User login
The diagnosis
Answer: Hepatic foregut duplication cyst and concurrent acute gangrenous cholecystitis
References
1. Imamoglu K.H., Walt, A.J. Duplication of the duodenum extending into liver. Am J Surg. 1977;133:628-32.
2. Seidman J.D., Yale-Loehr A.J., Beaver B., et al. Alimentary duplication presenting as an hepatic cyst in a neonate. Am J Surg Pathol. 1991;15:695-8.
3. Vick D.J., Goodman Z.D., Deavers M.T., et al. Ciliated hepatic foregut cyst: A study of six cases and review of the literature. Am J Surg Pathol. 1999;23:671-7.
The diagnosis
Answer: Hepatic foregut duplication cyst and concurrent acute gangrenous cholecystitis
References
1. Imamoglu K.H., Walt, A.J. Duplication of the duodenum extending into liver. Am J Surg. 1977;133:628-32.
2. Seidman J.D., Yale-Loehr A.J., Beaver B., et al. Alimentary duplication presenting as an hepatic cyst in a neonate. Am J Surg Pathol. 1991;15:695-8.
3. Vick D.J., Goodman Z.D., Deavers M.T., et al. Ciliated hepatic foregut cyst: A study of six cases and review of the literature. Am J Surg Pathol. 1999;23:671-7.
The diagnosis
Answer: Hepatic foregut duplication cyst and concurrent acute gangrenous cholecystitis
References
1. Imamoglu K.H., Walt, A.J. Duplication of the duodenum extending into liver. Am J Surg. 1977;133:628-32.
2. Seidman J.D., Yale-Loehr A.J., Beaver B., et al. Alimentary duplication presenting as an hepatic cyst in a neonate. Am J Surg Pathol. 1991;15:695-8.
3. Vick D.J., Goodman Z.D., Deavers M.T., et al. Ciliated hepatic foregut cyst: A study of six cases and review of the literature. Am J Surg Pathol. 1999;23:671-7.
By Ryan Law, MD, Thomas C. Smyrk, and Stephen C. Hauser. Published previously in Gastroenterology (2013;144[3]:508, 658).
A 43-year-old woman presented with progressively worsening right upper-quadrant abdominal pain. The episodic pain occurred after high-fat meals and lasted from minutes to hours with accompanying nausea. Her previous medical history was notable for endometriosis. She denied other constitutional symptoms. Physical examination revealed no hepatosplenomegaly, jaundice, right upper-quadrant mass, or stigmata of chronic liver disease.
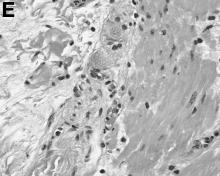
Initial laboratory evaluation yielded normal white blood cell count and liver chemistries. Ultrasonography, computed tomography, and magnetic resonance imaging of the abdomen all demonstrated a 2.0 × 4.1 × 3.9-cm, nonenhancing, elongated, cystic mass located superior to the gallbladder within the porta hepatis, with possible communication at the bile duct confluence and abutment of the right portal vein (Figure A). No definitive findings of acute cholecystitis were present.
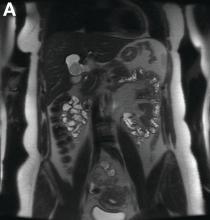
Endoscopic retrograde cholangiopancreatography with endoscopic ultrasonography was performed to further delineate the anatomy of the lesion. On endoscopic ultrasonography, the structure in question seemed to be embedded in the hepatic parenchyma with partial extension beyond the liver edge. Adherent debris was noted within the cystic structure. No lymphadenopathy was present. Cholangiography demonstrated filling of the lesion from a central right intrahepatic duct (Figure B). Attempts at cannulation of the cyst were unsuccessful.
The patient subsequently developed abnormal liver chemistries with continued right upper-quadrant pain. She was referred to an experienced hepatobiliary surgeon and underwent operative intervention. What is the diagnosis and how would you treat this patient?