User login
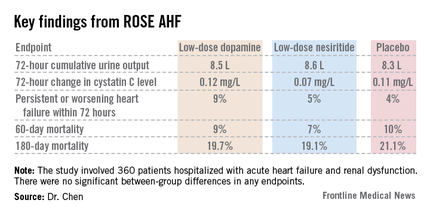
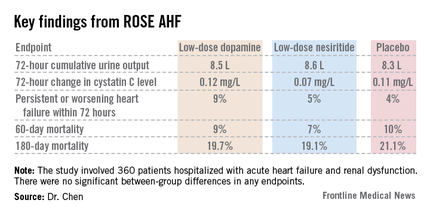
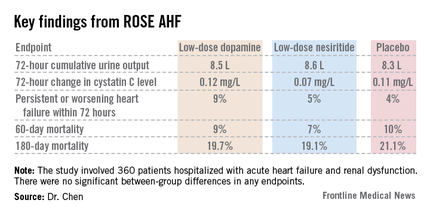
DALLAS – Neither low-dose dopamine nor low-dose nesiritide enhanced decongestion or improved renal function in patients with acute heart failure and kidney dysfunction in the randomized ROSE AHF trial.
Thus, the major unmet need for drugs that accomplish these benefits continues. There remains no Food and Drug Administration–approved therapy for enhancing renal function in acute heart failure, Dr. Horng H. Chen observed in presenting the ROSE AHF results at the American Heart Association scientific sessions.
The need for such therapies is great. Most patients with heart failure eventually develop renal dysfunction. If this dysfunction is moderate or severe, patients may experience inadequate decongestion in response to diuretic therapy along with worsening renal dysfunction, both linked to poor clinical outcomes.
Prior small, single-center studies with various methodologic shortcomings had suggested possible benefit for dopamine or nesiritide in low doses thought to be renal specific. The ROSE AHF (Renal Optimization Strategies Evaluation in Acute Heart Failure) trial was conducted to provide definitive evidence to guide practice, explained Dr. Chen, professor of medicine at the Mayo Clinic, Rochester, Minn.
ROSE AHF was a randomized, double-blind, placebo-controlled clinical trial involving 360 patients hospitalized with AHF and renal dysfunction at 26 U.S. and Canadian centers. The study was carried out by the National Heart, Lung, and Blood Institute (NHLBI) Heart Failure Clinical Research Network. Patients were randomized within 24 hours of admission to low-dose dopamine at 2 mcg/kg per minute, low-dose nesiritide at 0.005 mcg/kg per minute, or placebo.
The coprimary endpoints were 72-hour cumulative urine volume as a measure of decongestion and 72-hour change in serum cystatin C as an indicator of renal function.
Interestingly, the two drugs clearly were not truly renal specific, even in these low doses widely considered to be so, Dr. Chen noted. This lack of renal specificity was evident from the side effect profile. Significant tachycardia occurred in 7.2% of the low-dose dopamine group, none on nesiritide, and 10.4% of placebo-treated controls. In contrast, significant hypotension occurred in 0.9% of patients on dopamine, 18.8% on nesiritide, and 10.4% on placebo.
A trend toward a differential treatment response depending upon whether a patient had heart failure with a reduced versus preserved ejection fraction was evident. Patients with diastolic heart failure tended to do worse with dopamine than placebo in terms of 72-hour urine output, while those with systolic heart failure tended to do better with nesiritide than placebo. However, the trial was insufficiently powered to draw definitive conclusions on this score.
"One of our take-away messages when we looked at the data was that acute heart failure is broadly defined and includes a very diverse group of patients. With the suggestion that there may be a differential response based on ejection fraction, as we proceed with future heart failure studies we may consider targeting subsets of patients. Some therapies may benefit patients with reduced ejection fraction, others will benefit patients with preserved ejection fraction. We might want to power our studies to look at these subgroups," according to Dr. Chen.
Noting that current American Heart Association/American College of Cardiology guidelines for AHF management state that low-dose dopamine "may be considered" to improve diuresis and preserve renal function during diuretic therapy, the cardiologist said "the only conclusion we can make from our study is they should not be used routinely."
He added a caveat, however: "In my own practice, if I have a patient who is hypotensive and who hasn’t responded to increased doses of diuretics, I still may consider using low-dose dopamine at that stage" because of the reassuringly low 0.9% rate of hypotension in ROSE AHF.
Discussant Dr. Marco Metra of the University of Brescia (Italy) noted that low doses of dopamine and nesiritide are widely used in the United States and Europe. Recent data suggest nesiritide is used in 5%-10% of American patients with AHF and low-dose dopamine in 3%-5%.
"Surely this trial should reduce the use of these drugs in patients with acute heart failure. They are given routinely too often in some places," he said.
Discussant Marc Pfeffer called ROSE AHF "yet another example of shedding the light of the randomized controlled trial on things that we assume to be true but actually aren’t. And we probably spend more time on rounds talking about [improving decongestion in patients with AHF and renal dysfunction] than anything else," added Dr. Pfeffer, professor of medicine at Harvard University, Boston.
The ROSE AHF trial was sponsored by the NHLBI. Dr. Chen reported receiving research grants from Scios and royalties from Niles Therapeutics, Anexon, and UpToDate. Dr. Metra is a paid consultant to a handful of pharmaceutical companies.
DALLAS – Neither low-dose dopamine nor low-dose nesiritide enhanced decongestion or improved renal function in patients with acute heart failure and kidney dysfunction in the randomized ROSE AHF trial.
Thus, the major unmet need for drugs that accomplish these benefits continues. There remains no Food and Drug Administration–approved therapy for enhancing renal function in acute heart failure, Dr. Horng H. Chen observed in presenting the ROSE AHF results at the American Heart Association scientific sessions.
The need for such therapies is great. Most patients with heart failure eventually develop renal dysfunction. If this dysfunction is moderate or severe, patients may experience inadequate decongestion in response to diuretic therapy along with worsening renal dysfunction, both linked to poor clinical outcomes.
Prior small, single-center studies with various methodologic shortcomings had suggested possible benefit for dopamine or nesiritide in low doses thought to be renal specific. The ROSE AHF (Renal Optimization Strategies Evaluation in Acute Heart Failure) trial was conducted to provide definitive evidence to guide practice, explained Dr. Chen, professor of medicine at the Mayo Clinic, Rochester, Minn.
ROSE AHF was a randomized, double-blind, placebo-controlled clinical trial involving 360 patients hospitalized with AHF and renal dysfunction at 26 U.S. and Canadian centers. The study was carried out by the National Heart, Lung, and Blood Institute (NHLBI) Heart Failure Clinical Research Network. Patients were randomized within 24 hours of admission to low-dose dopamine at 2 mcg/kg per minute, low-dose nesiritide at 0.005 mcg/kg per minute, or placebo.
The coprimary endpoints were 72-hour cumulative urine volume as a measure of decongestion and 72-hour change in serum cystatin C as an indicator of renal function.
Interestingly, the two drugs clearly were not truly renal specific, even in these low doses widely considered to be so, Dr. Chen noted. This lack of renal specificity was evident from the side effect profile. Significant tachycardia occurred in 7.2% of the low-dose dopamine group, none on nesiritide, and 10.4% of placebo-treated controls. In contrast, significant hypotension occurred in 0.9% of patients on dopamine, 18.8% on nesiritide, and 10.4% on placebo.
A trend toward a differential treatment response depending upon whether a patient had heart failure with a reduced versus preserved ejection fraction was evident. Patients with diastolic heart failure tended to do worse with dopamine than placebo in terms of 72-hour urine output, while those with systolic heart failure tended to do better with nesiritide than placebo. However, the trial was insufficiently powered to draw definitive conclusions on this score.
"One of our take-away messages when we looked at the data was that acute heart failure is broadly defined and includes a very diverse group of patients. With the suggestion that there may be a differential response based on ejection fraction, as we proceed with future heart failure studies we may consider targeting subsets of patients. Some therapies may benefit patients with reduced ejection fraction, others will benefit patients with preserved ejection fraction. We might want to power our studies to look at these subgroups," according to Dr. Chen.
Noting that current American Heart Association/American College of Cardiology guidelines for AHF management state that low-dose dopamine "may be considered" to improve diuresis and preserve renal function during diuretic therapy, the cardiologist said "the only conclusion we can make from our study is they should not be used routinely."
He added a caveat, however: "In my own practice, if I have a patient who is hypotensive and who hasn’t responded to increased doses of diuretics, I still may consider using low-dose dopamine at that stage" because of the reassuringly low 0.9% rate of hypotension in ROSE AHF.
Discussant Dr. Marco Metra of the University of Brescia (Italy) noted that low doses of dopamine and nesiritide are widely used in the United States and Europe. Recent data suggest nesiritide is used in 5%-10% of American patients with AHF and low-dose dopamine in 3%-5%.
"Surely this trial should reduce the use of these drugs in patients with acute heart failure. They are given routinely too often in some places," he said.
Discussant Marc Pfeffer called ROSE AHF "yet another example of shedding the light of the randomized controlled trial on things that we assume to be true but actually aren’t. And we probably spend more time on rounds talking about [improving decongestion in patients with AHF and renal dysfunction] than anything else," added Dr. Pfeffer, professor of medicine at Harvard University, Boston.
The ROSE AHF trial was sponsored by the NHLBI. Dr. Chen reported receiving research grants from Scios and royalties from Niles Therapeutics, Anexon, and UpToDate. Dr. Metra is a paid consultant to a handful of pharmaceutical companies.
DALLAS – Neither low-dose dopamine nor low-dose nesiritide enhanced decongestion or improved renal function in patients with acute heart failure and kidney dysfunction in the randomized ROSE AHF trial.
Thus, the major unmet need for drugs that accomplish these benefits continues. There remains no Food and Drug Administration–approved therapy for enhancing renal function in acute heart failure, Dr. Horng H. Chen observed in presenting the ROSE AHF results at the American Heart Association scientific sessions.
The need for such therapies is great. Most patients with heart failure eventually develop renal dysfunction. If this dysfunction is moderate or severe, patients may experience inadequate decongestion in response to diuretic therapy along with worsening renal dysfunction, both linked to poor clinical outcomes.
Prior small, single-center studies with various methodologic shortcomings had suggested possible benefit for dopamine or nesiritide in low doses thought to be renal specific. The ROSE AHF (Renal Optimization Strategies Evaluation in Acute Heart Failure) trial was conducted to provide definitive evidence to guide practice, explained Dr. Chen, professor of medicine at the Mayo Clinic, Rochester, Minn.
ROSE AHF was a randomized, double-blind, placebo-controlled clinical trial involving 360 patients hospitalized with AHF and renal dysfunction at 26 U.S. and Canadian centers. The study was carried out by the National Heart, Lung, and Blood Institute (NHLBI) Heart Failure Clinical Research Network. Patients were randomized within 24 hours of admission to low-dose dopamine at 2 mcg/kg per minute, low-dose nesiritide at 0.005 mcg/kg per minute, or placebo.
The coprimary endpoints were 72-hour cumulative urine volume as a measure of decongestion and 72-hour change in serum cystatin C as an indicator of renal function.
Interestingly, the two drugs clearly were not truly renal specific, even in these low doses widely considered to be so, Dr. Chen noted. This lack of renal specificity was evident from the side effect profile. Significant tachycardia occurred in 7.2% of the low-dose dopamine group, none on nesiritide, and 10.4% of placebo-treated controls. In contrast, significant hypotension occurred in 0.9% of patients on dopamine, 18.8% on nesiritide, and 10.4% on placebo.
A trend toward a differential treatment response depending upon whether a patient had heart failure with a reduced versus preserved ejection fraction was evident. Patients with diastolic heart failure tended to do worse with dopamine than placebo in terms of 72-hour urine output, while those with systolic heart failure tended to do better with nesiritide than placebo. However, the trial was insufficiently powered to draw definitive conclusions on this score.
"One of our take-away messages when we looked at the data was that acute heart failure is broadly defined and includes a very diverse group of patients. With the suggestion that there may be a differential response based on ejection fraction, as we proceed with future heart failure studies we may consider targeting subsets of patients. Some therapies may benefit patients with reduced ejection fraction, others will benefit patients with preserved ejection fraction. We might want to power our studies to look at these subgroups," according to Dr. Chen.
Noting that current American Heart Association/American College of Cardiology guidelines for AHF management state that low-dose dopamine "may be considered" to improve diuresis and preserve renal function during diuretic therapy, the cardiologist said "the only conclusion we can make from our study is they should not be used routinely."
He added a caveat, however: "In my own practice, if I have a patient who is hypotensive and who hasn’t responded to increased doses of diuretics, I still may consider using low-dose dopamine at that stage" because of the reassuringly low 0.9% rate of hypotension in ROSE AHF.
Discussant Dr. Marco Metra of the University of Brescia (Italy) noted that low doses of dopamine and nesiritide are widely used in the United States and Europe. Recent data suggest nesiritide is used in 5%-10% of American patients with AHF and low-dose dopamine in 3%-5%.
"Surely this trial should reduce the use of these drugs in patients with acute heart failure. They are given routinely too often in some places," he said.
Discussant Marc Pfeffer called ROSE AHF "yet another example of shedding the light of the randomized controlled trial on things that we assume to be true but actually aren’t. And we probably spend more time on rounds talking about [improving decongestion in patients with AHF and renal dysfunction] than anything else," added Dr. Pfeffer, professor of medicine at Harvard University, Boston.
The ROSE AHF trial was sponsored by the NHLBI. Dr. Chen reported receiving research grants from Scios and royalties from Niles Therapeutics, Anexon, and UpToDate. Dr. Metra is a paid consultant to a handful of pharmaceutical companies.
AT THE AHA SCIENTIFIC SESSIONS
Major finding: Neither low-dose dopamine nor low-dose nesiritide improved decongestion or boosted renal function when added to diuretic therapy in patients hospitalized with acute heart failure and kidney dysfunction.
Data source: ROSE AHF, a multicenter, randomized, double-blind, placebo-controlled clinical trial of 360 patients with acute heart failure and renal dysfunction.
Disclosures. The trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Chen reported receiving research grants from Scios and royalties from Niles Therapeutics, Anexon, and UpToDate. Dr. Metra is a paid consultant to a handful of pharmaceutical companies.


