User login
CE/CME No: CR-1409
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Define the term concussion.
• Identify the major signs and symptoms of a concussion.
• Discuss the initial management of a pediatric patient with a suspected sports-related concussion.
• Describe the current recommendations for return to play after a pediatric concussion.
• Explain the main challenges clinicians face in the management of pediatric concussions
FACULTY
Sydney Meckler is pursuing her Doctor of Nursing Practice degree at Columbia University, New York City. The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
This article describes the challenges of diagnosis and treatment of pediatric concussive injuries, with particular attention to the effects of concussion on the developing brain. It highlights the need for individualized, age-dependent care; standardized return-to-play and return-to-school protocols; and better-informed clinicians, parents, teachers, and coaches.
Pediatric concussions—those occurring in children younger than 18—account for almost half a million emergency department visits each year.1 Of these, more than 25% occur during sports-related activities.2 Yet it is believed that pediatric concussive injuries are significantly underreported because parents do not always seek medical attention for their concussed children and because little has been published on the management of sports-related concussions in pre–high-school-age athletes.2
The 4th International Consensus Conference on Concussion in Sport, the American Academy of Neurology, and the American Medical Society for Sports Medicine all recently updated their guidelines for concussion evaluation and management.3-5 However, the lack of data on concussions in younger pediatric athletes presents challenges for the optimal management of these patients.6 In fact, in a February 2014 report, the Institute of Medicine said that more research is needed to develop evidence-based sports-related concussion management guidelines for children and adolescents.7
In this article, the factors that distinguish concussions in children from those in adults will be described, as will the management techniques that primary care clinicians can use to effectively address them.
WHAT IS A CONCUSSION?
Although the term concussion has been used interchangeably with head trauma and brain injury, concussion is most often described as mild traumatic brain injury (mTBI). Variations in terminology reflect both the lack of agreement on a standard definition for concussion, especially as it applies to the pediatric population, and the complexities of concussion diagnosis and management.8 This inherent ambiguity can lead to suboptimal recognition and awareness of concussion among clinicians, patients, families, school personnel, and sports staff, especially of its serious aftereffects in the pediatric patient.
A blow to the head can propel the brain to strike one side of the skull and then bounce off the opposite side. This can damage or tear the axons—the signal transmitters of the neurons—from their cell bodies, disrupting brain cell communications and causing neurocognitive deficits.
While a concussion is a direct injury to the brain, it is also an evolving process comprised of several pathophysiologic components that are a consequence of biomechanical forces. The brain does not directly contact the skull but is surrounded by cerebrospinal fluid and fluid-filled vessels with a greater density than the brain itself. This intracranial space provides room for the brain to move upon impact by shifting and compressing from one side of the skull to the other.9 The concussive injury occurs as a result of either a direct strike to the head or from an indirect force traumatic enough to be transmitted to the brain. The strike or force produces a complex disturbance to the brain that, in most cases, does not result in loss of consciousness.3
THE GREATER VULNERABILITY OF THE PEDIATRIC BRAIN
Pathophysiology
For a concussion to occur, the biomechanical threshold at which nerve cells' adaptability is impeded must be crossed.10 This sets in motion a cascade of events, developing over minutes, hours, and even days, in which homeostasis is disrupted due to an imbalance of ionic, neuronal, metabolic, and pathophysiologic processes.5
While many studies have sought to explain the pathophysiology of pediatric sports-related concussions, much is still unknown. One hypothesis suggests that, after the injury, neuronal depolarization occurs, releasing excitatory neurotransmitters and altering metabolism by the immediate release of potassium. Restoration of homeostasis demands response by the sodium-potassium pump, requiring energy in the form of glucose. Coupled with axonal injury and alterations in cerebral blood flow, an imbalance between energy supply and demand occurs.5
Maugans et al found that a single pediatric concussion does not cause a structural or metabolic injury but instead a physiologic interruption—different from what occurs in adult concussions.10 They observed a statistically significant reduction in cerebral blood flow of more than 10% in a small group of postconcussion children, ages 11 to 15, compared with a control group. This alteration persisted for two weeks in two-thirds of the children and for up to a month in the remaining third.10 The delayed return of normal cerebral blood flow is believed to be a major contributing factor to pediatric concussion-related symptoms. However, little is known about the long-term effects of concussion on the developing brain.9
Crucial developmental years
Because the pediatric brain is still developing, children between the ages of 5 and 12 are at greater risk for sustaining a disruption in brain function from a concussion. In addition, this group is more susceptible in general to sports injuries compared to adults, because of their stage of growth and development.11
With a pediatric concussion, the individual child’s stage of brain development and the possible effects on his or her evolving neurocognitive functioning must be taken into account. Critical skills, such as language, emotion, memory, problem solving, and motor dexterity, emerge during childhood, and a disturbance during this time could have substantial consequences.12 Motor skills and primary senses usually mature by age 5, with language maturity occurring by age 10.9 However, many other vital skills and processes, such as emotion, judgment, and abstract reasoning, are not fully developed until adulthood. As a result, damage to cortical areas of the brain, such as the parietal lobe and frontal areas—involved in fine motor skills and complex thinking—can hinder or delay the development of these necessary processes.9
Many researchers suggest that, while a concussion to the developing brain may not significantly affect previously learned functions, it may notably delay development of new cognitive functions. As a result, recovery from a concussion during these years may be poorer.2,9,12
On the next page: Clinical presentation and post injury evaluation >>
CLINICAL PRESENTATION
Initial assessment of pediatric athletes with suspected concussive injuries can be particularly challenging because of the variability and evolving nature of associated signs and symptoms, resulting in a wide range of clinical presentations.3 These presenting signs and symptoms can, however, provide vital clues to the location of the injury within the brain because the consequences of concussion arise from injury to the brain’s cortical and subcortical systems (see Table 1).9
The cortical systems are located within the frontal, temporal, parietal, and occipital lobes, each of which houses control centers for specific learned skills and functions. The subcortical systems include the hypothalamus, trigeminal system, basal ganglia, and cerebellum. While a concussion most often causes diffuse harm rather than localized trauma, familiarity with the functions associated with specific brain locations aids in initial identification of the injury and allows for individualized concussion management.13
After a concussion occurs, it is essential to evaluate all domains of the child’s functioning through a comprehensive physical assessment, including a detailed concussion history and review of preinjury risk factors.3 In addition, there may be unobservable symptoms about which a child is unable to communicate due to his or her stage of emotional and cognitive development and restricted capacity to serve as a primary reporter.14
Signs and symptoms
The four categories of concussion signs and symptoms include physical, cognitive, emotional, and sleep (see Table 2).15 A concussed patient may experience any variation or combination of these signs and symptoms.
It is important to recognize that, although loss of consciousness is a serious sign of a concussion, it occurs in only about 10% of concussive injuries.5,15 In fact, current concussion guidelines no longer advocate the use of grading scales, which assessed the severity of a concussion based primarily on the presence or absence of a brief loss of consciousness. Evidence now shows that loss of consciousness does not predict clinical course or cognitive long-term impairment after a concussion.16
Duration of symptoms
The duration of concussion symptoms can vary, but in most cases symptoms last seven to 10 days, with 10% to 15% of patients reporting symptoms for more than 10 days.3,5 While recovery duration has not been studied sufficiently in children younger than 15, younger children require longer recovery periods. The resolution of symptoms, however, does not necessarily correlate with absolute cognitive recovery.5,17
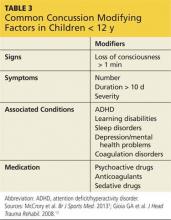
Modifying and complicating factors
In addition to the patient’s presenting signs and symptoms, factors that may modify or complicate recovery from a concussion should be identified (see Table 3).3 These factors include preexisting conditions or disorders and the use of certain prescription drugs. Each factor should be assessed individually, taking into account the patient’s age.2
Some presenting symptoms may overlap with symptoms of common disorders in this group. It is important to note if symptoms of such conditions as attention-deficit/hyperactivity disorder (ADHD), sleep disorders, learning disabilities, and mood disorders were present prior to the concussion.5
Modifying factors provide essential information that can help predict the individual patient’s anticipated recovery process and must be taken into account throughout the process. They are particularly important when assessing the differences between a child’s preconcussion and postconcussion functioning.3,4
POST INJURY EVALUATION OF COGNITIVE FUNCTIONING
Concussion is diagnosed clinically, based on the mechanism of the sustained injury, and is supported primarily by reported and observed signs and symptoms. The ability to systematically evaluate the patient for manifestations of concussion is essential to pediatric concussion management.3,18
To aid in appropriately evaluating symptoms and assessing functional damage, many standardized assessment tools and neuropsychological tests have been developed. These tools have been modified for younger athletes due to differences in children’s neurocognitive development and in their ability to be symptom self-reporters.
Concussion assessment tools
The tools most commonly used to assess the effects of concussion in younger athletes are listed in Table 4. It was not until 2012, with the release of the Child Sport Concussion Assessment Tool Version 3 (Child-SCAT3), that an appropriately adapted and valid concussion assessment tool became available for children younger than 10.3
Assessment tools are useful but are not diagnostic. They do not take the place of a clinician’s thorough neurocognitive evaluation of a potentially concussed child.
Neuropsychologic testing
In order to properly manage pediatric concussions, postconcussion status must be assessed relative to preconcussion status in order to ensure optimal resolution of symptoms and cognitive recovery.19
The American Medical Society for Sports Medicine supports baseline testing for high-risk athletes, defined as those with a prior history of concussions or “confounding” conditions (learning disability, mood and attention disorders, migraine headaches).5 The International Consensus Statement on Concussion in Sport states that there is insufficient evidence to recommend routine baseline testing, but its early use after pediatric concussion may provide helpful information for determining when the child may return to school. The American Academy of Neurology suggests that clinicians “… might utilize baseline scores on concussion assessment tools, especially in younger athletes, those with prior concussions, or those with preexisting learning disabilities/ADHD, as doing so fosters better interpretation of postinjury scores.”4
Assessment tools can provide essential insight into the cognitive functional state of a concussed child athlete, even after symptom resolution.3,5,20 They are not stand-alone measures of recovery but can be useful components of the pediatric concussion evaluation and management process and an aid to clinical decision making.3,13
Paper-and-pencil or computerized neuropsychologic tests provide objective measures of brain-behavior relationships and are more sensitive in detecting subtle cognitive impairments than a clinical examination.5 Although neuropsychologic testing has not been validated as a diagnostic tool, it may be useful for both baseline (preinjury) testing of athletes and for monitoring recovery from a concussive event.5,20 (For more information on motor control assessment, see Dirks RP, McLeod TCV. Sport-related mild traumatic brain injury. Clinician Reviews. 2008;18[9]:22. http://bit.ly/1mjizIa.)
On the next page: Postconcussion management >>
POSTCONCUSSION MANAGEMENT
All concussion management guidelines concur that immediate removal from play of a pediatric athlete with a suspected concussion is the most important initial action. Regardless of how short the duration or mild the symptoms may be, same-day return to play should never occur.3-5 This is particularly true because acute concussion is an evolving injury and manifestation of symptoms, including cognitive deficits, is often delayed.3
The foundation of postconcussion recovery is rest, both physical and cognitive. Acute symptoms must diminish before a gradual resumption of activities.3,5
Cognitive rest
Cognitive rest is the cornerstone of concussion management.5 The latest guidelines stress the importance, particularly in the pediatric age-group, of decreasing any activities of daily living that may aggravate symptoms.3 This includes such common childhood pastimes as playing video games, watching television, and using a computer.15 More important, cognitive rest means academic rest, which is essential to postconcussion recovery and preparing the child for a “return to school” or “return to learn.”21, 22
Return to play
In pediatric concussion management, a conservative approach to the determination of when a concussed child may return to play (RTP) is key. RTP decisions are guided by the resolution of the child’s symptoms and are based on clinical judgment.3-5
Current guidelines outline a gradual, stepwise approach to RTP after full recovery, which must be individualized and age-appropriate.3,5 These include
• Light aerobic exercise: Increase heart rate to 70% maximum predicted by walking, swimming, or using stationary bike. No resistance training.
• Sport-specific exercise: Add movement with skating or running drills. No head impact activities.
• Noncontact training drills: Add exercise, coordination, and cognitive load with progression to more complex training drills (eg, passing drills in football and ice hockey). May introduce progressive resistance training.
• Full contact practice: To restore confidence and allow coaching staff to assess functional skills, permit participation in normal training activities after obtaining medical clearance.
At any step, if symptoms develop with activity, the process is stopped and, after a 24-hour period of rest, is restarted at the previous symptom-free step.3,5
The goal of this approach is to ensure that the pediatric brain recovers fully and can resume normal developmental acquisition of cognitive skills and functions. Further, as previously noted, children and adolescents require more time to recover from the effects of a concussion than adults do.2,3 If a child returns too quickly to activity postconcussion, clinical evidence suggests that worsening of cognitive deficits is likely.9 Therefore, cautious postconcussion management that allows sufficient recovery time before clearance is given for a return to sports participation is highly recommended.2,4,5 No child should RTP unless cleared by a health care provider trained in the evaluation and management of pediatric concussive injuries.4,5,15
Return to school
Inadequate knowledge of concussion on the part of parents, teachers, and school officials can be a barrier to appropriate return-to-school decisions after pediatric concussive injuries.22 Since pre–high-school-age children spend the majority of their time in school, it is essential that a child’s school attendance and workload demands be decreased during recovery from a concussion.
Evidence indicates that an increase in cognitive or physical activity before complete recovery—ie, before normal brain cellular function is restored—may prolong cognitive dysfunction.5 Arbogast et al found that, in many pediatric concussion patients, unresolved symptoms impeded learning and school-based functioning: 10% to 18% of the children studied experienced fatigue, difficulty concentrating, feeling foggy, and/or vision problems.21 Within the first two weeks postinjury, 80% reported an increase in symptom severity while at school.
Academic demands should be increased gradually, with adjustments made for the individual student as needed, in order to avoid the exacerbation of such school-setting symptoms as headache, dizziness, light and/or noise sensitivity, and difficulty concentrating or remembering.22
While RTP guidelines are widely understood and implemented by clinicians, one survey found that return-to-school guidance is provided less often.21 Clinicians should be mindful of the importance of both physical rest and cognitive rest during recovery from pediatric concussion and should provide parents with clear guidance for both.21
On the next page: Role of the primary care clinician >>
THE ROLE OF THE PRIMARY CARE CLINICIAN
Primary care clinicians are central to pediatric concussion management because they facilitate and oversee a child’s recovery. They may administer neuropsychologic testing, monitor symptom resolution, and supervise the concussed child’s gradual return to physical and academic activities through the individualized phases of RTP and return-to-school protocols.4,20,23
The NP or PA functions as the main point of contact within the heath care team, organizing the plan of care and coordinating with parents, teachers, and coaches throughout the recovery process. Close follow-up care, including detailed documentation, should take place at well-child examinations to help ensure that the child’s development continues to progress as expected.
Referrals
Although referrals to a specialist are not typically necessary, persistent symptoms—those lasting longer than 10 days and not usually specific to concussion—warrant immediate and appropriate referral.3,22 Approximately 30% of mTBI patients experience long-term, often significant aftereffects, underscoring that mTBI is not a single entity and that each patient is unique.24
Risk factors for protracted symptoms
Factors that may be associated with prolonged or persistent duration of symptoms include early posttraumatic headache, previous concussion, early amnesia, alteration in mental status, disorientation, fatigue/fogginess, developmental disorders (eg, learning disabilities, ADHD), and psychiatric disorders (eg, anxiety, depression).4,13 Studies have examined this association, and there is conflicting evidence as to whether prolonged symptoms are attributed to, or are a combination of, preconcussion modifying factors, concussive episode severity, and/or coexistent pathologies.3,4
Concussion complications
Postconcussion syndrome can occur in pediatric athletes after a single concussion.3,23 The syndrome is not clearly understood but is characterized by the persistence of multiple cognitive, physical, and/or emotional symptoms of a concussion for weeks or even months, making it difficult to both diagnose and manage.5,15
Second impact syndrome, only documented in pediatric athletes, occurs when a child sustains a concussion before fully recovering from a prior concussion. This can lead to cerebral vascular congestion, cerebral swelling, and in some cases, death.15 Immediate removal of a concussed child from play until completely asymptomatic is obviously essential to the prevention of this rare catastrophe.
Any child with persistent symptoms should be referred to a multidisciplinary team of providers experienced in concussion management. This team may include, but is not limited to, neurologists, developmental pediatricians, concussion specialists, and psychologic, cognitive, and/or physical therapists.3,5
CONCUSSION EDUCATION
Family
Family-centered education is another essential component of pediatric concussion management. Parents and guardians are extremely influential and important to a child’s overall recovery, especially a younger child’s. While older pre–high-school-age children are much more capable of self-reporting symptoms, the younger child may not yet be developmentally able to do so, making the parent or guardian’s assistance and input essential.14
Unfortunately, studies have shown that a significant number of parents lack a good understanding of what constitutes a concussion as well as of the appropriate steps to ensure their child’s safe return to sport and school.22,25 Many parents view concussion as meaning a less severe head injury than if mild TBI or minor TBI is used.26 It is imperative that clinicians ensure that parents understand the seriousness of their child’s concussive injury and how to judge when their child may safely return to school.
GAAME is an acronym for a simple concussion action plan for parents of young sports participants. The name is based on the first word of each step in the plan:
Get out, Assess, Ask, Medical attention, and Emergency situation.
The GAAME handout (see "Parent Guide") briefly explains the steps to take if a child experiences a blow to the head during a sports activity. It can be given to parents of all pre–high-schoolers, whether their children participate in organized sports or not.
GAAME utilizes a five-step approach that immediately pulls the child out of the game and highlights the important information a clinician will need when the child receives medical attention.3 Parents, guardians, and other involved parties serve as a child’s best advocate by being informed and alert to the early signs and symptoms of a concussion and by helping the child to identify his or her own symptoms.
School personnel
Teachers and other school officials must recognize both the necessity of cognitive rest during concussion recovery and their role in enabling a child’s gradual return to the cognitive demands of school. A child may require such adjustments as a shorter school day or week, a reduced workload, and extra time for tests to avoid exacerbation of concussion symptoms.5,22 In light of state concussion laws (see below), schools commonly ensure that personnel are well-informed about concussion and its aftereffects in the classroom.
Sports officials
Heightened awareness of the need for more effective concussion education and management in youth sports has led to enactment of laws on youth sports-related concussions in all 50 states and the District of Columbia.27 Most of these laws include
1. Inform and educate coaches, athletes, and their parents and guardians about concussion through training and/or a concussion information sheet.
2. An athlete who is believed to have a concussion is to be removed from play right away.
3. An athlete can only return to play or practice after at least 24 hours and with permission from a health care professional.
Clinicians should also be familiar with the laws in their states as they may affect clinical decisions (eg, timing of RTP protocol).
On the next page: Conclusion >>
CONCLUSION
Optimal management of pediatric concussions is a multifaceted challenge that is best addressed by age-appropriate, individualized patient care. Educational initiatives based on the latest concussion guidelines will increase awareness of appropriate concussion management by all involved in overseeing the recovery of the pre-high-school-age child.
A greater understanding of concussion, coupled with management based on current, standardized RTP and return-to-school protocols, will enhance coordination among the multidisciplinary team overseeing the child’s recovery and facilitate the return to full preconcussion functioning. More research about the effects of concussion on the developing brain is needed in order to create evidence-based guidelines specific to this pediatric population.
1. Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths, 2002-2006. www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf. Accessed August 14, 2014.
2. Meehan WP, Taylor AM, Proctor M. The pediatric athlete: younger athletes with sports-related concussion. Clin Sports Med. 2011;30(1):1-11.
3. McCrory P, Meeuwisse WH, Aubry M, et al; Concussion in Sport Group. Consensus statement on concussion in sport: the 4th International Consensus Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250-258.
4. Giza CC, Kutcher JS, Ashwal S, et al; Guideline Development Subcommittee, American Academy of Neurology. Summary of evidence-based guideline update: evaluation and management of concussion in sports. Neurology. 2013;80(24):2250-2257.
5. Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15-26.
6. Chrisman SP, Schiff MA, Rivara FP. Physician concussion knowledge and effect of mailing the CDC “heads up” toolkit. Clin Pediatr. 2011;50(11):1031-1039.
7. Graham R, Rivara FP, Ford MA, Spicer CM, eds. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington, DC: The National Academies Press; 2014.
8. Khurana VG, Kaye AH. An overview of concussion in sport. J Clin Neurosci. 2012;19(1):1-11.
9. Toledo E, Lebel A, Becerra L, et al. The young brain and concussion: imaging as a biomarker for diagnosis and prognosis. Neurosci Biobehav Rev. 2012;36(6):1510-1531.
10. Maugans TA, Farley C, Altaye M, et al. Pediatric sports-related concussion produces cerebral blood flow alterations. Pediatrics. 2012;129(1):28-37.
11. Franklin CC, Weiss JM. Stopping sports injuries in kids: an overview of the last year in publications. Curr Opin Pediatr. 2012;24(1):64-67.
12. Cernak I, Chang T, Ahmed FA, et al. Pathophysiological response to experimental diffuse brain trauma differs as a function of developmental age. Dev Neurosci. 2012;32(5-6):442-453.
13. Gioia GA, Collins M, Isquith PK. Improving identification and diagnosis of mild traumatic brain injury with evidence: psychometric support for the acute concussion evaluation. J Head Trauma Rehabil. 2008;23(4):230-242.
14. Echemendia RJ, Iverson G, McCrea M, et al. Advances in neuropsychological assessment of sport-related concussion. Br J Sports Med. 2013;47(5):294-298.
15. Halstead M, Walter D. Clinical report: sports-related concussion in children and adolescents. Pediatrics. 2010;126(3):597-615.
16. Gomez JE, Hergenroeder AC. New guidelines for management of concussion in sport: special concern for youth. J Adolesc Health. 2013;53(3):311-313.
17. Grubenhoff JA, Kirkwood M, Gao D, et al. Evaluation of standardized assessment of concussion in a pediatric emergency department. Pediatrics. 2010;126(4):688-694.
18. Fung M, Willer B, Moreland D, Leddy J. A proposal for an evidence-based emergency department discharge form for mild traumatic brain injury. Brain Inj. 2006;20(9):889-994.
19. Apps JN, Walter KD. Pediatric and Adolescent Concussion: Diagnosis, Management, and Outcomes. New York: Springer Science+Business Media, LLC; 2012. http://midnurse.umsha.ac.ir/uploads/Pediatric&Adolescent_Concus sion.pdf. Accessed August 14, 2014.
20. Kirkwood MW, Yeates KO, Wilson PE. Pediatric sports-related concussion: a review of the clinical management of an oft-neglected population in children and adolescents. Pediatrics. 2006;117(4):1359-1371.
21. Arbogast KB, McGinley AD, Master CL, et al. Cognitive rest and school-based recommendations following pediatric concussion: the need for primary support tools. Clin Pediatr. 2013;452(5):397-402.
22. Halstead ME, McAvoy K, Devore CD, et al. Returning to learning following a concussion. Pediatrics. 2013;132(5):948-957.
23. Marsh AM, Fraser D, Marsh JP. Management of concussion in the pediatric patient. J Pediatr Health Care. 2013;27(6):499-504.
24. Rosenbaum SB, Lipton ML. Embracing chaos: the scope and importance of clinical and pathological heterogeneity in MTBI. Brain Imaging Behav. 2012;6:255-282.
25. Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126(3):e550-e556.
26. Gordon KE, Dooley JM, Fitzpatrick EA, et al. Concussion or mild traumatic brain injury: parents appreciate the nuances of nosology. Pediatr Neurol. 2010;43(4):253-257.
27. CDC. Get a heads up on concussion in sports policies. www.cdc.gov/concussion/policies.html. Accessed August 14, 2014.
28. Gioia G, Collins M. Acute concussion evaluation (ACE). 2006. www.cdc.gov/concussion/headsup/pdf/ace-a.pdf. Accessed August 14, 2014.
29. ImPACT Applications Inc. ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing). www.impacttest.com/about/?Overview-1. Accessed August 14, 2014.
CE/CME No: CR-1409
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Define the term concussion.
• Identify the major signs and symptoms of a concussion.
• Discuss the initial management of a pediatric patient with a suspected sports-related concussion.
• Describe the current recommendations for return to play after a pediatric concussion.
• Explain the main challenges clinicians face in the management of pediatric concussions
FACULTY
Sydney Meckler is pursuing her Doctor of Nursing Practice degree at Columbia University, New York City. The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
This article describes the challenges of diagnosis and treatment of pediatric concussive injuries, with particular attention to the effects of concussion on the developing brain. It highlights the need for individualized, age-dependent care; standardized return-to-play and return-to-school protocols; and better-informed clinicians, parents, teachers, and coaches.
Pediatric concussions—those occurring in children younger than 18—account for almost half a million emergency department visits each year.1 Of these, more than 25% occur during sports-related activities.2 Yet it is believed that pediatric concussive injuries are significantly underreported because parents do not always seek medical attention for their concussed children and because little has been published on the management of sports-related concussions in pre–high-school-age athletes.2
The 4th International Consensus Conference on Concussion in Sport, the American Academy of Neurology, and the American Medical Society for Sports Medicine all recently updated their guidelines for concussion evaluation and management.3-5 However, the lack of data on concussions in younger pediatric athletes presents challenges for the optimal management of these patients.6 In fact, in a February 2014 report, the Institute of Medicine said that more research is needed to develop evidence-based sports-related concussion management guidelines for children and adolescents.7
In this article, the factors that distinguish concussions in children from those in adults will be described, as will the management techniques that primary care clinicians can use to effectively address them.
WHAT IS A CONCUSSION?
Although the term concussion has been used interchangeably with head trauma and brain injury, concussion is most often described as mild traumatic brain injury (mTBI). Variations in terminology reflect both the lack of agreement on a standard definition for concussion, especially as it applies to the pediatric population, and the complexities of concussion diagnosis and management.8 This inherent ambiguity can lead to suboptimal recognition and awareness of concussion among clinicians, patients, families, school personnel, and sports staff, especially of its serious aftereffects in the pediatric patient.
A blow to the head can propel the brain to strike one side of the skull and then bounce off the opposite side. This can damage or tear the axons—the signal transmitters of the neurons—from their cell bodies, disrupting brain cell communications and causing neurocognitive deficits.
While a concussion is a direct injury to the brain, it is also an evolving process comprised of several pathophysiologic components that are a consequence of biomechanical forces. The brain does not directly contact the skull but is surrounded by cerebrospinal fluid and fluid-filled vessels with a greater density than the brain itself. This intracranial space provides room for the brain to move upon impact by shifting and compressing from one side of the skull to the other.9 The concussive injury occurs as a result of either a direct strike to the head or from an indirect force traumatic enough to be transmitted to the brain. The strike or force produces a complex disturbance to the brain that, in most cases, does not result in loss of consciousness.3
THE GREATER VULNERABILITY OF THE PEDIATRIC BRAIN
Pathophysiology
For a concussion to occur, the biomechanical threshold at which nerve cells' adaptability is impeded must be crossed.10 This sets in motion a cascade of events, developing over minutes, hours, and even days, in which homeostasis is disrupted due to an imbalance of ionic, neuronal, metabolic, and pathophysiologic processes.5
While many studies have sought to explain the pathophysiology of pediatric sports-related concussions, much is still unknown. One hypothesis suggests that, after the injury, neuronal depolarization occurs, releasing excitatory neurotransmitters and altering metabolism by the immediate release of potassium. Restoration of homeostasis demands response by the sodium-potassium pump, requiring energy in the form of glucose. Coupled with axonal injury and alterations in cerebral blood flow, an imbalance between energy supply and demand occurs.5
Maugans et al found that a single pediatric concussion does not cause a structural or metabolic injury but instead a physiologic interruption—different from what occurs in adult concussions.10 They observed a statistically significant reduction in cerebral blood flow of more than 10% in a small group of postconcussion children, ages 11 to 15, compared with a control group. This alteration persisted for two weeks in two-thirds of the children and for up to a month in the remaining third.10 The delayed return of normal cerebral blood flow is believed to be a major contributing factor to pediatric concussion-related symptoms. However, little is known about the long-term effects of concussion on the developing brain.9
Crucial developmental years
Because the pediatric brain is still developing, children between the ages of 5 and 12 are at greater risk for sustaining a disruption in brain function from a concussion. In addition, this group is more susceptible in general to sports injuries compared to adults, because of their stage of growth and development.11
With a pediatric concussion, the individual child’s stage of brain development and the possible effects on his or her evolving neurocognitive functioning must be taken into account. Critical skills, such as language, emotion, memory, problem solving, and motor dexterity, emerge during childhood, and a disturbance during this time could have substantial consequences.12 Motor skills and primary senses usually mature by age 5, with language maturity occurring by age 10.9 However, many other vital skills and processes, such as emotion, judgment, and abstract reasoning, are not fully developed until adulthood. As a result, damage to cortical areas of the brain, such as the parietal lobe and frontal areas—involved in fine motor skills and complex thinking—can hinder or delay the development of these necessary processes.9
Many researchers suggest that, while a concussion to the developing brain may not significantly affect previously learned functions, it may notably delay development of new cognitive functions. As a result, recovery from a concussion during these years may be poorer.2,9,12
On the next page: Clinical presentation and post injury evaluation >>
CLINICAL PRESENTATION
Initial assessment of pediatric athletes with suspected concussive injuries can be particularly challenging because of the variability and evolving nature of associated signs and symptoms, resulting in a wide range of clinical presentations.3 These presenting signs and symptoms can, however, provide vital clues to the location of the injury within the brain because the consequences of concussion arise from injury to the brain’s cortical and subcortical systems (see Table 1).9
The cortical systems are located within the frontal, temporal, parietal, and occipital lobes, each of which houses control centers for specific learned skills and functions. The subcortical systems include the hypothalamus, trigeminal system, basal ganglia, and cerebellum. While a concussion most often causes diffuse harm rather than localized trauma, familiarity with the functions associated with specific brain locations aids in initial identification of the injury and allows for individualized concussion management.13
After a concussion occurs, it is essential to evaluate all domains of the child’s functioning through a comprehensive physical assessment, including a detailed concussion history and review of preinjury risk factors.3 In addition, there may be unobservable symptoms about which a child is unable to communicate due to his or her stage of emotional and cognitive development and restricted capacity to serve as a primary reporter.14
Signs and symptoms
The four categories of concussion signs and symptoms include physical, cognitive, emotional, and sleep (see Table 2).15 A concussed patient may experience any variation or combination of these signs and symptoms.
It is important to recognize that, although loss of consciousness is a serious sign of a concussion, it occurs in only about 10% of concussive injuries.5,15 In fact, current concussion guidelines no longer advocate the use of grading scales, which assessed the severity of a concussion based primarily on the presence or absence of a brief loss of consciousness. Evidence now shows that loss of consciousness does not predict clinical course or cognitive long-term impairment after a concussion.16
Duration of symptoms
The duration of concussion symptoms can vary, but in most cases symptoms last seven to 10 days, with 10% to 15% of patients reporting symptoms for more than 10 days.3,5 While recovery duration has not been studied sufficiently in children younger than 15, younger children require longer recovery periods. The resolution of symptoms, however, does not necessarily correlate with absolute cognitive recovery.5,17
Modifying and complicating factors
In addition to the patient’s presenting signs and symptoms, factors that may modify or complicate recovery from a concussion should be identified (see Table 3).3 These factors include preexisting conditions or disorders and the use of certain prescription drugs. Each factor should be assessed individually, taking into account the patient’s age.2
Some presenting symptoms may overlap with symptoms of common disorders in this group. It is important to note if symptoms of such conditions as attention-deficit/hyperactivity disorder (ADHD), sleep disorders, learning disabilities, and mood disorders were present prior to the concussion.5
Modifying factors provide essential information that can help predict the individual patient’s anticipated recovery process and must be taken into account throughout the process. They are particularly important when assessing the differences between a child’s preconcussion and postconcussion functioning.3,4
POST INJURY EVALUATION OF COGNITIVE FUNCTIONING
Concussion is diagnosed clinically, based on the mechanism of the sustained injury, and is supported primarily by reported and observed signs and symptoms. The ability to systematically evaluate the patient for manifestations of concussion is essential to pediatric concussion management.3,18
To aid in appropriately evaluating symptoms and assessing functional damage, many standardized assessment tools and neuropsychological tests have been developed. These tools have been modified for younger athletes due to differences in children’s neurocognitive development and in their ability to be symptom self-reporters.
Concussion assessment tools
The tools most commonly used to assess the effects of concussion in younger athletes are listed in Table 4. It was not until 2012, with the release of the Child Sport Concussion Assessment Tool Version 3 (Child-SCAT3), that an appropriately adapted and valid concussion assessment tool became available for children younger than 10.3
Assessment tools are useful but are not diagnostic. They do not take the place of a clinician’s thorough neurocognitive evaluation of a potentially concussed child.
Neuropsychologic testing
In order to properly manage pediatric concussions, postconcussion status must be assessed relative to preconcussion status in order to ensure optimal resolution of symptoms and cognitive recovery.19
The American Medical Society for Sports Medicine supports baseline testing for high-risk athletes, defined as those with a prior history of concussions or “confounding” conditions (learning disability, mood and attention disorders, migraine headaches).5 The International Consensus Statement on Concussion in Sport states that there is insufficient evidence to recommend routine baseline testing, but its early use after pediatric concussion may provide helpful information for determining when the child may return to school. The American Academy of Neurology suggests that clinicians “… might utilize baseline scores on concussion assessment tools, especially in younger athletes, those with prior concussions, or those with preexisting learning disabilities/ADHD, as doing so fosters better interpretation of postinjury scores.”4
Assessment tools can provide essential insight into the cognitive functional state of a concussed child athlete, even after symptom resolution.3,5,20 They are not stand-alone measures of recovery but can be useful components of the pediatric concussion evaluation and management process and an aid to clinical decision making.3,13
Paper-and-pencil or computerized neuropsychologic tests provide objective measures of brain-behavior relationships and are more sensitive in detecting subtle cognitive impairments than a clinical examination.5 Although neuropsychologic testing has not been validated as a diagnostic tool, it may be useful for both baseline (preinjury) testing of athletes and for monitoring recovery from a concussive event.5,20 (For more information on motor control assessment, see Dirks RP, McLeod TCV. Sport-related mild traumatic brain injury. Clinician Reviews. 2008;18[9]:22. http://bit.ly/1mjizIa.)
On the next page: Postconcussion management >>
POSTCONCUSSION MANAGEMENT
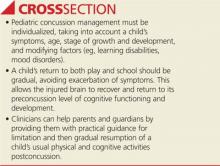
All concussion management guidelines concur that immediate removal from play of a pediatric athlete with a suspected concussion is the most important initial action. Regardless of how short the duration or mild the symptoms may be, same-day return to play should never occur.3-5 This is particularly true because acute concussion is an evolving injury and manifestation of symptoms, including cognitive deficits, is often delayed.3
The foundation of postconcussion recovery is rest, both physical and cognitive. Acute symptoms must diminish before a gradual resumption of activities.3,5
Cognitive rest
Cognitive rest is the cornerstone of concussion management.5 The latest guidelines stress the importance, particularly in the pediatric age-group, of decreasing any activities of daily living that may aggravate symptoms.3 This includes such common childhood pastimes as playing video games, watching television, and using a computer.15 More important, cognitive rest means academic rest, which is essential to postconcussion recovery and preparing the child for a “return to school” or “return to learn.”21, 22
Return to play
In pediatric concussion management, a conservative approach to the determination of when a concussed child may return to play (RTP) is key. RTP decisions are guided by the resolution of the child’s symptoms and are based on clinical judgment.3-5
Current guidelines outline a gradual, stepwise approach to RTP after full recovery, which must be individualized and age-appropriate.3,5 These include
• Light aerobic exercise: Increase heart rate to 70% maximum predicted by walking, swimming, or using stationary bike. No resistance training.
• Sport-specific exercise: Add movement with skating or running drills. No head impact activities.
• Noncontact training drills: Add exercise, coordination, and cognitive load with progression to more complex training drills (eg, passing drills in football and ice hockey). May introduce progressive resistance training.
• Full contact practice: To restore confidence and allow coaching staff to assess functional skills, permit participation in normal training activities after obtaining medical clearance.
At any step, if symptoms develop with activity, the process is stopped and, after a 24-hour period of rest, is restarted at the previous symptom-free step.3,5
The goal of this approach is to ensure that the pediatric brain recovers fully and can resume normal developmental acquisition of cognitive skills and functions. Further, as previously noted, children and adolescents require more time to recover from the effects of a concussion than adults do.2,3 If a child returns too quickly to activity postconcussion, clinical evidence suggests that worsening of cognitive deficits is likely.9 Therefore, cautious postconcussion management that allows sufficient recovery time before clearance is given for a return to sports participation is highly recommended.2,4,5 No child should RTP unless cleared by a health care provider trained in the evaluation and management of pediatric concussive injuries.4,5,15
Return to school
Inadequate knowledge of concussion on the part of parents, teachers, and school officials can be a barrier to appropriate return-to-school decisions after pediatric concussive injuries.22 Since pre–high-school-age children spend the majority of their time in school, it is essential that a child’s school attendance and workload demands be decreased during recovery from a concussion.
Evidence indicates that an increase in cognitive or physical activity before complete recovery—ie, before normal brain cellular function is restored—may prolong cognitive dysfunction.5 Arbogast et al found that, in many pediatric concussion patients, unresolved symptoms impeded learning and school-based functioning: 10% to 18% of the children studied experienced fatigue, difficulty concentrating, feeling foggy, and/or vision problems.21 Within the first two weeks postinjury, 80% reported an increase in symptom severity while at school.
Academic demands should be increased gradually, with adjustments made for the individual student as needed, in order to avoid the exacerbation of such school-setting symptoms as headache, dizziness, light and/or noise sensitivity, and difficulty concentrating or remembering.22
While RTP guidelines are widely understood and implemented by clinicians, one survey found that return-to-school guidance is provided less often.21 Clinicians should be mindful of the importance of both physical rest and cognitive rest during recovery from pediatric concussion and should provide parents with clear guidance for both.21
On the next page: Role of the primary care clinician >>
THE ROLE OF THE PRIMARY CARE CLINICIAN
Primary care clinicians are central to pediatric concussion management because they facilitate and oversee a child’s recovery. They may administer neuropsychologic testing, monitor symptom resolution, and supervise the concussed child’s gradual return to physical and academic activities through the individualized phases of RTP and return-to-school protocols.4,20,23
The NP or PA functions as the main point of contact within the heath care team, organizing the plan of care and coordinating with parents, teachers, and coaches throughout the recovery process. Close follow-up care, including detailed documentation, should take place at well-child examinations to help ensure that the child’s development continues to progress as expected.
Referrals
Although referrals to a specialist are not typically necessary, persistent symptoms—those lasting longer than 10 days and not usually specific to concussion—warrant immediate and appropriate referral.3,22 Approximately 30% of mTBI patients experience long-term, often significant aftereffects, underscoring that mTBI is not a single entity and that each patient is unique.24
Risk factors for protracted symptoms
Factors that may be associated with prolonged or persistent duration of symptoms include early posttraumatic headache, previous concussion, early amnesia, alteration in mental status, disorientation, fatigue/fogginess, developmental disorders (eg, learning disabilities, ADHD), and psychiatric disorders (eg, anxiety, depression).4,13 Studies have examined this association, and there is conflicting evidence as to whether prolonged symptoms are attributed to, or are a combination of, preconcussion modifying factors, concussive episode severity, and/or coexistent pathologies.3,4
Concussion complications
Postconcussion syndrome can occur in pediatric athletes after a single concussion.3,23 The syndrome is not clearly understood but is characterized by the persistence of multiple cognitive, physical, and/or emotional symptoms of a concussion for weeks or even months, making it difficult to both diagnose and manage.5,15
Second impact syndrome, only documented in pediatric athletes, occurs when a child sustains a concussion before fully recovering from a prior concussion. This can lead to cerebral vascular congestion, cerebral swelling, and in some cases, death.15 Immediate removal of a concussed child from play until completely asymptomatic is obviously essential to the prevention of this rare catastrophe.
Any child with persistent symptoms should be referred to a multidisciplinary team of providers experienced in concussion management. This team may include, but is not limited to, neurologists, developmental pediatricians, concussion specialists, and psychologic, cognitive, and/or physical therapists.3,5
CONCUSSION EDUCATION
Family
Family-centered education is another essential component of pediatric concussion management. Parents and guardians are extremely influential and important to a child’s overall recovery, especially a younger child’s. While older pre–high-school-age children are much more capable of self-reporting symptoms, the younger child may not yet be developmentally able to do so, making the parent or guardian’s assistance and input essential.14
Unfortunately, studies have shown that a significant number of parents lack a good understanding of what constitutes a concussion as well as of the appropriate steps to ensure their child’s safe return to sport and school.22,25 Many parents view concussion as meaning a less severe head injury than if mild TBI or minor TBI is used.26 It is imperative that clinicians ensure that parents understand the seriousness of their child’s concussive injury and how to judge when their child may safely return to school.
GAAME is an acronym for a simple concussion action plan for parents of young sports participants. The name is based on the first word of each step in the plan:
Get out, Assess, Ask, Medical attention, and Emergency situation.
The GAAME handout (see "Parent Guide") briefly explains the steps to take if a child experiences a blow to the head during a sports activity. It can be given to parents of all pre–high-schoolers, whether their children participate in organized sports or not.
GAAME utilizes a five-step approach that immediately pulls the child out of the game and highlights the important information a clinician will need when the child receives medical attention.3 Parents, guardians, and other involved parties serve as a child’s best advocate by being informed and alert to the early signs and symptoms of a concussion and by helping the child to identify his or her own symptoms.
School personnel
Teachers and other school officials must recognize both the necessity of cognitive rest during concussion recovery and their role in enabling a child’s gradual return to the cognitive demands of school. A child may require such adjustments as a shorter school day or week, a reduced workload, and extra time for tests to avoid exacerbation of concussion symptoms.5,22 In light of state concussion laws (see below), schools commonly ensure that personnel are well-informed about concussion and its aftereffects in the classroom.
Sports officials
Heightened awareness of the need for more effective concussion education and management in youth sports has led to enactment of laws on youth sports-related concussions in all 50 states and the District of Columbia.27 Most of these laws include
1. Inform and educate coaches, athletes, and their parents and guardians about concussion through training and/or a concussion information sheet.
2. An athlete who is believed to have a concussion is to be removed from play right away.
3. An athlete can only return to play or practice after at least 24 hours and with permission from a health care professional.
Clinicians should also be familiar with the laws in their states as they may affect clinical decisions (eg, timing of RTP protocol).
On the next page: Conclusion >>
CONCLUSION
Optimal management of pediatric concussions is a multifaceted challenge that is best addressed by age-appropriate, individualized patient care. Educational initiatives based on the latest concussion guidelines will increase awareness of appropriate concussion management by all involved in overseeing the recovery of the pre-high-school-age child.
A greater understanding of concussion, coupled with management based on current, standardized RTP and return-to-school protocols, will enhance coordination among the multidisciplinary team overseeing the child’s recovery and facilitate the return to full preconcussion functioning. More research about the effects of concussion on the developing brain is needed in order to create evidence-based guidelines specific to this pediatric population.
CE/CME No: CR-1409
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Define the term concussion.
• Identify the major signs and symptoms of a concussion.
• Discuss the initial management of a pediatric patient with a suspected sports-related concussion.
• Describe the current recommendations for return to play after a pediatric concussion.
• Explain the main challenges clinicians face in the management of pediatric concussions
FACULTY
Sydney Meckler is pursuing her Doctor of Nursing Practice degree at Columbia University, New York City. The author has no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
This article describes the challenges of diagnosis and treatment of pediatric concussive injuries, with particular attention to the effects of concussion on the developing brain. It highlights the need for individualized, age-dependent care; standardized return-to-play and return-to-school protocols; and better-informed clinicians, parents, teachers, and coaches.
Pediatric concussions—those occurring in children younger than 18—account for almost half a million emergency department visits each year.1 Of these, more than 25% occur during sports-related activities.2 Yet it is believed that pediatric concussive injuries are significantly underreported because parents do not always seek medical attention for their concussed children and because little has been published on the management of sports-related concussions in pre–high-school-age athletes.2
The 4th International Consensus Conference on Concussion in Sport, the American Academy of Neurology, and the American Medical Society for Sports Medicine all recently updated their guidelines for concussion evaluation and management.3-5 However, the lack of data on concussions in younger pediatric athletes presents challenges for the optimal management of these patients.6 In fact, in a February 2014 report, the Institute of Medicine said that more research is needed to develop evidence-based sports-related concussion management guidelines for children and adolescents.7
In this article, the factors that distinguish concussions in children from those in adults will be described, as will the management techniques that primary care clinicians can use to effectively address them.
WHAT IS A CONCUSSION?
Although the term concussion has been used interchangeably with head trauma and brain injury, concussion is most often described as mild traumatic brain injury (mTBI). Variations in terminology reflect both the lack of agreement on a standard definition for concussion, especially as it applies to the pediatric population, and the complexities of concussion diagnosis and management.8 This inherent ambiguity can lead to suboptimal recognition and awareness of concussion among clinicians, patients, families, school personnel, and sports staff, especially of its serious aftereffects in the pediatric patient.
A blow to the head can propel the brain to strike one side of the skull and then bounce off the opposite side. This can damage or tear the axons—the signal transmitters of the neurons—from their cell bodies, disrupting brain cell communications and causing neurocognitive deficits.
While a concussion is a direct injury to the brain, it is also an evolving process comprised of several pathophysiologic components that are a consequence of biomechanical forces. The brain does not directly contact the skull but is surrounded by cerebrospinal fluid and fluid-filled vessels with a greater density than the brain itself. This intracranial space provides room for the brain to move upon impact by shifting and compressing from one side of the skull to the other.9 The concussive injury occurs as a result of either a direct strike to the head or from an indirect force traumatic enough to be transmitted to the brain. The strike or force produces a complex disturbance to the brain that, in most cases, does not result in loss of consciousness.3
THE GREATER VULNERABILITY OF THE PEDIATRIC BRAIN
Pathophysiology
For a concussion to occur, the biomechanical threshold at which nerve cells' adaptability is impeded must be crossed.10 This sets in motion a cascade of events, developing over minutes, hours, and even days, in which homeostasis is disrupted due to an imbalance of ionic, neuronal, metabolic, and pathophysiologic processes.5
While many studies have sought to explain the pathophysiology of pediatric sports-related concussions, much is still unknown. One hypothesis suggests that, after the injury, neuronal depolarization occurs, releasing excitatory neurotransmitters and altering metabolism by the immediate release of potassium. Restoration of homeostasis demands response by the sodium-potassium pump, requiring energy in the form of glucose. Coupled with axonal injury and alterations in cerebral blood flow, an imbalance between energy supply and demand occurs.5
Maugans et al found that a single pediatric concussion does not cause a structural or metabolic injury but instead a physiologic interruption—different from what occurs in adult concussions.10 They observed a statistically significant reduction in cerebral blood flow of more than 10% in a small group of postconcussion children, ages 11 to 15, compared with a control group. This alteration persisted for two weeks in two-thirds of the children and for up to a month in the remaining third.10 The delayed return of normal cerebral blood flow is believed to be a major contributing factor to pediatric concussion-related symptoms. However, little is known about the long-term effects of concussion on the developing brain.9
Crucial developmental years
Because the pediatric brain is still developing, children between the ages of 5 and 12 are at greater risk for sustaining a disruption in brain function from a concussion. In addition, this group is more susceptible in general to sports injuries compared to adults, because of their stage of growth and development.11
With a pediatric concussion, the individual child’s stage of brain development and the possible effects on his or her evolving neurocognitive functioning must be taken into account. Critical skills, such as language, emotion, memory, problem solving, and motor dexterity, emerge during childhood, and a disturbance during this time could have substantial consequences.12 Motor skills and primary senses usually mature by age 5, with language maturity occurring by age 10.9 However, many other vital skills and processes, such as emotion, judgment, and abstract reasoning, are not fully developed until adulthood. As a result, damage to cortical areas of the brain, such as the parietal lobe and frontal areas—involved in fine motor skills and complex thinking—can hinder or delay the development of these necessary processes.9
Many researchers suggest that, while a concussion to the developing brain may not significantly affect previously learned functions, it may notably delay development of new cognitive functions. As a result, recovery from a concussion during these years may be poorer.2,9,12
On the next page: Clinical presentation and post injury evaluation >>
CLINICAL PRESENTATION
Initial assessment of pediatric athletes with suspected concussive injuries can be particularly challenging because of the variability and evolving nature of associated signs and symptoms, resulting in a wide range of clinical presentations.3 These presenting signs and symptoms can, however, provide vital clues to the location of the injury within the brain because the consequences of concussion arise from injury to the brain’s cortical and subcortical systems (see Table 1).9
The cortical systems are located within the frontal, temporal, parietal, and occipital lobes, each of which houses control centers for specific learned skills and functions. The subcortical systems include the hypothalamus, trigeminal system, basal ganglia, and cerebellum. While a concussion most often causes diffuse harm rather than localized trauma, familiarity with the functions associated with specific brain locations aids in initial identification of the injury and allows for individualized concussion management.13
After a concussion occurs, it is essential to evaluate all domains of the child’s functioning through a comprehensive physical assessment, including a detailed concussion history and review of preinjury risk factors.3 In addition, there may be unobservable symptoms about which a child is unable to communicate due to his or her stage of emotional and cognitive development and restricted capacity to serve as a primary reporter.14
Signs and symptoms
The four categories of concussion signs and symptoms include physical, cognitive, emotional, and sleep (see Table 2).15 A concussed patient may experience any variation or combination of these signs and symptoms.
It is important to recognize that, although loss of consciousness is a serious sign of a concussion, it occurs in only about 10% of concussive injuries.5,15 In fact, current concussion guidelines no longer advocate the use of grading scales, which assessed the severity of a concussion based primarily on the presence or absence of a brief loss of consciousness. Evidence now shows that loss of consciousness does not predict clinical course or cognitive long-term impairment after a concussion.16
Duration of symptoms
The duration of concussion symptoms can vary, but in most cases symptoms last seven to 10 days, with 10% to 15% of patients reporting symptoms for more than 10 days.3,5 While recovery duration has not been studied sufficiently in children younger than 15, younger children require longer recovery periods. The resolution of symptoms, however, does not necessarily correlate with absolute cognitive recovery.5,17
Modifying and complicating factors
In addition to the patient’s presenting signs and symptoms, factors that may modify or complicate recovery from a concussion should be identified (see Table 3).3 These factors include preexisting conditions or disorders and the use of certain prescription drugs. Each factor should be assessed individually, taking into account the patient’s age.2
Some presenting symptoms may overlap with symptoms of common disorders in this group. It is important to note if symptoms of such conditions as attention-deficit/hyperactivity disorder (ADHD), sleep disorders, learning disabilities, and mood disorders were present prior to the concussion.5
Modifying factors provide essential information that can help predict the individual patient’s anticipated recovery process and must be taken into account throughout the process. They are particularly important when assessing the differences between a child’s preconcussion and postconcussion functioning.3,4
POST INJURY EVALUATION OF COGNITIVE FUNCTIONING
Concussion is diagnosed clinically, based on the mechanism of the sustained injury, and is supported primarily by reported and observed signs and symptoms. The ability to systematically evaluate the patient for manifestations of concussion is essential to pediatric concussion management.3,18
To aid in appropriately evaluating symptoms and assessing functional damage, many standardized assessment tools and neuropsychological tests have been developed. These tools have been modified for younger athletes due to differences in children’s neurocognitive development and in their ability to be symptom self-reporters.
Concussion assessment tools
The tools most commonly used to assess the effects of concussion in younger athletes are listed in Table 4. It was not until 2012, with the release of the Child Sport Concussion Assessment Tool Version 3 (Child-SCAT3), that an appropriately adapted and valid concussion assessment tool became available for children younger than 10.3
Assessment tools are useful but are not diagnostic. They do not take the place of a clinician’s thorough neurocognitive evaluation of a potentially concussed child.
Neuropsychologic testing
In order to properly manage pediatric concussions, postconcussion status must be assessed relative to preconcussion status in order to ensure optimal resolution of symptoms and cognitive recovery.19
The American Medical Society for Sports Medicine supports baseline testing for high-risk athletes, defined as those with a prior history of concussions or “confounding” conditions (learning disability, mood and attention disorders, migraine headaches).5 The International Consensus Statement on Concussion in Sport states that there is insufficient evidence to recommend routine baseline testing, but its early use after pediatric concussion may provide helpful information for determining when the child may return to school. The American Academy of Neurology suggests that clinicians “… might utilize baseline scores on concussion assessment tools, especially in younger athletes, those with prior concussions, or those with preexisting learning disabilities/ADHD, as doing so fosters better interpretation of postinjury scores.”4
Assessment tools can provide essential insight into the cognitive functional state of a concussed child athlete, even after symptom resolution.3,5,20 They are not stand-alone measures of recovery but can be useful components of the pediatric concussion evaluation and management process and an aid to clinical decision making.3,13
Paper-and-pencil or computerized neuropsychologic tests provide objective measures of brain-behavior relationships and are more sensitive in detecting subtle cognitive impairments than a clinical examination.5 Although neuropsychologic testing has not been validated as a diagnostic tool, it may be useful for both baseline (preinjury) testing of athletes and for monitoring recovery from a concussive event.5,20 (For more information on motor control assessment, see Dirks RP, McLeod TCV. Sport-related mild traumatic brain injury. Clinician Reviews. 2008;18[9]:22. http://bit.ly/1mjizIa.)
On the next page: Postconcussion management >>
POSTCONCUSSION MANAGEMENT
All concussion management guidelines concur that immediate removal from play of a pediatric athlete with a suspected concussion is the most important initial action. Regardless of how short the duration or mild the symptoms may be, same-day return to play should never occur.3-5 This is particularly true because acute concussion is an evolving injury and manifestation of symptoms, including cognitive deficits, is often delayed.3
The foundation of postconcussion recovery is rest, both physical and cognitive. Acute symptoms must diminish before a gradual resumption of activities.3,5
Cognitive rest
Cognitive rest is the cornerstone of concussion management.5 The latest guidelines stress the importance, particularly in the pediatric age-group, of decreasing any activities of daily living that may aggravate symptoms.3 This includes such common childhood pastimes as playing video games, watching television, and using a computer.15 More important, cognitive rest means academic rest, which is essential to postconcussion recovery and preparing the child for a “return to school” or “return to learn.”21, 22
Return to play
In pediatric concussion management, a conservative approach to the determination of when a concussed child may return to play (RTP) is key. RTP decisions are guided by the resolution of the child’s symptoms and are based on clinical judgment.3-5
Current guidelines outline a gradual, stepwise approach to RTP after full recovery, which must be individualized and age-appropriate.3,5 These include
• Light aerobic exercise: Increase heart rate to 70% maximum predicted by walking, swimming, or using stationary bike. No resistance training.
• Sport-specific exercise: Add movement with skating or running drills. No head impact activities.
• Noncontact training drills: Add exercise, coordination, and cognitive load with progression to more complex training drills (eg, passing drills in football and ice hockey). May introduce progressive resistance training.
• Full contact practice: To restore confidence and allow coaching staff to assess functional skills, permit participation in normal training activities after obtaining medical clearance.
At any step, if symptoms develop with activity, the process is stopped and, after a 24-hour period of rest, is restarted at the previous symptom-free step.3,5
The goal of this approach is to ensure that the pediatric brain recovers fully and can resume normal developmental acquisition of cognitive skills and functions. Further, as previously noted, children and adolescents require more time to recover from the effects of a concussion than adults do.2,3 If a child returns too quickly to activity postconcussion, clinical evidence suggests that worsening of cognitive deficits is likely.9 Therefore, cautious postconcussion management that allows sufficient recovery time before clearance is given for a return to sports participation is highly recommended.2,4,5 No child should RTP unless cleared by a health care provider trained in the evaluation and management of pediatric concussive injuries.4,5,15
Return to school
Inadequate knowledge of concussion on the part of parents, teachers, and school officials can be a barrier to appropriate return-to-school decisions after pediatric concussive injuries.22 Since pre–high-school-age children spend the majority of their time in school, it is essential that a child’s school attendance and workload demands be decreased during recovery from a concussion.
Evidence indicates that an increase in cognitive or physical activity before complete recovery—ie, before normal brain cellular function is restored—may prolong cognitive dysfunction.5 Arbogast et al found that, in many pediatric concussion patients, unresolved symptoms impeded learning and school-based functioning: 10% to 18% of the children studied experienced fatigue, difficulty concentrating, feeling foggy, and/or vision problems.21 Within the first two weeks postinjury, 80% reported an increase in symptom severity while at school.
Academic demands should be increased gradually, with adjustments made for the individual student as needed, in order to avoid the exacerbation of such school-setting symptoms as headache, dizziness, light and/or noise sensitivity, and difficulty concentrating or remembering.22
While RTP guidelines are widely understood and implemented by clinicians, one survey found that return-to-school guidance is provided less often.21 Clinicians should be mindful of the importance of both physical rest and cognitive rest during recovery from pediatric concussion and should provide parents with clear guidance for both.21
On the next page: Role of the primary care clinician >>
THE ROLE OF THE PRIMARY CARE CLINICIAN
Primary care clinicians are central to pediatric concussion management because they facilitate and oversee a child’s recovery. They may administer neuropsychologic testing, monitor symptom resolution, and supervise the concussed child’s gradual return to physical and academic activities through the individualized phases of RTP and return-to-school protocols.4,20,23
The NP or PA functions as the main point of contact within the heath care team, organizing the plan of care and coordinating with parents, teachers, and coaches throughout the recovery process. Close follow-up care, including detailed documentation, should take place at well-child examinations to help ensure that the child’s development continues to progress as expected.
Referrals
Although referrals to a specialist are not typically necessary, persistent symptoms—those lasting longer than 10 days and not usually specific to concussion—warrant immediate and appropriate referral.3,22 Approximately 30% of mTBI patients experience long-term, often significant aftereffects, underscoring that mTBI is not a single entity and that each patient is unique.24
Risk factors for protracted symptoms
Factors that may be associated with prolonged or persistent duration of symptoms include early posttraumatic headache, previous concussion, early amnesia, alteration in mental status, disorientation, fatigue/fogginess, developmental disorders (eg, learning disabilities, ADHD), and psychiatric disorders (eg, anxiety, depression).4,13 Studies have examined this association, and there is conflicting evidence as to whether prolonged symptoms are attributed to, or are a combination of, preconcussion modifying factors, concussive episode severity, and/or coexistent pathologies.3,4
Concussion complications
Postconcussion syndrome can occur in pediatric athletes after a single concussion.3,23 The syndrome is not clearly understood but is characterized by the persistence of multiple cognitive, physical, and/or emotional symptoms of a concussion for weeks or even months, making it difficult to both diagnose and manage.5,15
Second impact syndrome, only documented in pediatric athletes, occurs when a child sustains a concussion before fully recovering from a prior concussion. This can lead to cerebral vascular congestion, cerebral swelling, and in some cases, death.15 Immediate removal of a concussed child from play until completely asymptomatic is obviously essential to the prevention of this rare catastrophe.
Any child with persistent symptoms should be referred to a multidisciplinary team of providers experienced in concussion management. This team may include, but is not limited to, neurologists, developmental pediatricians, concussion specialists, and psychologic, cognitive, and/or physical therapists.3,5
CONCUSSION EDUCATION
Family
Family-centered education is another essential component of pediatric concussion management. Parents and guardians are extremely influential and important to a child’s overall recovery, especially a younger child’s. While older pre–high-school-age children are much more capable of self-reporting symptoms, the younger child may not yet be developmentally able to do so, making the parent or guardian’s assistance and input essential.14
Unfortunately, studies have shown that a significant number of parents lack a good understanding of what constitutes a concussion as well as of the appropriate steps to ensure their child’s safe return to sport and school.22,25 Many parents view concussion as meaning a less severe head injury than if mild TBI or minor TBI is used.26 It is imperative that clinicians ensure that parents understand the seriousness of their child’s concussive injury and how to judge when their child may safely return to school.
GAAME is an acronym for a simple concussion action plan for parents of young sports participants. The name is based on the first word of each step in the plan:
Get out, Assess, Ask, Medical attention, and Emergency situation.
The GAAME handout (see "Parent Guide") briefly explains the steps to take if a child experiences a blow to the head during a sports activity. It can be given to parents of all pre–high-schoolers, whether their children participate in organized sports or not.
GAAME utilizes a five-step approach that immediately pulls the child out of the game and highlights the important information a clinician will need when the child receives medical attention.3 Parents, guardians, and other involved parties serve as a child’s best advocate by being informed and alert to the early signs and symptoms of a concussion and by helping the child to identify his or her own symptoms.
School personnel
Teachers and other school officials must recognize both the necessity of cognitive rest during concussion recovery and their role in enabling a child’s gradual return to the cognitive demands of school. A child may require such adjustments as a shorter school day or week, a reduced workload, and extra time for tests to avoid exacerbation of concussion symptoms.5,22 In light of state concussion laws (see below), schools commonly ensure that personnel are well-informed about concussion and its aftereffects in the classroom.
Sports officials
Heightened awareness of the need for more effective concussion education and management in youth sports has led to enactment of laws on youth sports-related concussions in all 50 states and the District of Columbia.27 Most of these laws include
1. Inform and educate coaches, athletes, and their parents and guardians about concussion through training and/or a concussion information sheet.
2. An athlete who is believed to have a concussion is to be removed from play right away.
3. An athlete can only return to play or practice after at least 24 hours and with permission from a health care professional.
Clinicians should also be familiar with the laws in their states as they may affect clinical decisions (eg, timing of RTP protocol).
On the next page: Conclusion >>
CONCLUSION
Optimal management of pediatric concussions is a multifaceted challenge that is best addressed by age-appropriate, individualized patient care. Educational initiatives based on the latest concussion guidelines will increase awareness of appropriate concussion management by all involved in overseeing the recovery of the pre-high-school-age child.
A greater understanding of concussion, coupled with management based on current, standardized RTP and return-to-school protocols, will enhance coordination among the multidisciplinary team overseeing the child’s recovery and facilitate the return to full preconcussion functioning. More research about the effects of concussion on the developing brain is needed in order to create evidence-based guidelines specific to this pediatric population.
1. Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths, 2002-2006. www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf. Accessed August 14, 2014.
2. Meehan WP, Taylor AM, Proctor M. The pediatric athlete: younger athletes with sports-related concussion. Clin Sports Med. 2011;30(1):1-11.
3. McCrory P, Meeuwisse WH, Aubry M, et al; Concussion in Sport Group. Consensus statement on concussion in sport: the 4th International Consensus Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250-258.
4. Giza CC, Kutcher JS, Ashwal S, et al; Guideline Development Subcommittee, American Academy of Neurology. Summary of evidence-based guideline update: evaluation and management of concussion in sports. Neurology. 2013;80(24):2250-2257.
5. Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15-26.
6. Chrisman SP, Schiff MA, Rivara FP. Physician concussion knowledge and effect of mailing the CDC “heads up” toolkit. Clin Pediatr. 2011;50(11):1031-1039.
7. Graham R, Rivara FP, Ford MA, Spicer CM, eds. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington, DC: The National Academies Press; 2014.
8. Khurana VG, Kaye AH. An overview of concussion in sport. J Clin Neurosci. 2012;19(1):1-11.
9. Toledo E, Lebel A, Becerra L, et al. The young brain and concussion: imaging as a biomarker for diagnosis and prognosis. Neurosci Biobehav Rev. 2012;36(6):1510-1531.
10. Maugans TA, Farley C, Altaye M, et al. Pediatric sports-related concussion produces cerebral blood flow alterations. Pediatrics. 2012;129(1):28-37.
11. Franklin CC, Weiss JM. Stopping sports injuries in kids: an overview of the last year in publications. Curr Opin Pediatr. 2012;24(1):64-67.
12. Cernak I, Chang T, Ahmed FA, et al. Pathophysiological response to experimental diffuse brain trauma differs as a function of developmental age. Dev Neurosci. 2012;32(5-6):442-453.
13. Gioia GA, Collins M, Isquith PK. Improving identification and diagnosis of mild traumatic brain injury with evidence: psychometric support for the acute concussion evaluation. J Head Trauma Rehabil. 2008;23(4):230-242.
14. Echemendia RJ, Iverson G, McCrea M, et al. Advances in neuropsychological assessment of sport-related concussion. Br J Sports Med. 2013;47(5):294-298.
15. Halstead M, Walter D. Clinical report: sports-related concussion in children and adolescents. Pediatrics. 2010;126(3):597-615.
16. Gomez JE, Hergenroeder AC. New guidelines for management of concussion in sport: special concern for youth. J Adolesc Health. 2013;53(3):311-313.
17. Grubenhoff JA, Kirkwood M, Gao D, et al. Evaluation of standardized assessment of concussion in a pediatric emergency department. Pediatrics. 2010;126(4):688-694.
18. Fung M, Willer B, Moreland D, Leddy J. A proposal for an evidence-based emergency department discharge form for mild traumatic brain injury. Brain Inj. 2006;20(9):889-994.
19. Apps JN, Walter KD. Pediatric and Adolescent Concussion: Diagnosis, Management, and Outcomes. New York: Springer Science+Business Media, LLC; 2012. http://midnurse.umsha.ac.ir/uploads/Pediatric&Adolescent_Concus sion.pdf. Accessed August 14, 2014.
20. Kirkwood MW, Yeates KO, Wilson PE. Pediatric sports-related concussion: a review of the clinical management of an oft-neglected population in children and adolescents. Pediatrics. 2006;117(4):1359-1371.
21. Arbogast KB, McGinley AD, Master CL, et al. Cognitive rest and school-based recommendations following pediatric concussion: the need for primary support tools. Clin Pediatr. 2013;452(5):397-402.
22. Halstead ME, McAvoy K, Devore CD, et al. Returning to learning following a concussion. Pediatrics. 2013;132(5):948-957.
23. Marsh AM, Fraser D, Marsh JP. Management of concussion in the pediatric patient. J Pediatr Health Care. 2013;27(6):499-504.
24. Rosenbaum SB, Lipton ML. Embracing chaos: the scope and importance of clinical and pathological heterogeneity in MTBI. Brain Imaging Behav. 2012;6:255-282.
25. Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126(3):e550-e556.
26. Gordon KE, Dooley JM, Fitzpatrick EA, et al. Concussion or mild traumatic brain injury: parents appreciate the nuances of nosology. Pediatr Neurol. 2010;43(4):253-257.
27. CDC. Get a heads up on concussion in sports policies. www.cdc.gov/concussion/policies.html. Accessed August 14, 2014.
28. Gioia G, Collins M. Acute concussion evaluation (ACE). 2006. www.cdc.gov/concussion/headsup/pdf/ace-a.pdf. Accessed August 14, 2014.
29. ImPACT Applications Inc. ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing). www.impacttest.com/about/?Overview-1. Accessed August 14, 2014.
1. Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths, 2002-2006. www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf. Accessed August 14, 2014.
2. Meehan WP, Taylor AM, Proctor M. The pediatric athlete: younger athletes with sports-related concussion. Clin Sports Med. 2011;30(1):1-11.
3. McCrory P, Meeuwisse WH, Aubry M, et al; Concussion in Sport Group. Consensus statement on concussion in sport: the 4th International Consensus Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250-258.
4. Giza CC, Kutcher JS, Ashwal S, et al; Guideline Development Subcommittee, American Academy of Neurology. Summary of evidence-based guideline update: evaluation and management of concussion in sports. Neurology. 2013;80(24):2250-2257.
5. Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15-26.
6. Chrisman SP, Schiff MA, Rivara FP. Physician concussion knowledge and effect of mailing the CDC “heads up” toolkit. Clin Pediatr. 2011;50(11):1031-1039.
7. Graham R, Rivara FP, Ford MA, Spicer CM, eds. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington, DC: The National Academies Press; 2014.
8. Khurana VG, Kaye AH. An overview of concussion in sport. J Clin Neurosci. 2012;19(1):1-11.
9. Toledo E, Lebel A, Becerra L, et al. The young brain and concussion: imaging as a biomarker for diagnosis and prognosis. Neurosci Biobehav Rev. 2012;36(6):1510-1531.
10. Maugans TA, Farley C, Altaye M, et al. Pediatric sports-related concussion produces cerebral blood flow alterations. Pediatrics. 2012;129(1):28-37.
11. Franklin CC, Weiss JM. Stopping sports injuries in kids: an overview of the last year in publications. Curr Opin Pediatr. 2012;24(1):64-67.
12. Cernak I, Chang T, Ahmed FA, et al. Pathophysiological response to experimental diffuse brain trauma differs as a function of developmental age. Dev Neurosci. 2012;32(5-6):442-453.
13. Gioia GA, Collins M, Isquith PK. Improving identification and diagnosis of mild traumatic brain injury with evidence: psychometric support for the acute concussion evaluation. J Head Trauma Rehabil. 2008;23(4):230-242.
14. Echemendia RJ, Iverson G, McCrea M, et al. Advances in neuropsychological assessment of sport-related concussion. Br J Sports Med. 2013;47(5):294-298.
15. Halstead M, Walter D. Clinical report: sports-related concussion in children and adolescents. Pediatrics. 2010;126(3):597-615.
16. Gomez JE, Hergenroeder AC. New guidelines for management of concussion in sport: special concern for youth. J Adolesc Health. 2013;53(3):311-313.
17. Grubenhoff JA, Kirkwood M, Gao D, et al. Evaluation of standardized assessment of concussion in a pediatric emergency department. Pediatrics. 2010;126(4):688-694.
18. Fung M, Willer B, Moreland D, Leddy J. A proposal for an evidence-based emergency department discharge form for mild traumatic brain injury. Brain Inj. 2006;20(9):889-994.
19. Apps JN, Walter KD. Pediatric and Adolescent Concussion: Diagnosis, Management, and Outcomes. New York: Springer Science+Business Media, LLC; 2012. http://midnurse.umsha.ac.ir/uploads/Pediatric&Adolescent_Concus sion.pdf. Accessed August 14, 2014.
20. Kirkwood MW, Yeates KO, Wilson PE. Pediatric sports-related concussion: a review of the clinical management of an oft-neglected population in children and adolescents. Pediatrics. 2006;117(4):1359-1371.
21. Arbogast KB, McGinley AD, Master CL, et al. Cognitive rest and school-based recommendations following pediatric concussion: the need for primary support tools. Clin Pediatr. 2013;452(5):397-402.
22. Halstead ME, McAvoy K, Devore CD, et al. Returning to learning following a concussion. Pediatrics. 2013;132(5):948-957.
23. Marsh AM, Fraser D, Marsh JP. Management of concussion in the pediatric patient. J Pediatr Health Care. 2013;27(6):499-504.
24. Rosenbaum SB, Lipton ML. Embracing chaos: the scope and importance of clinical and pathological heterogeneity in MTBI. Brain Imaging Behav. 2012;6:255-282.
25. Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126(3):e550-e556.
26. Gordon KE, Dooley JM, Fitzpatrick EA, et al. Concussion or mild traumatic brain injury: parents appreciate the nuances of nosology. Pediatr Neurol. 2010;43(4):253-257.
27. CDC. Get a heads up on concussion in sports policies. www.cdc.gov/concussion/policies.html. Accessed August 14, 2014.
28. Gioia G, Collins M. Acute concussion evaluation (ACE). 2006. www.cdc.gov/concussion/headsup/pdf/ace-a.pdf. Accessed August 14, 2014.
29. ImPACT Applications Inc. ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing). www.impacttest.com/about/?Overview-1. Accessed August 14, 2014.