeclampsia and premature rupture of membranes often includes delivery after 34 weeks of gestation,3 further contributing to the problem. Finally, higher rates of antenatal screening have contributed to more inductions and cesarean sections at earlier gestational ages. One study even found a correlation between higher malpractice premiums and more frequent late preterm inductions.4
Don’t let their appearance fool you
At first appearance, late preterm infants are similar to term infants in terms of Apgar scores,5 size, and weight.2 However, the care of these infants can be complex. They are often placed in well-infant nurseries under the same protocols as term infants and discharged before an adequate observation period. These infants have both increased short- and long-term morbidity and mortality and use a significant amount of health care resources.5 Morbidity in these infants decreases with each week of gestation from 34 weeks to a nadir at 39 weeks and can be unrelated to maternal and pregnancy complications.6
The following are some important issues to keep in mind when caring for these infants.
Hypothermia and hypoglycemia
Late preterm infants experience increased cold stress because of their limited fat stores, reduced brown fat, an immature epidermal barrier, and increased surface area to body mass ratio.2 Hypothermia increases the metabolic demands on the neonate and can worsen hypoglycemia as well as respiratory distress.7
Ideally, clinicians should dry these infants with warm blankets, place them skin-to-skin with their mother, and cover them with a warm blanket and cap to avoid excess energy expenditure.8 If conditions necessitate, neonates can be placed in a radiant warmer. Infants’ temperature needs to be monitored within the first 30 minutes of life and frequently reassessed during the first 12 hours of life—the “transition period.”8 The infant’s axillary temperature should be maintained between 36.5°C and 37.4°C (97.7-99.3°F); the temperature should remain stable in an open crib for the 12 hours before discharge.2
Decreased glycogen stores, increased glucose utilization, and immature hepatic enzymes help to explain the fact that hypoglycemia is 3 times more common in late preterm infants compared with full-term neonates.7 In all newborns, glucose levels decrease to their nadir between 30 and 90 minutes of life and normally trigger the breakdown of glycogen if the infant does not eat.7 Hypoglycemia can manifest as a change in level of consciousness, apnea, cyanosis, tachypnea, hypothermia, and seizures.9 The evidence is limited and there is controversy as to what level of hypoglycemia and over what duration of time is harmful.9
Most experts agree that breastfeeding should be started in the delivery room, and plasma glucose checked at 60 minutes of life and any time an infant is symptomatic. A level less than 45 mg/dL during the transition period should prompt feeding.9 Glucose levels should be rechecked within an hour of feeding and every 3 hours thereafter. If the level remains low or the infant is not interested in feeding, give a bolus of D10W and consider an infusion.7,10 TABLE 110 highlights one proposed method of glucose management.
TABLE 1
How best to manage glucose in a late preterm newborn10
| Asymptomatic late preterm infants | Glucose level (mg/dL) | Response |
|---|---|---|
| Check plasma glucose at 1 hour of life | <45 | Feed, recheck 1 h |
| Subsequent glucose monitoring | <35 | IV infusion* |
| >35 | Rescreen q3h for 36 h | |
| Symptomatic late preterm infants | ||
| Infusion for goal >55 mg/dL | <45 | Minibolus;† IV infusion* |
| *IV infusion=D10W at 6-8 mg/kg/min. †Minibolus=200 mg/kg D10W (2 mL/kg). Adapted with permission from: Macmillan Publishers Ltd. Adamkin DH. Late preterm infants: severe hyperbilirubinemia and postnatal glucose homeostasis. J Perinatol. 2009;29:S12-S17. Copyright 2009. | ||
Respiratory distress
At least 30% of late preterm infants will have some evidence of respiratory distress,5 which is defined as the need for oxygen supplementation due to tachypnea, grunting, nasal flaring, retractions, or cyanosis. Those at highest risk are white males born via cesarean section.11 Transient tachypnea of the newborn (TTN) appears to be the cause of almost half the cases of respiratory distress in these young patients.12 As this is a diagnosis by exclusion, consider other common causes: respiratory distress syndrome, neonatal pneumonia, meconium aspiration syndrome, and persistent pulmonary hypertension.12 The need for ventilator support is a significant concern in this group and increases exponentially with decreasing gestational age.6
Hyperbilirubinemia
More than half of all late preterm infants will present with clinically significant jaundice.5 Late preterm infants have an increased bilirubin load, decreased uptake of bilirubin, and delayed conjugation. They are less able to bind bilirubin to albumin, which increases their predisposition to bilirubin-induced neurological dysfunction and kernicterus.13 They also have more difficulty with breastfeeding, which exacerbates their hyperbilirubinemia.14
Infants born at 36 weeks have an 8-fold increased risk of developing severe hyperbilirubinemia (total serum bilirubin >20 mg/dL) than those born at 41 weeks,13 which explains why they are disproportionately represented in the US Pilot Kernicterus Registry.14 These infants can develop neurological sequelae at lower levels of bilirubin than their term counterparts and have less chance of complete recovery once intensive therapy has been implemented.14
The 2 main risk factors for severe hyperbilirubinemia have to do with discharge time and breastfeeding. Discharge at less than 48 hours is a risk factor for both term and late preterm infants.14,15 This is likely due to the fact that bilirubin peaks in late preterm infants between Days 5 and 7, and in term infants between Days 3 and 5.16 Difficulties with breastfeeding, the second risk factor,17 can be due to a combination of delayed maternal lactogenesis and ineffective milk removal on the part of the infant.18 When infants ingest smaller volumes of milk, bowel movements are infrequent and the bilirubin in the gut gets reabsorbed instead of excreted.
American Academy of Pediatrics (AAP) guidelines suggest measuring total serum bilirubin or transcutaneous bilirubin and plotting the value on an hour-specific, gestational-age-specific, risk-specific nomogram (FIGURE).19 Alternately, BiliTool (http://www.bilitool.org) can be used to individualize an infant’s risk.
FIGURE
Bilirubin levels and risk of significant hyperbilirubinemia19
Bilirubin levels should be plotted according to the infant’s hours of life and assessed according to risk factors on the appropriate risk line. If infants are 34 weeks 0 days to 34 weeks 6 days, they should be assessed on the high risk line.
- Use total bilirubin. Do not subtract direct reacting or conjugated bilirubin.
- Risk factors include isoimmune hemolytic disease, G6PD deficiency, asphyxia, significant lethargy, temperature instability, sepsis, acidosis, or albumin <3.0 g/dL (if measured).
- For well infants 35-37 6/7 weeks, you can adjust the total serum bilirubin (TSB) levels for intervention around the medium risk line. It is an option to intervene at lower TSB levels for infants closer to 35 weeks and at higher TSB levels for those closer to 37 6/7 weeks.
- It is an option to provide conventional phototherapy in the hospital or at home at TSB levels of 2-3 mg/dL (35-50 mmol/L) below those shown, but home phototherapy should not be used in any infant with risk factors.
Reprinted with permission from: American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316. Copyright © 2004 by the American Academy of Pediatrics.
Feeding difficulties
The advantages of breast milk feeding for these babies are great. Unfortunately, it is breastfed infants who are more likely to have feeding difficulties and are at higher risk for readmission.17 Early feeding skills are complex and challenging. Because of their immaturity, late preterm infants have less effective suck and swallow coordination. They can be sleepier and have less stamina.10 Infants require coordinated oral motor movements, breathing, and swallowing to avoid desaturation and aspiration.20 It is also important to note that almost every reported case of kernicterus in the past 20 years has been in breastfed infants whose feeding was not well established.13 First-born infants are especially at risk, as it takes longer to establish an adequate supply of milk.
For late preterm infants, it is imperative to establish successful breastfeeding to avoid dehydration and jaundice. Lactation consultation, education, and close follow-up are essential to successful breastfeeding in this group.18 The AAP Committee on Fetus and Newborn recommends a formal breastfeeding evaluation by trained caregivers at least twice daily prior to discharge.2
Brain injury
Late gestation is a critical period of brain growth. The 34-week-old brain weighs 65% of the term brain and increases linearly with each week. Fifty percent of the increase in cortical volume happens after 34 weeks.21 The risk of intraventricular hemorrhage and periventricular leukomalacia, while common in earlier preemies, is rare in infants born after 34 weeks. However, there is evidence to suggest other complications. Late preterm infants are more likely to be diagnosed with developmental delay and require special resources in preschool and less likely to be ready for school.22
Sepsis
While late preterm neonates do have a small but significant increase in culture-proven sepsis and pneumonia compared with term babies,6 the work-up for possible sepsis is 3 times more likely. When these infants have poor feeding, mild respiratory distress, or TTN, physicians become concerned about sepsis and initiate a work-up.5 Currently there are no management guidelines for sepsis evaluation in this subset of preterm infants.23
Readmission is a distinct possibility
One study of healthy late preterm infants showed a readmission rate of 4.8%. The most common reasons for readmission were jaundice and infection.17 Risk factors for readmission were breastfeeding, primiparity, labor and delivery complications, public payer source at delivery, and a mother of Asian/Pacific Islander ethnicity.17 Another study showed that discharge at less than 48 hours significantly increased the likelihood of readmission, even more so if the infant was breastfeeding.15
Several recent studies have highlighted a relationship between decreasing gestational age and a wide range of long-term adverse outcomes. In the early years of childhood, there is an increased risk for developmental delay and decreased kindergarten readiness.22 There is also a significant risk for disability, including cerebral palsy, mental retardation, and behavioral disorders.
Late preterm infants are at greater risk for several complications and the mortality rate is high in this group, when compared with term infants. By initial appearance and even weight, they rival their term counterparts. However, while they may look much like term babies and not weigh much less, they need more intense monitoring and should meet stringent discharge criteria (TABLE 22).
TABLE 2
Minimum discharge criteria for late preterm infants2
All criteria should be met prior to discharge.
|
| Adapted with permission from: Engle WA, Tomashek KM, Wallman C, Committee on Fetus and Newborn. “Late-preterm” infants: a population at risk. Pediatrics. 2007;120:1390-1401. Copyright © 2007 by the American Academy of Pediatrics. |
Clearly, more studies need to be done to address the unique needs and specific treatment guidelines for these infants. In fact, hospitals may need to consider introducing neonatal observation nurseries with protocols specifically tailored for late preterm infants.
CASE Ms. M and Julia likely would have been better served with an extra day in the hospital to address feeding issues and monitor for hyperbilirubinemia. Julia received phototherapy, IV fluids, and intensive lactation support, which included pumped breast milk given through a supplemental nursing system.
Over the course of 48 hours, her bilirubin decreased to 14 mg/dL and she was able to feed for longer periods of time without tiring. While both Ms. M and Julia’s initial outcomes were good, an extra day of feeding support may have prevented a readmission, thousands of dollars in care, and unnecessary stress on both mother and baby.
CORRESPONDENCE
Kimberly Stuckey-Schrock, MD, IU Health Goshen, Lincoln Avenue Family Medicine, 400 W Lincoln Avenue, Goshen, IN 46526; kstuckeyschr@iuhealth.org
1. Martin JA, Hamilton BE, Sutton PD, et al. Birth: final data for 2008. Natl Vital Stat Rep. 2010;59:1, 3-71.
2. Engle WA, Tomashek KM, Wallman C. Committee on Fetus and Newborn. “Late-preterm” infants: a population at risk. Pediatrics. 2007;120:1390-1401.
3. Gabbe SG, Niebyl JR, Simpson JL. eds. Obstetrics Normal and Problem Pregnancies. Philadelphia, Pa: Churchill Livingstone; 2007.
4. Murthy K, Grobman WA, Lee TA, et al. Obstetricians’ rising liability insurance premiums and inductions at late preterm gestations. Med Care. 2009;47:425-430.
5. Wang ML, Dorer DJ, Fleming MP, et al. Clinical outcomes of near-term infants. Pediatrics. 2004;114:372-376.
6. Melamed N, Klinger G, Tenenbaum-Gavish K, et al. Short-term neonatal outcome in low-risk, spontaneous, singleton, late preterm deliveries. Obstet Gynecol. 2009;114:253-260.
7. Garg M, Devaskar SU. Glucose metabolism in the late preterm infant. Clin Perinatol. 2006;33:853-870.
8. Laptook A, Jackson G. Cold stress and hypoglycemia in the late preterm (“near-term”) infant: impact on nursery of admission. Semin Perinatol. 2006;30:24-27.
9. Cornblath M, Hawdon JM, Williams AF, et al. Controversies regarding definition of neonatal hypoglycemia: suggested operational thresholds. Pediatrics. 2000;105:1141-1145.
10. Adamkin D. Late preterm infants: severe hyperbilirubinemia and postnatal glucose homeostasis. J Perinatol. 2009;29(suppl):S12-S17.
11. Clark R. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol. 2005;25:251-257.
12. Kalyoncu O, Aygun C, Cetinoglu E, et al. Neonatal morbidity and mortality of late-preterm babies. J Matern Fetal Neonatal Med. 2010;23:607-612.
13. Watchko J. Hyperbilirubinemia and bilirubin toxicity in the late preterm infant. Clin Perinatol. 2006;33:839-852.
14. Bhutani V. Kernicterus in late preterm infants cared for as term healthy infants. Semin Perinatol. 2006;30:89-97.
15. Tomashek KM, Shapiro-Mendoza CK, Weiss J, et al. Early discharge among late preterm and term newborns and risk of neonatal morbidity. Semin Perinatol. 2006;30:61-68.
16. Sarici SU, Serdar MA, Korkmaz A, et al. Incidence, course, and prediction of hyperbilirubinemia in near-term and term newborns. Pediatrics. 2004;113:775-780.
17. Shapiro-Mendoza CK, Tomashek K, Kotelchuck M, et al. Risk factors for neonatal morbidity and mortality among “healthy” late preterm newborns. Semin Perinatol. 2006;30:54-60.
18. Meier PP, Furman LM, Degenhardt M. Increased lactation risk for late preterm infants and mothers: evidence and management strategies to protect breastfeeding. J Midwifery Women’s Health. 2007;52:579-587.
19. American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316.
20. Thoyre S, Shaker CS, Pridham KF. The early feeding skills assessment for preterm infants. Neonatal Netw. 2005;24:7-16.
21. Adams-Chapman I. Neurodevelopmental outcomes of the late preterm infant. Clin Perinatol. 2006;33:947-964.
22. Morse SB, Zheng H, Tang Y, et al. Early school age outcomes of late preterm infants. Pediatrics. 2009;123:622-629.
23. Cohen-Wolkowiez M, Moran C, Benjamin D, et al. Early and late onset sepsis in late preterm infants. Pediatr Infect Dis J. 2009;28:1052-1056.
1. Martin JA, Hamilton BE, Sutton PD, et al. Birth: final data for 2008. Natl Vital Stat Rep. 2010;59:1, 3-71.
2. Engle WA, Tomashek KM, Wallman C. Committee on Fetus and Newborn. “Late-preterm” infants: a population at risk. Pediatrics. 2007;120:1390-1401.
3. Gabbe SG, Niebyl JR, Simpson JL. eds. Obstetrics Normal and Problem Pregnancies. Philadelphia, Pa: Churchill Livingstone; 2007.
4. Murthy K, Grobman WA, Lee TA, et al. Obstetricians’ rising liability insurance premiums and inductions at late preterm gestations. Med Care. 2009;47:425-430.
5. Wang ML, Dorer DJ, Fleming MP, et al. Clinical outcomes of near-term infants. Pediatrics. 2004;114:372-376.
6. Melamed N, Klinger G, Tenenbaum-Gavish K, et al. Short-term neonatal outcome in low-risk, spontaneous, singleton, late preterm deliveries. Obstet Gynecol. 2009;114:253-260.
7. Garg M, Devaskar SU. Glucose metabolism in the late preterm infant. Clin Perinatol. 2006;33:853-870.
8. Laptook A, Jackson G. Cold stress and hypoglycemia in the late preterm (“near-term”) infant: impact on nursery of admission. Semin Perinatol. 2006;30:24-27.
9. Cornblath M, Hawdon JM, Williams AF, et al. Controversies regarding definition of neonatal hypoglycemia: suggested operational thresholds. Pediatrics. 2000;105:1141-1145.
10. Adamkin D. Late preterm infants: severe hyperbilirubinemia and postnatal glucose homeostasis. J Perinatol. 2009;29(suppl):S12-S17.
11. Clark R. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol. 2005;25:251-257.
12. Kalyoncu O, Aygun C, Cetinoglu E, et al. Neonatal morbidity and mortality of late-preterm babies. J Matern Fetal Neonatal Med. 2010;23:607-612.
13. Watchko J. Hyperbilirubinemia and bilirubin toxicity in the late preterm infant. Clin Perinatol. 2006;33:839-852.
14. Bhutani V. Kernicterus in late preterm infants cared for as term healthy infants. Semin Perinatol. 2006;30:89-97.
15. Tomashek KM, Shapiro-Mendoza CK, Weiss J, et al. Early discharge among late preterm and term newborns and risk of neonatal morbidity. Semin Perinatol. 2006;30:61-68.
16. Sarici SU, Serdar MA, Korkmaz A, et al. Incidence, course, and prediction of hyperbilirubinemia in near-term and term newborns. Pediatrics. 2004;113:775-780.
17. Shapiro-Mendoza CK, Tomashek K, Kotelchuck M, et al. Risk factors for neonatal morbidity and mortality among “healthy” late preterm newborns. Semin Perinatol. 2006;30:54-60.
18. Meier PP, Furman LM, Degenhardt M. Increased lactation risk for late preterm infants and mothers: evidence and management strategies to protect breastfeeding. J Midwifery Women’s Health. 2007;52:579-587.
19. American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316.
20. Thoyre S, Shaker CS, Pridham KF. The early feeding skills assessment for preterm infants. Neonatal Netw. 2005;24:7-16.
21. Adams-Chapman I. Neurodevelopmental outcomes of the late preterm infant. Clin Perinatol. 2006;33:947-964.
22. Morse SB, Zheng H, Tang Y, et al. Early school age outcomes of late preterm infants. Pediatrics. 2009;123:622-629.
23. Cohen-Wolkowiez M, Moran C, Benjamin D, et al. Early and late onset sepsis in late preterm infants. Pediatr Infect Dis J. 2009;28:1052-1056.