User login
Once you decide to expectantly manage a patient with preeclampsia, the balancing act begins. That means weighing fetal benefits against maternal risks, since the only justification for expectant management is to prolong pregnancy for fetal gain—there is no advantage to the mother.
The best approach is to classify the woman’s preeclampsia by the degree of severity and gestational age at the time of diagnosis, then follow recommendations tailored to that particular category.
This article offers guidelines for expectant management of mild and severe preeclampsia, preeclampsia superimposed on a preexisting medical condition, and intrapartum and postpartum care.
Mild preeclampsia
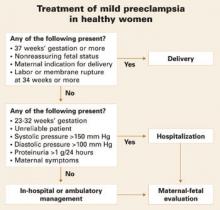
The earlier preeclampsia develops, the greater the risk it will become severe. The need for hospitalization depends on gestational age, blood pressure, proteinuria levels, maternal symptoms, and reliability of the patient.
Preeclampsia is mild when systolic blood pressure reaches 140 to 159 mm Hg or diastolic pressure measures 90 to 109 mm Hg on at least 2 occasions more than 6 hours apart after 20 weeks’ gestation in a woman who previously had normal blood pressure. In preeclampsia, this hypertension is accompanied by proteinuria of 0.3 to 4.9 g in a 24-hour urine sample (1+ or 2+ by dipstick on 2 occasions).
At or beyond 37 weeks’ gestation
In general, women diagnosed with preeclampsia at this gestational age have pregnancy outcomes similar to those of normotensive gravidas. Thus, they benefit from induction of labor and delivery.
32 to 36 weeks’ gestation
Close maternal and fetal evaluation is essential. (It is assumed these women have no labor or membrane rupture and normal fetal testing; otherwise, delivery is indicated at 34 weeks or beyond.)
In general, hospitalization is indicated when any of the following circumstances are present (FIGURE 1):
- the patient is unreliable,
- 2 or more systolic blood pressure readings exceed 150 mm Hg,
- 2 or more diastolic blood pressure readings exceed 100 mm Hg,
- proteinuria occurs at a rate exceeding 1 g/24 hours, or
- persistent maternal symptoms are present.
FIGURE 1 Treatment of mild preeclampsia in healthy women
Before 32 weeks’ gestation
These women are at high risk of progressing to severe disease. They also are more likely to have adverse perinatal outcomes such as intrauterine growth restriction (IUGR) (15% to 20%), preterm delivery (50%), and abruptio placentae (1% to 2%), compared with women diagnosed with preeclampsia at 32 to 36 weeks. In addition, they require more antenatal surveillance than women who develop preeclampsia later in pregnancy.
I recommend hospitalization at the time of diagnosis when women develop mild preeclampsia before 32 weeks.
What and when to monitor
Maternal evaluation should include:
- monitoring of blood pressure at least daily (at home or in the hospital),
- daily urine dipstick evaluation to monitor changes in proteinuria,
- twice-weekly platelet count and liver enzymes, and
- documentation of symptoms. (Instruct all women to report the onset of severe headaches, visual changes, altered mental status, epigastric or right upper quadrant pain, and any nausea or vomiting.)
Fetal evaluation should include:
- serial ultrasound every 3 weeks to estimate fetal weight and amniotic fluid status,
- nonstress testing every week, and
- daily fetal movement counts.
If a nonstress test is nonreactive, it should be confirmed by biophysical profile.
All testing should be promptly repeated if the maternal clinical condition deteriorates.
No need for bed rest, diuretics, or antihypertensive medications
Although expectantly managed patients with mild preeclampsia should be advised to restrict daily activity, there is no need for complete bed rest. Nor have diuretics or other antihypertensive drugs been shown to prolong gestation. On the contrary, these medications may mask severe preeclampsia.
Antihypertensive medications reduce the rate of severe hypertension but do not improve perinatal outcome. If these drugs are used to treat mild disease remote from term, hospitalize the patient and manage her as though she has severe preeclampsia.
Hospitalization versus outpatient management
Although she may be hospitalized at the time of diagnosis, a woman with preeclampsia may switch to outpatient management if systolic or diastolic blood pressure declines, proteinuria diminishes to 1 g/24 hours or less, and there are no maternal symptoms or evidence of severe IUGR. Otherwise, these women should remain hospitalized until delivery.
In cases that begin with outpatient management, prompt hospitalization is indicated if there is clinical evidence that the disease is progressing (ie, new symptoms, labor or rupture of membranes, vaginal bleeding, or increased blood pressures or proteinuria) or IUGR and/or oligohydramnios.
Instruct all women to report symptoms and changes in fetal movement.
When to deliver
Whether the gravida is hospitalized or an outpatient, delivery is indicated at 37 weeks. Earlier delivery may be warranted if nonreassuring maternal or fetal conditions develop. (FIGURE 1 summarizes management of mild preeclampsia.)
Severe preeclampsia
Expectant management is safe in properly selected women with severe disease, although maternal and fetal conditions can deteriorate. Hospitalization and daily monitoring are required.
Preeclampsia is severe when any of the following are present:
- systolic blood pressure of 160 mm Hg or higher or diastolic pressure of 110 mm Hg or above on 2 occasions at least 6 hours apart while the patient is on bed rest
- proteinuria of 5 g or more in a 24-hour urine specimen,
- oliguria of less than 500 mL in 24 hours,
- cerebral or visual disturbances,
- pulmonary edema or cyanosis,
- severe epigastric or right upper-quadrant pain, or
- thrombocytopenia.
When gestational hypertension or preeclampsia is severe, hospitalization in the labor and delivery suite is warranted. These women should receive intravenous (IV) magnesium sulfate to reduce the risk of convulsions and antihypertensive drugs to treat severe levels of hypertension, if present. The aim of antihypertensive treatment is to keep diastolic blood pressure between 90 and 105 mm Hg and systolic blood pressure below 160 mm Hg.
During observation, assess maternal and fetal conditions and decide whether delivery is indicated (FIGURE 2).
Expectant management is warranted only for gestations between 23 and 32 weeks’ gestation, provided maternal and fetal conditions are stable (FIGURE 2).
Keep in mind that both maternal and fetal conditions may progressively deteriorate. Thus, these pregnancies involve higher rates of maternal morbidity and significant risk of neonatal morbidity. For this reason, expectant management should proceed only in a tertiary-care center with adequate maternal and neonatal facilities.
Recommended counseling
Advise these patients of the potential risks and benefits of expectant management, which requires daily monitoring of maternal and fetal conditions. Also explain that the decision to continue expectant management will be revisited on a daily basis and that the median number of days pregnancy is prolonged in these cases is 7 (range 2 to 35).
Another important fact to relay: Only 2 randomized trials involving 133 women have compared expectant management to aggressive management in early-onset preeclampsia. However, retrospective and observational studies involving more than 700 women suggest expectant management reduces short-term neonatal morbidity with minimal risk to the mother.
Superimposed preeclampsia
Women who develop preeclampsia on top of chronic hypertension, renal disease, or type 1 diabetes have a markedly higher risk of morbidity, including perinatal morbidity, than women without preexisting conditions.
Women with superimposed preeclampsia may be managed in the hospital, since these pregnancies are associated with higher rates of abruptio placentae (2% to 5%), preterm delivery (56%), IUGR (13% to 15%), and perinatal death (8%). Thus, these women benefit from very close maternal and fetal monitoring.
Superimposed preeclampsia is not classified according to severity.
In general, maternal and perinatal morbidities are substantially higher in women who have preexisting conditions than in healthy women who develop preeclampsia.
Chronic hypertension
Indications for delivery are similar to those described for healthy women with preeclampsia, as is antihypertensive therapy.
If the woman develops preeclampsia while using antihypertensive drugs, delivery should be considered beyond 34 weeks’ gestation.
How preeclampsia affects renal function
Women with renal disease or dysfunction (serum creatinine ≥1.2 mg/dL) prior to or early in pregnancy face an increased risk of adverse neonatal outcomes, regardless of whether preeclampsia also develops. These women also face an increased risk of deteriorating renal function during pregnancy (particularly if preeclampsia or severe hypertension develops) and beyond (more than 6 months postpartum).
Start antihypertensive medications as soon as possible, with the goal of keeping systolic blood pressure below 140 mm Hg and diastolic blood pressure below 90 mm Hg throughout gestation.
Delivery is indicated with the onset of preeclampsia or significant deterioration in renal function.
Diabetes warrants aggressive therapy
Women with type 1 diabetes have a higher risk of preeclampsia, maternal and fetal morbidity, and perinatal mortality. These risks multiply in women who have hypertension and/or diabetic nephropathy. Worsening of retinopathy and nephropathy also is more likely in women who have hypertension. Thus, aggressive management of blood sugars with insulin should be accompanied by aggressive control of blood pressure, with the goal of keeping systolic pressure below 130 mm Hg and diastolic pressure below 85 mm Hg.
Choosing antihypertensive drugs. Calcium-channel blockers are preferred to control blood pressure during pregnancy in women with diabetes. Outside of pregnancy, angiotensin-converting enzyme (ACE) inhibitors are best to avert long-term complications, but avoid these drugs in pregnancy (along with angiotensin-receptor blockers), particularly beyond 16 weeks.
Delivery is indicated in all women with vascular diabetes mellitus beyond 34 weeks when preeclampsia is present.
Intrapartum management
Close fetal heart rate and maternal blood pressure monitoring are mainstays, along with magnesium sulfate and antihypertensive therapy.
All women with preeclampsia should receive continuous monitoring of fetal heart rate and uterine activity, with special vigilance for hyperstimulation and onset of vaginal bleeding during labor. (For a description of potential maternal complications, see TABLE 1; fetal complications are described in FIGURE 3.)
Uterine irritability, recurrent variable or late decelerations, and the development of vaginal bleeding may be the first signs of abruptio placentae.
I recommend recording maternal blood pressure at least hourly to detect progression from mild to severe hypertension and to determine the need for antihypertensive therapy.
TABLE 1
Likelihood of maternal complications
| Disease progresses during labor (from mild to severe) | 10% |
| Eclampsia | |
| • Mild disease | <0.5% |
| • Severe preeclampsia | 1–2% |
| Stroke (encephalopathy or hemorrhage) | <1% |
| Mainly with severe or early onset disease | |
| Pulmonary edema | 1–2% |
| Usually associated with fluid overload or long-standing chronic hypertension | |
Prevent progression to eclampsia
Magnesium sulfate is the drug of choice in women with preeclampsia. Recent reviews indicate that it reduces the rate of convulsions from 2% to 0.6% in women with severe preeclampsia. In women with mild preeclampsia, the benefit of magnesium sulfate remains unclear.
I recommend IV magnesium sulfate during labor and postpartum when a woman has the indications listed in TABLE 2.
The dose of magnesium sulfate is 6 g IV loading over 20 minutes, followed by a maintenance dose of 2 g/hour.
Magnesium sulfate should be started before surgery (elective cesarean delivery) and continued for at least 12 hours postpartum (I prefer 24 hours).
TABLE 2
When to give prophylactic magnesium sulfate
| Use intrapartum and for at least 12 hours postpartum |
|---|
When the patient has:
|
When treating hypertension in labor, avoid “hypotensive overshoot”
The goal of intrapartum treatment is to lower maternal blood pressure without causing precipitous hypotensive overshoot that may lead to reduced maternal organ perfusion, particularly uteroplacental blood flow. Such acute lowering of maternal blood pressure is a common cause of nonreassuring fetal heart rate patterns during labor.
What blood pressure necessitates treatment? There is no doubt that severe levels of hypertension should be treated to avoid potential cerebrovascular and cardiovascular complications in healthy women. However, there is disagreement about what constitutes severe hypertension.
In previously healthy women, I recommend antihypertensive therapy for systolic pressures of 170 mm Hg or above and/or for diastolic pressures of 110 mm Hg or above.
For women with thrombocytopenia, disseminated intravascular coagulation, or pulmonary edema, I recommend treatment for systolic pressures of 160 mm Hg or above and diastolic pressures of 105 mm Hg or above. This latter group should also be given IV furosemide (20 to 40 mg) to promote diuresis. I also recommend treatment at these levels in the postpartum period.
For women with diabetes, renal disease, or left ventricular cardiac disease, antihypertensive medications should be used to keep systolic pressure below 140 mm Hg and diastolic pressure below 90 mm Hg during labor and postpartum. Further, patients in congestive heart failure or with left ventricular diastolic dysfunction should receive furosemide in addition to antihypertensive drugs.
Choosing a drug. My drugs of choice are IV labetalol and oral nifedipine. These 2 drugs, along with IV hydralazine, are the most commonly recommended medications for severe hypertension in pregnancy (TABLE 3).
Although many authorities prefer hydralazine, recent data indicate that, compared with IV labetalol and oral nifedipine, IV hydralazine is associated with more maternal side effects and worse perinatal outcomes (more fetal distress in labor).
TABLE 3
Drug profiles: Dosing and side effects of antihypertensives used in pregnancy
| MEDICATION | ONSET OF ACTION | DOSE | SIDE EFFECTS |
|---|---|---|---|
| Hydralazine | 10-20 minutes | 5-10 mg intravenously every 20 minutes up to maximum dose of 30 mg | More maternal side effects and worse perinatal outcomes than labetalol or nifedipine. |
| Skin blisters; chest pain; general feeling of discomfort, illness, or weakness; joint or muscle pain; sore throat and fever; swollen lymph glands | |||
| Labetalol* | 10-15 minutes | 10-20 mg intravenously, then 40-80 mg every 10 minutes up to maximum dose of 220 mg/hour or continuous infusion of 1-2 mg/minute | Breathing difficulty and/or wheezing, cold hands and feet, mental depression, shortness of breath, slow heartbeat, swelling of lower extremities, back or joint pain, chest pain, confusion, fever and sore throat, hallucinations, irregular heartbeat, unusual bleeding and bruising, yellow eyes or skin |
| Nifedipine | 5-10 minutes | 10-20 mg orally, repeated in 30 minutes, up to maximum dose of 50 mg/hour | Breathing difficulty, coughing, or wheezing; irregular or fast, poundingheartbeat; skin rash; swelling of lower extremities; chest pain; fainting; painful, swollen joints; vision impairment |
| Sodium nitroprusside† | 0.5-5 minutes | 0.25-5 μg/kg/minute by intravenous infusion | Risk of fetal cyanide poisoning with prolonged treatment. |
| Maternal effects include symptoms of hypothyroidism, headache, abdominal pain, drowsiness, nausea, involuntary muscle movements, perspiration, restlessness, paraesthesia, palpitations, dizziness, retching, tachycardia | |||
| *In women with asthma and congestive heart failure | |||
| †Rarely needed except in hypertensive encephalopathy or cerebral hemorrhage | |||
Postpartum management
Because preeclampsia can worsen, or first appear, in the postpartum period, extra vigilance is important, and pharmacotherapy may be appropriate.
Management of preeclampsia does not end with delivery of the fetus and the placenta. These events do signal the beginning of the curative process, but complications can occur in the postpartum period. Indeed, in some women, the disease process worsens immediately postpartum. Therefore, women with diagnosed preeclampsia or severe gestational hypertension require close monitoring of blood pressure and maternal symptoms and accurate measurement of fluid intake and urine output. Some of these women are at increased risk for pulmonary edema; exacerbation of severe hypertension; eclampsia; and hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome.
Treating postpartum hypertension
Women who continue to have severe hypertension (systolic pressure at or above 155 mm Hg or diastolic pressure of 105 mm Hg or higher) will benefit from oral nifedipine (10 mg every 6 hours) or long-acting nifedipine (10 to 20 mg twice daily), the drugs of choice because of their favorable effects on renal function.
Women with severe hypertension also may require diuretics for better control of blood pressure, as may women with a history of congestive heart failure or left ventricular dysfunction.
Start women with vascular diabetes mellitus or diabetic nephropathy on ACE inhibitors immediately postpartum.
Patients can be discharged home once blood pressure is stable, provided there are no maternal symptoms of preeclampsia.
Postpartum preeclampsia can develop even in healthy women
Because severe hypertension or preeclampsia may develop for the first time in the postpartum period, it is important to educate all gravidas about the signs and symptoms. All health-care providers should be on the lookout for these symptoms as well.
The author reports no financial relationships relevant to this article.
BIBLIOGRAPHY
Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev (England). 2001;(2)pCD002252.-
Alfirevic Z, Roberts D, Martlew V. How strong is the association between maternal thrombophilia and adverse pregnancy outcome? A systematic review. Eur J Obstet Gynecol Reprod Biol. 2002;101:6-14.
Amorim MMR, Santas LC, Faundes A. Corticosteroid therapy for prevention of respiratory distress syndrome in severe preeclampsia. Am J Obstet Gynecol. 1999;180:1283-1288.
Duley L, Galmezoglu AM, Henderson-Smart DJ. Magnesium sulfate and other anticonvulsants for women with preeclampsia. Cochrane Database Syst Rev (England). 2003;(2)pCD000025.-
Friedman SA, Lubarsky S, Schiff E. Expectant management of severe preeclampsia remote from term. Clin Obstet Gynecol. 1999;42:470-478.
Haddad B, Deis S, Goffinet F, et al. Maternal and perinatal outcomes during expectant management of 239 severe preeclamptic women between 24 and 33 weeks’ gestation. Am J Obstet Gynecol. 2004;190:1590-1597.
Hall DR, Odendaal HJ, Kirten GF, Smith J. Expectant management of early onset, severe preeclampsia, perinatal outcome. BJOG. 2000;107:1258-1264.
Kupferminc MJ, Fait G, Many A, et al. Low molecular weight heparin for the prevention of obstetric complications in women with thrombophilia. Hypertension in Pregnancy. 2001;20:35-44.
Kupferminc MJ. Thrombophilia and pregnancy. Reprod Biol Endocrinol. 2003;1:111-166.
Magee LA, Cham C, Waterman EJ, Ohlsson A, Von Dadelszen P. Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003;327:1-10.
Magee LA, Ornstein MP, Von Dadelszen P. Fortnightly review: management of hypertension in pregnancy. BMJ. 1999;318:1332-1336.
Magpie Trial Group. Do women with preeclampsia, and their babies, benefit from magnesium sulfate? The Magpie Trial: a randomised, placebo-controlled trial. Lancet. 2002;359:1877-1890.
Report of the National High Blood Pressure Education Program. Working group report on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000;183:S1-22.
Sibai BM. Chronic hypertension in pregnancy. Obstet Gynecol. 2002;100:369-377.
Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003;102:181-192.
Sibai BM, Lindheimer MD, Hauth J, et al. Risk factors for preeclampsia, abruptio placentae, and adverse neonatal outcomes among women with chronic hypertension. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;229:667-671.
Sibai BM. Magnesium sulfate prophylaxis in preeclampsia. Lessons learned from recent trials. Am J Obstet Gynecol. 2004;190:1520-1526.
Vigil-DeGracia P, Montufar-Rueda C, Ruiz J. Expectant management of severe preeclampsia and preeclampsia superimposed on chronic hypertension between 24 and 34 weeks’ gestation. Eur J Obstet Gynecol Reprod Biol. 2003;107:24-27.
Once you decide to expectantly manage a patient with preeclampsia, the balancing act begins. That means weighing fetal benefits against maternal risks, since the only justification for expectant management is to prolong pregnancy for fetal gain—there is no advantage to the mother.
The best approach is to classify the woman’s preeclampsia by the degree of severity and gestational age at the time of diagnosis, then follow recommendations tailored to that particular category.
This article offers guidelines for expectant management of mild and severe preeclampsia, preeclampsia superimposed on a preexisting medical condition, and intrapartum and postpartum care.
Mild preeclampsia
The earlier preeclampsia develops, the greater the risk it will become severe. The need for hospitalization depends on gestational age, blood pressure, proteinuria levels, maternal symptoms, and reliability of the patient.
Preeclampsia is mild when systolic blood pressure reaches 140 to 159 mm Hg or diastolic pressure measures 90 to 109 mm Hg on at least 2 occasions more than 6 hours apart after 20 weeks’ gestation in a woman who previously had normal blood pressure. In preeclampsia, this hypertension is accompanied by proteinuria of 0.3 to 4.9 g in a 24-hour urine sample (1+ or 2+ by dipstick on 2 occasions).
At or beyond 37 weeks’ gestation
In general, women diagnosed with preeclampsia at this gestational age have pregnancy outcomes similar to those of normotensive gravidas. Thus, they benefit from induction of labor and delivery.
32 to 36 weeks’ gestation
Close maternal and fetal evaluation is essential. (It is assumed these women have no labor or membrane rupture and normal fetal testing; otherwise, delivery is indicated at 34 weeks or beyond.)
In general, hospitalization is indicated when any of the following circumstances are present (FIGURE 1):
- the patient is unreliable,
- 2 or more systolic blood pressure readings exceed 150 mm Hg,
- 2 or more diastolic blood pressure readings exceed 100 mm Hg,
- proteinuria occurs at a rate exceeding 1 g/24 hours, or
- persistent maternal symptoms are present.
FIGURE 1 Treatment of mild preeclampsia in healthy women
Before 32 weeks’ gestation
These women are at high risk of progressing to severe disease. They also are more likely to have adverse perinatal outcomes such as intrauterine growth restriction (IUGR) (15% to 20%), preterm delivery (50%), and abruptio placentae (1% to 2%), compared with women diagnosed with preeclampsia at 32 to 36 weeks. In addition, they require more antenatal surveillance than women who develop preeclampsia later in pregnancy.
I recommend hospitalization at the time of diagnosis when women develop mild preeclampsia before 32 weeks.
What and when to monitor
Maternal evaluation should include:
- monitoring of blood pressure at least daily (at home or in the hospital),
- daily urine dipstick evaluation to monitor changes in proteinuria,
- twice-weekly platelet count and liver enzymes, and
- documentation of symptoms. (Instruct all women to report the onset of severe headaches, visual changes, altered mental status, epigastric or right upper quadrant pain, and any nausea or vomiting.)
Fetal evaluation should include:
- serial ultrasound every 3 weeks to estimate fetal weight and amniotic fluid status,
- nonstress testing every week, and
- daily fetal movement counts.
If a nonstress test is nonreactive, it should be confirmed by biophysical profile.
All testing should be promptly repeated if the maternal clinical condition deteriorates.
No need for bed rest, diuretics, or antihypertensive medications
Although expectantly managed patients with mild preeclampsia should be advised to restrict daily activity, there is no need for complete bed rest. Nor have diuretics or other antihypertensive drugs been shown to prolong gestation. On the contrary, these medications may mask severe preeclampsia.
Antihypertensive medications reduce the rate of severe hypertension but do not improve perinatal outcome. If these drugs are used to treat mild disease remote from term, hospitalize the patient and manage her as though she has severe preeclampsia.
Hospitalization versus outpatient management
Although she may be hospitalized at the time of diagnosis, a woman with preeclampsia may switch to outpatient management if systolic or diastolic blood pressure declines, proteinuria diminishes to 1 g/24 hours or less, and there are no maternal symptoms or evidence of severe IUGR. Otherwise, these women should remain hospitalized until delivery.
In cases that begin with outpatient management, prompt hospitalization is indicated if there is clinical evidence that the disease is progressing (ie, new symptoms, labor or rupture of membranes, vaginal bleeding, or increased blood pressures or proteinuria) or IUGR and/or oligohydramnios.
Instruct all women to report symptoms and changes in fetal movement.
When to deliver
Whether the gravida is hospitalized or an outpatient, delivery is indicated at 37 weeks. Earlier delivery may be warranted if nonreassuring maternal or fetal conditions develop. (FIGURE 1 summarizes management of mild preeclampsia.)
Severe preeclampsia
Expectant management is safe in properly selected women with severe disease, although maternal and fetal conditions can deteriorate. Hospitalization and daily monitoring are required.
Preeclampsia is severe when any of the following are present:
- systolic blood pressure of 160 mm Hg or higher or diastolic pressure of 110 mm Hg or above on 2 occasions at least 6 hours apart while the patient is on bed rest
- proteinuria of 5 g or more in a 24-hour urine specimen,
- oliguria of less than 500 mL in 24 hours,
- cerebral or visual disturbances,
- pulmonary edema or cyanosis,
- severe epigastric or right upper-quadrant pain, or
- thrombocytopenia.
When gestational hypertension or preeclampsia is severe, hospitalization in the labor and delivery suite is warranted. These women should receive intravenous (IV) magnesium sulfate to reduce the risk of convulsions and antihypertensive drugs to treat severe levels of hypertension, if present. The aim of antihypertensive treatment is to keep diastolic blood pressure between 90 and 105 mm Hg and systolic blood pressure below 160 mm Hg.
During observation, assess maternal and fetal conditions and decide whether delivery is indicated (FIGURE 2).
Expectant management is warranted only for gestations between 23 and 32 weeks’ gestation, provided maternal and fetal conditions are stable (FIGURE 2).
Keep in mind that both maternal and fetal conditions may progressively deteriorate. Thus, these pregnancies involve higher rates of maternal morbidity and significant risk of neonatal morbidity. For this reason, expectant management should proceed only in a tertiary-care center with adequate maternal and neonatal facilities.
Recommended counseling
Advise these patients of the potential risks and benefits of expectant management, which requires daily monitoring of maternal and fetal conditions. Also explain that the decision to continue expectant management will be revisited on a daily basis and that the median number of days pregnancy is prolonged in these cases is 7 (range 2 to 35).
Another important fact to relay: Only 2 randomized trials involving 133 women have compared expectant management to aggressive management in early-onset preeclampsia. However, retrospective and observational studies involving more than 700 women suggest expectant management reduces short-term neonatal morbidity with minimal risk to the mother.
Superimposed preeclampsia
Women who develop preeclampsia on top of chronic hypertension, renal disease, or type 1 diabetes have a markedly higher risk of morbidity, including perinatal morbidity, than women without preexisting conditions.
Women with superimposed preeclampsia may be managed in the hospital, since these pregnancies are associated with higher rates of abruptio placentae (2% to 5%), preterm delivery (56%), IUGR (13% to 15%), and perinatal death (8%). Thus, these women benefit from very close maternal and fetal monitoring.
Superimposed preeclampsia is not classified according to severity.
In general, maternal and perinatal morbidities are substantially higher in women who have preexisting conditions than in healthy women who develop preeclampsia.
Chronic hypertension
Indications for delivery are similar to those described for healthy women with preeclampsia, as is antihypertensive therapy.
If the woman develops preeclampsia while using antihypertensive drugs, delivery should be considered beyond 34 weeks’ gestation.
How preeclampsia affects renal function
Women with renal disease or dysfunction (serum creatinine ≥1.2 mg/dL) prior to or early in pregnancy face an increased risk of adverse neonatal outcomes, regardless of whether preeclampsia also develops. These women also face an increased risk of deteriorating renal function during pregnancy (particularly if preeclampsia or severe hypertension develops) and beyond (more than 6 months postpartum).
Start antihypertensive medications as soon as possible, with the goal of keeping systolic blood pressure below 140 mm Hg and diastolic blood pressure below 90 mm Hg throughout gestation.
Delivery is indicated with the onset of preeclampsia or significant deterioration in renal function.
Diabetes warrants aggressive therapy
Women with type 1 diabetes have a higher risk of preeclampsia, maternal and fetal morbidity, and perinatal mortality. These risks multiply in women who have hypertension and/or diabetic nephropathy. Worsening of retinopathy and nephropathy also is more likely in women who have hypertension. Thus, aggressive management of blood sugars with insulin should be accompanied by aggressive control of blood pressure, with the goal of keeping systolic pressure below 130 mm Hg and diastolic pressure below 85 mm Hg.
Choosing antihypertensive drugs. Calcium-channel blockers are preferred to control blood pressure during pregnancy in women with diabetes. Outside of pregnancy, angiotensin-converting enzyme (ACE) inhibitors are best to avert long-term complications, but avoid these drugs in pregnancy (along with angiotensin-receptor blockers), particularly beyond 16 weeks.
Delivery is indicated in all women with vascular diabetes mellitus beyond 34 weeks when preeclampsia is present.
Intrapartum management
Close fetal heart rate and maternal blood pressure monitoring are mainstays, along with magnesium sulfate and antihypertensive therapy.
All women with preeclampsia should receive continuous monitoring of fetal heart rate and uterine activity, with special vigilance for hyperstimulation and onset of vaginal bleeding during labor. (For a description of potential maternal complications, see TABLE 1; fetal complications are described in FIGURE 3.)
Uterine irritability, recurrent variable or late decelerations, and the development of vaginal bleeding may be the first signs of abruptio placentae.
I recommend recording maternal blood pressure at least hourly to detect progression from mild to severe hypertension and to determine the need for antihypertensive therapy.
TABLE 1
Likelihood of maternal complications
| Disease progresses during labor (from mild to severe) | 10% |
| Eclampsia | |
| • Mild disease | <0.5% |
| • Severe preeclampsia | 1–2% |
| Stroke (encephalopathy or hemorrhage) | <1% |
| Mainly with severe or early onset disease | |
| Pulmonary edema | 1–2% |
| Usually associated with fluid overload or long-standing chronic hypertension | |
Prevent progression to eclampsia
Magnesium sulfate is the drug of choice in women with preeclampsia. Recent reviews indicate that it reduces the rate of convulsions from 2% to 0.6% in women with severe preeclampsia. In women with mild preeclampsia, the benefit of magnesium sulfate remains unclear.
I recommend IV magnesium sulfate during labor and postpartum when a woman has the indications listed in TABLE 2.
The dose of magnesium sulfate is 6 g IV loading over 20 minutes, followed by a maintenance dose of 2 g/hour.
Magnesium sulfate should be started before surgery (elective cesarean delivery) and continued for at least 12 hours postpartum (I prefer 24 hours).
TABLE 2
When to give prophylactic magnesium sulfate
| Use intrapartum and for at least 12 hours postpartum |
|---|
When the patient has:
|
When treating hypertension in labor, avoid “hypotensive overshoot”
The goal of intrapartum treatment is to lower maternal blood pressure without causing precipitous hypotensive overshoot that may lead to reduced maternal organ perfusion, particularly uteroplacental blood flow. Such acute lowering of maternal blood pressure is a common cause of nonreassuring fetal heart rate patterns during labor.
What blood pressure necessitates treatment? There is no doubt that severe levels of hypertension should be treated to avoid potential cerebrovascular and cardiovascular complications in healthy women. However, there is disagreement about what constitutes severe hypertension.
In previously healthy women, I recommend antihypertensive therapy for systolic pressures of 170 mm Hg or above and/or for diastolic pressures of 110 mm Hg or above.
For women with thrombocytopenia, disseminated intravascular coagulation, or pulmonary edema, I recommend treatment for systolic pressures of 160 mm Hg or above and diastolic pressures of 105 mm Hg or above. This latter group should also be given IV furosemide (20 to 40 mg) to promote diuresis. I also recommend treatment at these levels in the postpartum period.
For women with diabetes, renal disease, or left ventricular cardiac disease, antihypertensive medications should be used to keep systolic pressure below 140 mm Hg and diastolic pressure below 90 mm Hg during labor and postpartum. Further, patients in congestive heart failure or with left ventricular diastolic dysfunction should receive furosemide in addition to antihypertensive drugs.
Choosing a drug. My drugs of choice are IV labetalol and oral nifedipine. These 2 drugs, along with IV hydralazine, are the most commonly recommended medications for severe hypertension in pregnancy (TABLE 3).
Although many authorities prefer hydralazine, recent data indicate that, compared with IV labetalol and oral nifedipine, IV hydralazine is associated with more maternal side effects and worse perinatal outcomes (more fetal distress in labor).
TABLE 3
Drug profiles: Dosing and side effects of antihypertensives used in pregnancy
| MEDICATION | ONSET OF ACTION | DOSE | SIDE EFFECTS |
|---|---|---|---|
| Hydralazine | 10-20 minutes | 5-10 mg intravenously every 20 minutes up to maximum dose of 30 mg | More maternal side effects and worse perinatal outcomes than labetalol or nifedipine. |
| Skin blisters; chest pain; general feeling of discomfort, illness, or weakness; joint or muscle pain; sore throat and fever; swollen lymph glands | |||
| Labetalol* | 10-15 minutes | 10-20 mg intravenously, then 40-80 mg every 10 minutes up to maximum dose of 220 mg/hour or continuous infusion of 1-2 mg/minute | Breathing difficulty and/or wheezing, cold hands and feet, mental depression, shortness of breath, slow heartbeat, swelling of lower extremities, back or joint pain, chest pain, confusion, fever and sore throat, hallucinations, irregular heartbeat, unusual bleeding and bruising, yellow eyes or skin |
| Nifedipine | 5-10 minutes | 10-20 mg orally, repeated in 30 minutes, up to maximum dose of 50 mg/hour | Breathing difficulty, coughing, or wheezing; irregular or fast, poundingheartbeat; skin rash; swelling of lower extremities; chest pain; fainting; painful, swollen joints; vision impairment |
| Sodium nitroprusside† | 0.5-5 minutes | 0.25-5 μg/kg/minute by intravenous infusion | Risk of fetal cyanide poisoning with prolonged treatment. |
| Maternal effects include symptoms of hypothyroidism, headache, abdominal pain, drowsiness, nausea, involuntary muscle movements, perspiration, restlessness, paraesthesia, palpitations, dizziness, retching, tachycardia | |||
| *In women with asthma and congestive heart failure | |||
| †Rarely needed except in hypertensive encephalopathy or cerebral hemorrhage | |||
Postpartum management
Because preeclampsia can worsen, or first appear, in the postpartum period, extra vigilance is important, and pharmacotherapy may be appropriate.
Management of preeclampsia does not end with delivery of the fetus and the placenta. These events do signal the beginning of the curative process, but complications can occur in the postpartum period. Indeed, in some women, the disease process worsens immediately postpartum. Therefore, women with diagnosed preeclampsia or severe gestational hypertension require close monitoring of blood pressure and maternal symptoms and accurate measurement of fluid intake and urine output. Some of these women are at increased risk for pulmonary edema; exacerbation of severe hypertension; eclampsia; and hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome.
Treating postpartum hypertension
Women who continue to have severe hypertension (systolic pressure at or above 155 mm Hg or diastolic pressure of 105 mm Hg or higher) will benefit from oral nifedipine (10 mg every 6 hours) or long-acting nifedipine (10 to 20 mg twice daily), the drugs of choice because of their favorable effects on renal function.
Women with severe hypertension also may require diuretics for better control of blood pressure, as may women with a history of congestive heart failure or left ventricular dysfunction.
Start women with vascular diabetes mellitus or diabetic nephropathy on ACE inhibitors immediately postpartum.
Patients can be discharged home once blood pressure is stable, provided there are no maternal symptoms of preeclampsia.
Postpartum preeclampsia can develop even in healthy women
Because severe hypertension or preeclampsia may develop for the first time in the postpartum period, it is important to educate all gravidas about the signs and symptoms. All health-care providers should be on the lookout for these symptoms as well.
The author reports no financial relationships relevant to this article.
Once you decide to expectantly manage a patient with preeclampsia, the balancing act begins. That means weighing fetal benefits against maternal risks, since the only justification for expectant management is to prolong pregnancy for fetal gain—there is no advantage to the mother.
The best approach is to classify the woman’s preeclampsia by the degree of severity and gestational age at the time of diagnosis, then follow recommendations tailored to that particular category.
This article offers guidelines for expectant management of mild and severe preeclampsia, preeclampsia superimposed on a preexisting medical condition, and intrapartum and postpartum care.
Mild preeclampsia
The earlier preeclampsia develops, the greater the risk it will become severe. The need for hospitalization depends on gestational age, blood pressure, proteinuria levels, maternal symptoms, and reliability of the patient.
Preeclampsia is mild when systolic blood pressure reaches 140 to 159 mm Hg or diastolic pressure measures 90 to 109 mm Hg on at least 2 occasions more than 6 hours apart after 20 weeks’ gestation in a woman who previously had normal blood pressure. In preeclampsia, this hypertension is accompanied by proteinuria of 0.3 to 4.9 g in a 24-hour urine sample (1+ or 2+ by dipstick on 2 occasions).
At or beyond 37 weeks’ gestation
In general, women diagnosed with preeclampsia at this gestational age have pregnancy outcomes similar to those of normotensive gravidas. Thus, they benefit from induction of labor and delivery.
32 to 36 weeks’ gestation
Close maternal and fetal evaluation is essential. (It is assumed these women have no labor or membrane rupture and normal fetal testing; otherwise, delivery is indicated at 34 weeks or beyond.)
In general, hospitalization is indicated when any of the following circumstances are present (FIGURE 1):
- the patient is unreliable,
- 2 or more systolic blood pressure readings exceed 150 mm Hg,
- 2 or more diastolic blood pressure readings exceed 100 mm Hg,
- proteinuria occurs at a rate exceeding 1 g/24 hours, or
- persistent maternal symptoms are present.
FIGURE 1 Treatment of mild preeclampsia in healthy women
Before 32 weeks’ gestation
These women are at high risk of progressing to severe disease. They also are more likely to have adverse perinatal outcomes such as intrauterine growth restriction (IUGR) (15% to 20%), preterm delivery (50%), and abruptio placentae (1% to 2%), compared with women diagnosed with preeclampsia at 32 to 36 weeks. In addition, they require more antenatal surveillance than women who develop preeclampsia later in pregnancy.
I recommend hospitalization at the time of diagnosis when women develop mild preeclampsia before 32 weeks.
What and when to monitor
Maternal evaluation should include:
- monitoring of blood pressure at least daily (at home or in the hospital),
- daily urine dipstick evaluation to monitor changes in proteinuria,
- twice-weekly platelet count and liver enzymes, and
- documentation of symptoms. (Instruct all women to report the onset of severe headaches, visual changes, altered mental status, epigastric or right upper quadrant pain, and any nausea or vomiting.)
Fetal evaluation should include:
- serial ultrasound every 3 weeks to estimate fetal weight and amniotic fluid status,
- nonstress testing every week, and
- daily fetal movement counts.
If a nonstress test is nonreactive, it should be confirmed by biophysical profile.
All testing should be promptly repeated if the maternal clinical condition deteriorates.
No need for bed rest, diuretics, or antihypertensive medications
Although expectantly managed patients with mild preeclampsia should be advised to restrict daily activity, there is no need for complete bed rest. Nor have diuretics or other antihypertensive drugs been shown to prolong gestation. On the contrary, these medications may mask severe preeclampsia.
Antihypertensive medications reduce the rate of severe hypertension but do not improve perinatal outcome. If these drugs are used to treat mild disease remote from term, hospitalize the patient and manage her as though she has severe preeclampsia.
Hospitalization versus outpatient management
Although she may be hospitalized at the time of diagnosis, a woman with preeclampsia may switch to outpatient management if systolic or diastolic blood pressure declines, proteinuria diminishes to 1 g/24 hours or less, and there are no maternal symptoms or evidence of severe IUGR. Otherwise, these women should remain hospitalized until delivery.
In cases that begin with outpatient management, prompt hospitalization is indicated if there is clinical evidence that the disease is progressing (ie, new symptoms, labor or rupture of membranes, vaginal bleeding, or increased blood pressures or proteinuria) or IUGR and/or oligohydramnios.
Instruct all women to report symptoms and changes in fetal movement.
When to deliver
Whether the gravida is hospitalized or an outpatient, delivery is indicated at 37 weeks. Earlier delivery may be warranted if nonreassuring maternal or fetal conditions develop. (FIGURE 1 summarizes management of mild preeclampsia.)
Severe preeclampsia
Expectant management is safe in properly selected women with severe disease, although maternal and fetal conditions can deteriorate. Hospitalization and daily monitoring are required.
Preeclampsia is severe when any of the following are present:
- systolic blood pressure of 160 mm Hg or higher or diastolic pressure of 110 mm Hg or above on 2 occasions at least 6 hours apart while the patient is on bed rest
- proteinuria of 5 g or more in a 24-hour urine specimen,
- oliguria of less than 500 mL in 24 hours,
- cerebral or visual disturbances,
- pulmonary edema or cyanosis,
- severe epigastric or right upper-quadrant pain, or
- thrombocytopenia.
When gestational hypertension or preeclampsia is severe, hospitalization in the labor and delivery suite is warranted. These women should receive intravenous (IV) magnesium sulfate to reduce the risk of convulsions and antihypertensive drugs to treat severe levels of hypertension, if present. The aim of antihypertensive treatment is to keep diastolic blood pressure between 90 and 105 mm Hg and systolic blood pressure below 160 mm Hg.
During observation, assess maternal and fetal conditions and decide whether delivery is indicated (FIGURE 2).
Expectant management is warranted only for gestations between 23 and 32 weeks’ gestation, provided maternal and fetal conditions are stable (FIGURE 2).
Keep in mind that both maternal and fetal conditions may progressively deteriorate. Thus, these pregnancies involve higher rates of maternal morbidity and significant risk of neonatal morbidity. For this reason, expectant management should proceed only in a tertiary-care center with adequate maternal and neonatal facilities.
Recommended counseling
Advise these patients of the potential risks and benefits of expectant management, which requires daily monitoring of maternal and fetal conditions. Also explain that the decision to continue expectant management will be revisited on a daily basis and that the median number of days pregnancy is prolonged in these cases is 7 (range 2 to 35).
Another important fact to relay: Only 2 randomized trials involving 133 women have compared expectant management to aggressive management in early-onset preeclampsia. However, retrospective and observational studies involving more than 700 women suggest expectant management reduces short-term neonatal morbidity with minimal risk to the mother.
Superimposed preeclampsia
Women who develop preeclampsia on top of chronic hypertension, renal disease, or type 1 diabetes have a markedly higher risk of morbidity, including perinatal morbidity, than women without preexisting conditions.
Women with superimposed preeclampsia may be managed in the hospital, since these pregnancies are associated with higher rates of abruptio placentae (2% to 5%), preterm delivery (56%), IUGR (13% to 15%), and perinatal death (8%). Thus, these women benefit from very close maternal and fetal monitoring.
Superimposed preeclampsia is not classified according to severity.
In general, maternal and perinatal morbidities are substantially higher in women who have preexisting conditions than in healthy women who develop preeclampsia.
Chronic hypertension
Indications for delivery are similar to those described for healthy women with preeclampsia, as is antihypertensive therapy.
If the woman develops preeclampsia while using antihypertensive drugs, delivery should be considered beyond 34 weeks’ gestation.
How preeclampsia affects renal function
Women with renal disease or dysfunction (serum creatinine ≥1.2 mg/dL) prior to or early in pregnancy face an increased risk of adverse neonatal outcomes, regardless of whether preeclampsia also develops. These women also face an increased risk of deteriorating renal function during pregnancy (particularly if preeclampsia or severe hypertension develops) and beyond (more than 6 months postpartum).
Start antihypertensive medications as soon as possible, with the goal of keeping systolic blood pressure below 140 mm Hg and diastolic blood pressure below 90 mm Hg throughout gestation.
Delivery is indicated with the onset of preeclampsia or significant deterioration in renal function.
Diabetes warrants aggressive therapy
Women with type 1 diabetes have a higher risk of preeclampsia, maternal and fetal morbidity, and perinatal mortality. These risks multiply in women who have hypertension and/or diabetic nephropathy. Worsening of retinopathy and nephropathy also is more likely in women who have hypertension. Thus, aggressive management of blood sugars with insulin should be accompanied by aggressive control of blood pressure, with the goal of keeping systolic pressure below 130 mm Hg and diastolic pressure below 85 mm Hg.
Choosing antihypertensive drugs. Calcium-channel blockers are preferred to control blood pressure during pregnancy in women with diabetes. Outside of pregnancy, angiotensin-converting enzyme (ACE) inhibitors are best to avert long-term complications, but avoid these drugs in pregnancy (along with angiotensin-receptor blockers), particularly beyond 16 weeks.
Delivery is indicated in all women with vascular diabetes mellitus beyond 34 weeks when preeclampsia is present.
Intrapartum management
Close fetal heart rate and maternal blood pressure monitoring are mainstays, along with magnesium sulfate and antihypertensive therapy.
All women with preeclampsia should receive continuous monitoring of fetal heart rate and uterine activity, with special vigilance for hyperstimulation and onset of vaginal bleeding during labor. (For a description of potential maternal complications, see TABLE 1; fetal complications are described in FIGURE 3.)
Uterine irritability, recurrent variable or late decelerations, and the development of vaginal bleeding may be the first signs of abruptio placentae.
I recommend recording maternal blood pressure at least hourly to detect progression from mild to severe hypertension and to determine the need for antihypertensive therapy.
TABLE 1
Likelihood of maternal complications
| Disease progresses during labor (from mild to severe) | 10% |
| Eclampsia | |
| • Mild disease | <0.5% |
| • Severe preeclampsia | 1–2% |
| Stroke (encephalopathy or hemorrhage) | <1% |
| Mainly with severe or early onset disease | |
| Pulmonary edema | 1–2% |
| Usually associated with fluid overload or long-standing chronic hypertension | |
Prevent progression to eclampsia
Magnesium sulfate is the drug of choice in women with preeclampsia. Recent reviews indicate that it reduces the rate of convulsions from 2% to 0.6% in women with severe preeclampsia. In women with mild preeclampsia, the benefit of magnesium sulfate remains unclear.
I recommend IV magnesium sulfate during labor and postpartum when a woman has the indications listed in TABLE 2.
The dose of magnesium sulfate is 6 g IV loading over 20 minutes, followed by a maintenance dose of 2 g/hour.
Magnesium sulfate should be started before surgery (elective cesarean delivery) and continued for at least 12 hours postpartum (I prefer 24 hours).
TABLE 2
When to give prophylactic magnesium sulfate
| Use intrapartum and for at least 12 hours postpartum |
|---|
When the patient has:
|
When treating hypertension in labor, avoid “hypotensive overshoot”
The goal of intrapartum treatment is to lower maternal blood pressure without causing precipitous hypotensive overshoot that may lead to reduced maternal organ perfusion, particularly uteroplacental blood flow. Such acute lowering of maternal blood pressure is a common cause of nonreassuring fetal heart rate patterns during labor.
What blood pressure necessitates treatment? There is no doubt that severe levels of hypertension should be treated to avoid potential cerebrovascular and cardiovascular complications in healthy women. However, there is disagreement about what constitutes severe hypertension.
In previously healthy women, I recommend antihypertensive therapy for systolic pressures of 170 mm Hg or above and/or for diastolic pressures of 110 mm Hg or above.
For women with thrombocytopenia, disseminated intravascular coagulation, or pulmonary edema, I recommend treatment for systolic pressures of 160 mm Hg or above and diastolic pressures of 105 mm Hg or above. This latter group should also be given IV furosemide (20 to 40 mg) to promote diuresis. I also recommend treatment at these levels in the postpartum period.
For women with diabetes, renal disease, or left ventricular cardiac disease, antihypertensive medications should be used to keep systolic pressure below 140 mm Hg and diastolic pressure below 90 mm Hg during labor and postpartum. Further, patients in congestive heart failure or with left ventricular diastolic dysfunction should receive furosemide in addition to antihypertensive drugs.
Choosing a drug. My drugs of choice are IV labetalol and oral nifedipine. These 2 drugs, along with IV hydralazine, are the most commonly recommended medications for severe hypertension in pregnancy (TABLE 3).
Although many authorities prefer hydralazine, recent data indicate that, compared with IV labetalol and oral nifedipine, IV hydralazine is associated with more maternal side effects and worse perinatal outcomes (more fetal distress in labor).
TABLE 3
Drug profiles: Dosing and side effects of antihypertensives used in pregnancy
| MEDICATION | ONSET OF ACTION | DOSE | SIDE EFFECTS |
|---|---|---|---|
| Hydralazine | 10-20 minutes | 5-10 mg intravenously every 20 minutes up to maximum dose of 30 mg | More maternal side effects and worse perinatal outcomes than labetalol or nifedipine. |
| Skin blisters; chest pain; general feeling of discomfort, illness, or weakness; joint or muscle pain; sore throat and fever; swollen lymph glands | |||
| Labetalol* | 10-15 minutes | 10-20 mg intravenously, then 40-80 mg every 10 minutes up to maximum dose of 220 mg/hour or continuous infusion of 1-2 mg/minute | Breathing difficulty and/or wheezing, cold hands and feet, mental depression, shortness of breath, slow heartbeat, swelling of lower extremities, back or joint pain, chest pain, confusion, fever and sore throat, hallucinations, irregular heartbeat, unusual bleeding and bruising, yellow eyes or skin |
| Nifedipine | 5-10 minutes | 10-20 mg orally, repeated in 30 minutes, up to maximum dose of 50 mg/hour | Breathing difficulty, coughing, or wheezing; irregular or fast, poundingheartbeat; skin rash; swelling of lower extremities; chest pain; fainting; painful, swollen joints; vision impairment |
| Sodium nitroprusside† | 0.5-5 minutes | 0.25-5 μg/kg/minute by intravenous infusion | Risk of fetal cyanide poisoning with prolonged treatment. |
| Maternal effects include symptoms of hypothyroidism, headache, abdominal pain, drowsiness, nausea, involuntary muscle movements, perspiration, restlessness, paraesthesia, palpitations, dizziness, retching, tachycardia | |||
| *In women with asthma and congestive heart failure | |||
| †Rarely needed except in hypertensive encephalopathy or cerebral hemorrhage | |||
Postpartum management
Because preeclampsia can worsen, or first appear, in the postpartum period, extra vigilance is important, and pharmacotherapy may be appropriate.
Management of preeclampsia does not end with delivery of the fetus and the placenta. These events do signal the beginning of the curative process, but complications can occur in the postpartum period. Indeed, in some women, the disease process worsens immediately postpartum. Therefore, women with diagnosed preeclampsia or severe gestational hypertension require close monitoring of blood pressure and maternal symptoms and accurate measurement of fluid intake and urine output. Some of these women are at increased risk for pulmonary edema; exacerbation of severe hypertension; eclampsia; and hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome.
Treating postpartum hypertension
Women who continue to have severe hypertension (systolic pressure at or above 155 mm Hg or diastolic pressure of 105 mm Hg or higher) will benefit from oral nifedipine (10 mg every 6 hours) or long-acting nifedipine (10 to 20 mg twice daily), the drugs of choice because of their favorable effects on renal function.
Women with severe hypertension also may require diuretics for better control of blood pressure, as may women with a history of congestive heart failure or left ventricular dysfunction.
Start women with vascular diabetes mellitus or diabetic nephropathy on ACE inhibitors immediately postpartum.
Patients can be discharged home once blood pressure is stable, provided there are no maternal symptoms of preeclampsia.
Postpartum preeclampsia can develop even in healthy women
Because severe hypertension or preeclampsia may develop for the first time in the postpartum period, it is important to educate all gravidas about the signs and symptoms. All health-care providers should be on the lookout for these symptoms as well.
The author reports no financial relationships relevant to this article.
BIBLIOGRAPHY
Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev (England). 2001;(2)pCD002252.-
Alfirevic Z, Roberts D, Martlew V. How strong is the association between maternal thrombophilia and adverse pregnancy outcome? A systematic review. Eur J Obstet Gynecol Reprod Biol. 2002;101:6-14.
Amorim MMR, Santas LC, Faundes A. Corticosteroid therapy for prevention of respiratory distress syndrome in severe preeclampsia. Am J Obstet Gynecol. 1999;180:1283-1288.
Duley L, Galmezoglu AM, Henderson-Smart DJ. Magnesium sulfate and other anticonvulsants for women with preeclampsia. Cochrane Database Syst Rev (England). 2003;(2)pCD000025.-
Friedman SA, Lubarsky S, Schiff E. Expectant management of severe preeclampsia remote from term. Clin Obstet Gynecol. 1999;42:470-478.
Haddad B, Deis S, Goffinet F, et al. Maternal and perinatal outcomes during expectant management of 239 severe preeclamptic women between 24 and 33 weeks’ gestation. Am J Obstet Gynecol. 2004;190:1590-1597.
Hall DR, Odendaal HJ, Kirten GF, Smith J. Expectant management of early onset, severe preeclampsia, perinatal outcome. BJOG. 2000;107:1258-1264.
Kupferminc MJ, Fait G, Many A, et al. Low molecular weight heparin for the prevention of obstetric complications in women with thrombophilia. Hypertension in Pregnancy. 2001;20:35-44.
Kupferminc MJ. Thrombophilia and pregnancy. Reprod Biol Endocrinol. 2003;1:111-166.
Magee LA, Cham C, Waterman EJ, Ohlsson A, Von Dadelszen P. Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003;327:1-10.
Magee LA, Ornstein MP, Von Dadelszen P. Fortnightly review: management of hypertension in pregnancy. BMJ. 1999;318:1332-1336.
Magpie Trial Group. Do women with preeclampsia, and their babies, benefit from magnesium sulfate? The Magpie Trial: a randomised, placebo-controlled trial. Lancet. 2002;359:1877-1890.
Report of the National High Blood Pressure Education Program. Working group report on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000;183:S1-22.
Sibai BM. Chronic hypertension in pregnancy. Obstet Gynecol. 2002;100:369-377.
Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003;102:181-192.
Sibai BM, Lindheimer MD, Hauth J, et al. Risk factors for preeclampsia, abruptio placentae, and adverse neonatal outcomes among women with chronic hypertension. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;229:667-671.
Sibai BM. Magnesium sulfate prophylaxis in preeclampsia. Lessons learned from recent trials. Am J Obstet Gynecol. 2004;190:1520-1526.
Vigil-DeGracia P, Montufar-Rueda C, Ruiz J. Expectant management of severe preeclampsia and preeclampsia superimposed on chronic hypertension between 24 and 34 weeks’ gestation. Eur J Obstet Gynecol Reprod Biol. 2003;107:24-27.
BIBLIOGRAPHY
Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev (England). 2001;(2)pCD002252.-
Alfirevic Z, Roberts D, Martlew V. How strong is the association between maternal thrombophilia and adverse pregnancy outcome? A systematic review. Eur J Obstet Gynecol Reprod Biol. 2002;101:6-14.
Amorim MMR, Santas LC, Faundes A. Corticosteroid therapy for prevention of respiratory distress syndrome in severe preeclampsia. Am J Obstet Gynecol. 1999;180:1283-1288.
Duley L, Galmezoglu AM, Henderson-Smart DJ. Magnesium sulfate and other anticonvulsants for women with preeclampsia. Cochrane Database Syst Rev (England). 2003;(2)pCD000025.-
Friedman SA, Lubarsky S, Schiff E. Expectant management of severe preeclampsia remote from term. Clin Obstet Gynecol. 1999;42:470-478.
Haddad B, Deis S, Goffinet F, et al. Maternal and perinatal outcomes during expectant management of 239 severe preeclamptic women between 24 and 33 weeks’ gestation. Am J Obstet Gynecol. 2004;190:1590-1597.
Hall DR, Odendaal HJ, Kirten GF, Smith J. Expectant management of early onset, severe preeclampsia, perinatal outcome. BJOG. 2000;107:1258-1264.
Kupferminc MJ, Fait G, Many A, et al. Low molecular weight heparin for the prevention of obstetric complications in women with thrombophilia. Hypertension in Pregnancy. 2001;20:35-44.
Kupferminc MJ. Thrombophilia and pregnancy. Reprod Biol Endocrinol. 2003;1:111-166.
Magee LA, Cham C, Waterman EJ, Ohlsson A, Von Dadelszen P. Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003;327:1-10.
Magee LA, Ornstein MP, Von Dadelszen P. Fortnightly review: management of hypertension in pregnancy. BMJ. 1999;318:1332-1336.
Magpie Trial Group. Do women with preeclampsia, and their babies, benefit from magnesium sulfate? The Magpie Trial: a randomised, placebo-controlled trial. Lancet. 2002;359:1877-1890.
Report of the National High Blood Pressure Education Program. Working group report on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000;183:S1-22.
Sibai BM. Chronic hypertension in pregnancy. Obstet Gynecol. 2002;100:369-377.
Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003;102:181-192.
Sibai BM, Lindheimer MD, Hauth J, et al. Risk factors for preeclampsia, abruptio placentae, and adverse neonatal outcomes among women with chronic hypertension. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;229:667-671.
Sibai BM. Magnesium sulfate prophylaxis in preeclampsia. Lessons learned from recent trials. Am J Obstet Gynecol. 2004;190:1520-1526.
Vigil-DeGracia P, Montufar-Rueda C, Ruiz J. Expectant management of severe preeclampsia and preeclampsia superimposed on chronic hypertension between 24 and 34 weeks’ gestation. Eur J Obstet Gynecol Reprod Biol. 2003;107:24-27.